GentleWave can help endodontists to achieve positive results even with complex anatomy.
Dr. Scott K. Hetz illustrates minimally invasive endodontic treatment with predictable results
Our patients are primarily concerned with two things: getting a painless procedure and knowing how long this will take. It is not often that we receive an initial inquiry about outcomes before the game even begins. Outcomes matter; in fact, that is where my mind goes every time I begin gathering diagnostic data and discovering the details about my patient’s chief complaint. Endodontics is not a game or a sport, yet we aspire to gain any advantage and win nonetheless.
Whether we like it or not, change is inevitable. New technology options will continue to evolve, allowing each of us the opportunity to be an active participant in the direction of our own practice. I was initially fascinated by the science supporting the GentleWave® Procedure (Sonendo®, Laguna Hills, California). This technology’s mechanism of action offers a different option for actively dissolving pulp tissue and removing biofilm, which are just a couple of the many advantages that I have come to rely on over the past 4 years.
In the AAE 2010 Colleagues for Excellence article, titled “Access Opening and Canal Location,” the authors wrote, “The ultimate goal of endodontic treatment is to create an environment in which the body can heal itself.”1 In other words, our job as endodontists is to clean and disinfect the root canal system as thoroughly as possible, to then allow the body’s natural healing process to take over, and to repair the damage created by either infection or inflammation, or both. Our objective then should be to minimize our “touch” to the tooth, thereby promoting lasting sustainability of the remaining structure and, ultimately, full healing.
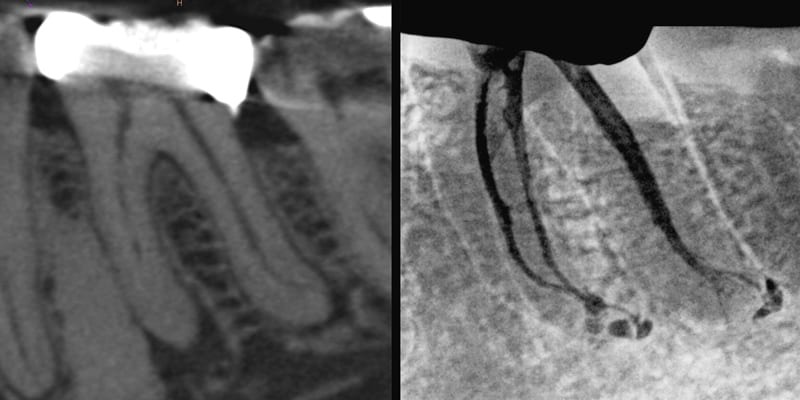
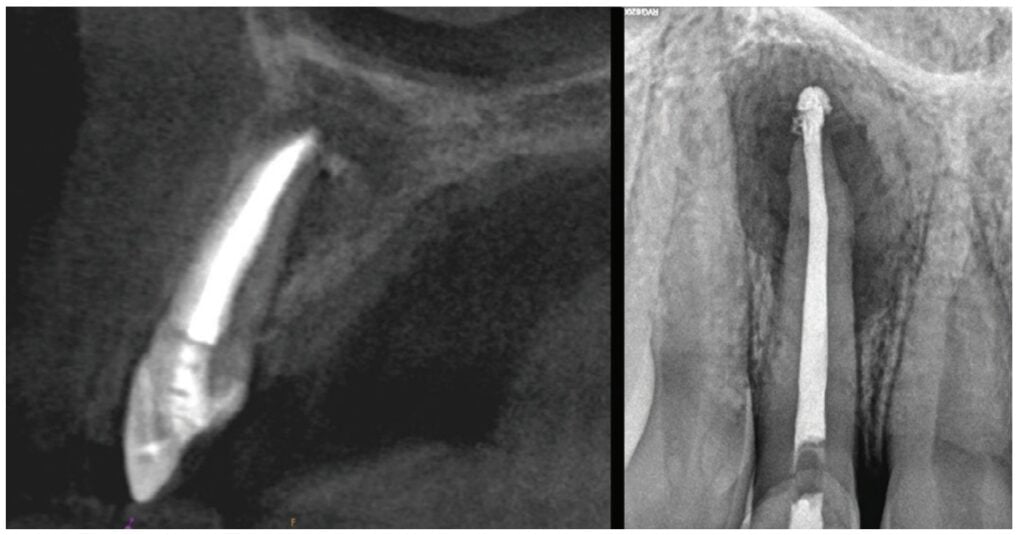
Case 1: The thrill of the clean
For many of us specialists, it is rewarding to see some of the amazing canal anatomy displayed on the final radiograph after putting all that effort into your root canal treatment — it is the “Thrill of the Fill,” as quoted by one of the masters of endodontics. However, the real game changer is the “Thrill of the Clean.” We know from the Pauli’s exclusion principle that two objects cannot occupy the same space at the same time, so you cannot fill if there is debris remaining. The GentleWave Procedure offers an option to dissolve both vital and necrotic tissues in previously inaccessible isthmus anatomy, fins, and lateral canals.
Case 1 poses a number of shaping challenges, but let us approach it from a place of opportunity. Cutting a more traditional shape for this specific anatomy would block out most of this distal apical delta and risk file separation. Shortly after adopting GentleWave, my mindset had shifted. I now ask, “How will I accommodate my approach to any case to best utilize this technology?” Instead of shaping, the new goal is to secure a minimally invasive fluid pathway to deliver the GentleWave System’s efficient and powerful mechanism of action into this complex anatomy.
Once cleaned and thoroughly dried, the root canal system can be predictably obturated with a single-cone, sealer-based technique using bioceramic sealer.
The early healing observed by most clinicians using these techniques is validated with comparative CBCT images at 3 months.
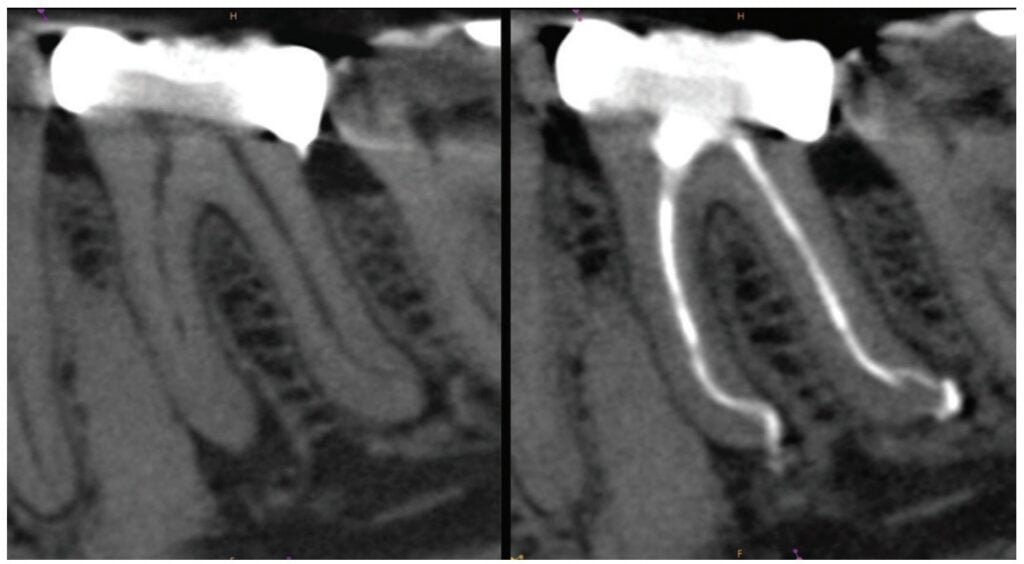
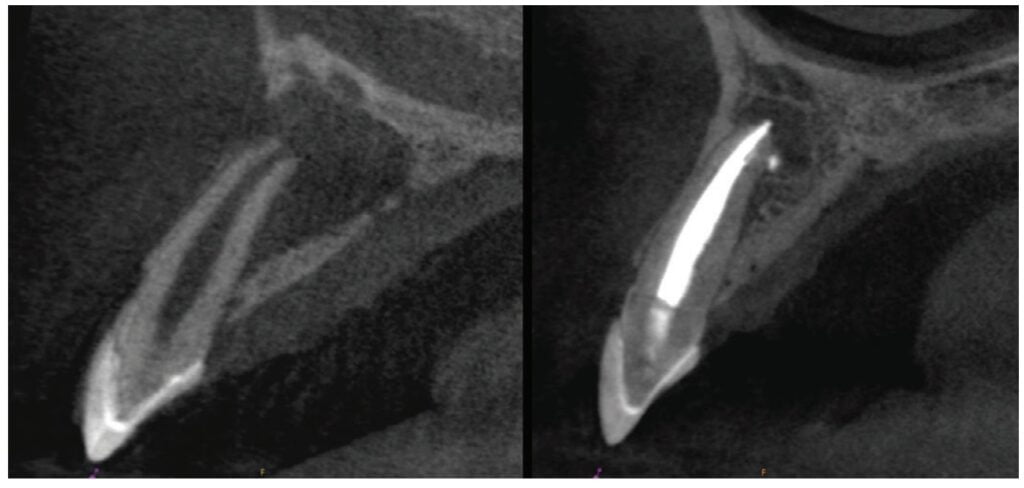
Case 2: Endo-perio: Single-appointment resolution with longer-term results
In this case, the endo-perio lesion was the result of periodontal and pulpal disease occurring within the same dental element. Diagnosis, prognosis, and treatment planning were complicated by the inter-relationships and simultaneous existence of both processes. Many of us were trained to treat a case like this just one way — multiple visits. Only shape and clean initially, and we should definitely be medicating.
Legacy workflow involved bringing the patient back to assess the periodontal status, followed by another treatment session with more anesthesia and a rubber dam.
An additional level of difficulty to consider was the “C-shaped” root form. It must be explained that the prognosis remains questionable, and only the desired periodontal healing can confirm a diagnosis of primary endo etiology. So successful resolution of periodontal symptoms after endodontic therapy is diagnostic in itself. Now we can offer same-day, unscheduled, single-appointment, and predictable endodontics for this patient using the GentleWave Procedure.

images. 6B. 3.5-year recall post-GentleWave® Procedure
A differential diagnosis to include root fracture and treatment options was discussed, and this patient consented to my primary recommendation for nonsurgical RCT.
Resolution of the current symptoms was certainly important, but confirming longer-range healing and tooth retention carried equal value. The probing depths and sinus tract resolved in 1 month, providing an immediate upgrade to the periodontal prognosis. The 3.5-year recall demonstrated continued and lasting healing of the endodontic component. This patient had completely regenerated hard tissues.

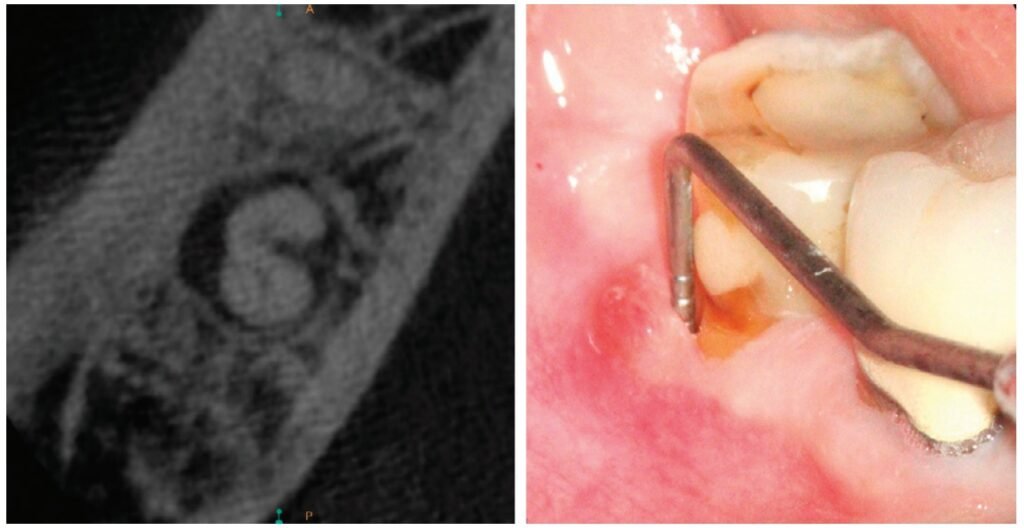
Case 3: A minimalistic approach with small shapes
With the GentleWave System, the emphasis on the decades-old endodontic triad of shape, clean, and obturate has shifted to cleaning, with shaping taking on a much lesser role. In my practice, a 6% taper now only has historical value. I no longer use files to shape in the traditional sense, but instead to provide a fluid pathway to dissolve vital pulp tissues, necrotic remnants, and remove biofilm from intricate canal anatomies previously inaccessible by traditional means of irrigation.

This case highlights a minimalistic approach with no shape exceeding .17 tip size or .04 taper. The DB and MB2 remained at .16 tip size with a .02 taper! The obturation optics would not have projected “a sense of clean” in years past, but now the GentleWave Procedure’s mechanism of action leaves areas of confluent isthmus and lateral canals free of debris. This style of endodontics is now possible due to the perfect storm of conservative shapes, bioceramic sealer, and an enhanced irrigation delivery system.
Evidence of accelerated healing was observed at the 3-month recall, and complete healing was verified at the 16-month recall.
Now we can offer same-day, unscheduled, single-appointment, and predictable endodontics for this patient using the GentleWave® Procedure.”
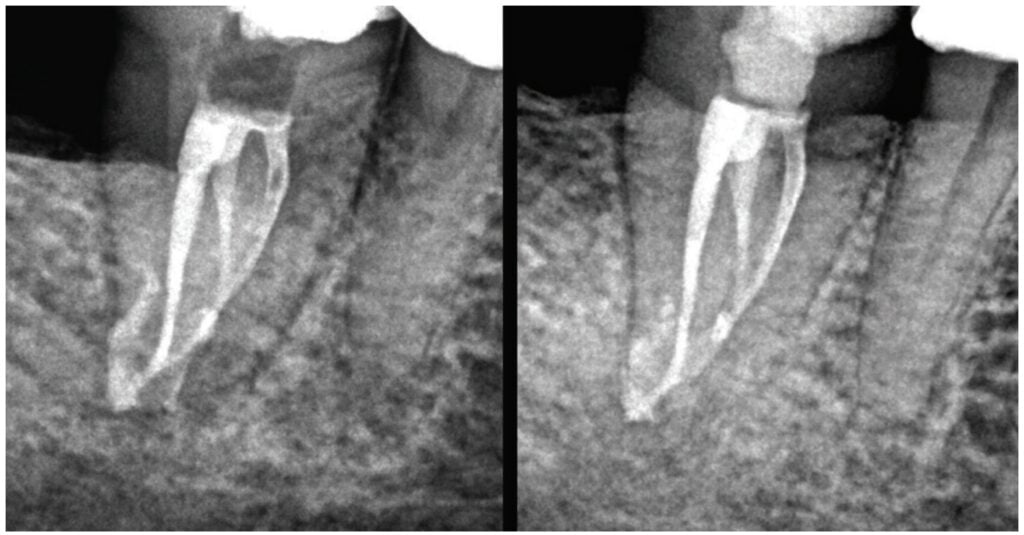
Case 4: Non-instrumentation endodontics
This next case represents a huge paradigm shift in how I treatment-plan emergency endodontic care and is a great opportunity to share how we can let go of deep-rooted protocols and embrace new technologies.

This young adult presented with buccal edema and significant pain. Upon access, purulent drainage was allowed to passively flow, but not for long. After a few brief moments to build a custom platform, the 9-minute GentleWave Procedure applied negative pressure to this closed-loop system, which enhanced the evacuation of drainage. It simultaneously provided a clean canal space, free of debris, and ready for same-day obturation with a combination of bioceramic putty/bioceramic sealer to address the open apex.
The canal walls of this 28 mm lateral incisor remained untouched. No files were used, not one! A fluid pathway to the portal of exit allowed for continuous exchange of irrigation fluids throughout the procedure. Once the procedure was completed, my patient reported, “Hey, Doc, the swelling in my face is nearly gone!” Continued follow-up care demonstrated complete regeneration of the buccal cortical plate.
post-GentleWave® Procedure
Implementing the GentleWave® System
My goal always is to make the canal anatomy as clean as possible, and GentleWave more than satisfies this criterion in a single-appointment model. Often, I am asked about the level of difficulty to expect while implementing the GentleWave System. It is not difficult, but it does require a commitment from the whole office. There is a lot of preparation to get your staff and practice ready, but once you integrate the system, you will discover it is worth it.
For more information on how the GentleWave system works, read “GentleWave: Root canals cleaned at the speed of sound” at https://endopracticeus.com/gentlewave-root-canals-cleaned-at-the-speed-of-sound/
- Paul Krasner, Rankow HJ, Abrams ES. Access Opening and Canal Location. ENDONDONTICS: Colleagues for Excellence newsletter. Spring 2010:2. https://www.aae.org/specialty/newsletter/access-opening-canal-location/. Accessed November 10, 2022.
Stay Relevant With Endodontic Practice US
Join our email list for CE courses and webinars, articles and more..

 Scott K. Hetz, DMD, is a Board-certified specialist in Endodontics. He is a 1997 graduate of the University of Pittsburgh School of Dental Medicine. Dr. Hetz served in the United States Air Force for 9 years, including an Advanced Education in General Dentistry program. Also, while on active duty, he received his specialty certificate in Endodontics from the University of Southern California in 2004.
Scott K. Hetz, DMD, is a Board-certified specialist in Endodontics. He is a 1997 graduate of the University of Pittsburgh School of Dental Medicine. Dr. Hetz served in the United States Air Force for 9 years, including an Advanced Education in General Dentistry program. Also, while on active duty, he received his specialty certificate in Endodontics from the University of Southern California in 2004.
