Dr. Gregori Kurtzman considers the details needed to decide between endodontics or implants in treatment planning.
Dr. Gregori M. Kurtzman discusses treatment planning for long-term success
Endodontic therapy provides preservation of the natural dentition, which is a primary goal of dentistry. Yet endodontic success is closely linked to the restorability of the coronal aspect of the tooth. Being able to identify, instrument, and obturate the canals is important, but if the tooth cannot be predictably restored, then treatment will not provide clinical success. A lack of sufficient coronal structure to retain a restoration returning the tooth to natural anatomy often leads to dislodgement of the restoration during function, failure of the coronal seal of the canal system, and subsequent failure of the endodontic obturation.
When a patient presents with significant coronal breakdown of a tooth, this presents clinical challenges with regard to treatment planning decisions. If the practitioner performs endodontic treatment in their practice, do they treat the tooth and augment that treatment with crown lengthening to permit sufficient ferrule (a band of natural tooth that is circumferentially grasped by the crown that prevents lateral displacement of the crown from the tooth) of the remaining root structure to allow restoration, or is it more prudent to extract the tooth and place an implant? If the practitioner is an endodontist, and the patient was referred for treatment, has the referring general dentist determined that sufficient tooth structure is present to restore the tooth predictably following endodontic treatment? We have to understand that endodontics is a restorative treatment with an endodontic component, and evaluation in that regard needs to be accomplished prior to initiating any endodontic treatment.
Treatment planning decisions need to focus on the restorability of the tooth when deciding what treatment will provide reasonable longterm success.
With regard to indirect restorations such as full coverage crowns and onlays, the literature has suggested that a 1.5-mm to 2-mm ferrule is minimally necessary to prevent fracture of the endodontically treated tooth and provide resistance to displacement of the fixed restoration.1-5 Today with improvements in adhesive dentistry, the emphasis has drifted away from the principle of restorative ferrule. Practitioners may be relying too heavily on adhesive bond strength to retain fixed prosthetic restoration margins sealed. Thus, thought should be given to how much coronal structure remains when deciding if a tooth should be treated endodontically or replaced with an implant. Those restorative decisions need to be made prior to the initiation of endodontic treatment. The practitioner must determine which additional procedures will be necessary to achieve the required restorative goals and how those procedures will affect the tooth being treated and adjacent teeth.
Raise the bridge or lower the water?
When a patient presents with a broken-down tooth that has pulpal issues or would require intentional endodontics to allow restoration, the restorability of that affected tooth needs to be the first consideration in deciding how and what treatment is required for long-term predictability. When analyzing how that tooth may be restored following endodontic treatment, one has to determine if sufficient root length remains to allow stability of the tooth once it is restored. Is adequate supracrestal tooth structure present to provide a restorative ferrule? What ancillary procedures may help increase supracrestal tooth structure to ferrule?
Osseous crown lengthening to improve restorative ferrule
Traditionally, when insufficient tooth structure presents supracrestally, osseous crown-lengthening procedures have been employed to increase the available coronal tooth structure to achieve a restorative ferrule.6,7 This presents challenges in treatment with regard to adjacent teeth. Osseous crown lengthening will require the removal of crestal bone on the adjacent teeth to create osseous slopes that will allow soft tissue maintenance. One cannot just remove bone around an individual tooth which leads to isolated pocketing and abrupt slopes in the bone. This then leads to adjacent bone loss as the body attempts to create gentle crestal osseous slopes that it can maintain over time. So, to create adequate coronal tooth structure for restorative purposes the periodontal structures adjacent to that tooth may have to be compromised.
The removal of crestal bone additionally may expose furcations on posterior teeth that can complicate home care — exposing areas that may be difficult to maintain over the long-term by the patient. This may also be a factor in the maxillary first premolars, which typically have a mesial root concavity that can create restorative challenges. When the tooth being treated has a short cervical trunk, or the furcation is already at or just coronal to the crestal margin, removal of additional bone may be contraindicated, and extraction of the tooth and subsequent replacement with an implant may be a more prudent treatment option. Some studies have reported lower long-term survival in those endodontically treated teeth that underwent osseous crown lengthening, and this should be a consideration in decisions that may incorporate that into the treatment plan.8-10
Forced orthodontic eruption
An alternative to osseous crown lengthening when additional tooth structure is needed restoratively is the use of forced orthodontic eruption.11,12 Following completion of endodontic treatment, orthodontic forces are used to erupt the tooth coronally, exposing more root structure upon which a ferrule may be placed.13-15 When this option is considered, one needs to assess how much root length will remain within the osseous housing following forced orthodontic eruption and whether this allows an adequate crown-to-root ratio to maintain tooth stability over time. This approach is more ideally suited for single rooted teeth than multi-rooted teeth.16,17 As with crown lengthening, forced eruption of multi-rooted teeth may create furcation issues and may be a contraindication to this treatment modality.
Orthodontic extrusion involves slow forces of low intensity that are exerted on the tooth and as the tooth extrudes, the crestal bone and gingival apparatus move together coronally. When heavier traction forces are exerted, as seen in rapid extrusion, coronal migration of the tissues supporting the tooth is less pronounced. As rapid movement exceeds the capacity for physiologic adaptation, the tooth erupts coronally beyond the crestal bone.18,19 Following rapid extrusion, an extended period of retention is needed to allow remodeling and adaptation of the periodontium to the new tooth position.20,21

Clinical decisions for single-rooted teeth
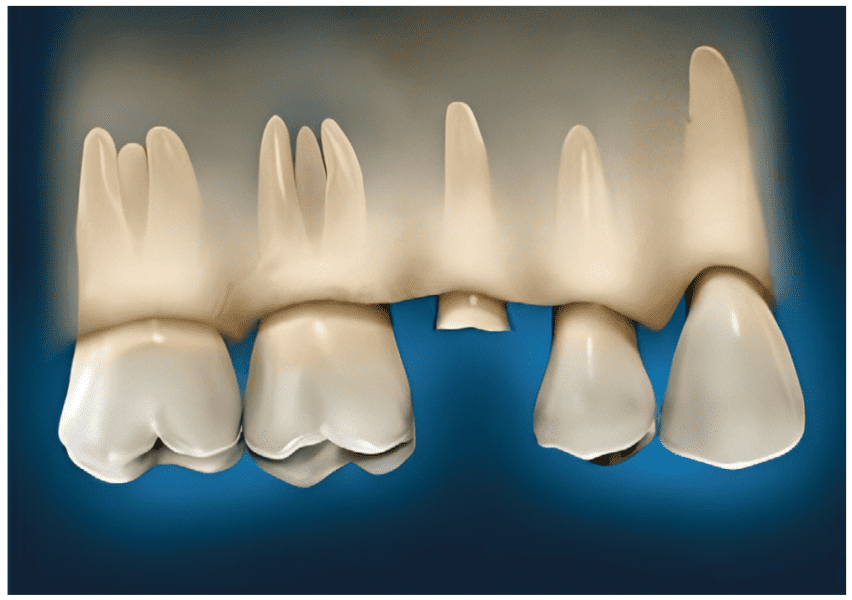
If a patient presents with coronal breakdown of a single-rooted tooth that is at or close to the crestal bone margin (Figure 1), the length of the root subcrestally must be determined. Is there sufficient root length so that movement of the crestal margin in relation to the coronal of the remaining tooth structure will not compromise the crown-to-root ratio of the restored tooth? If the answer is “yes,” then two options should be considered: clinical crown lengthening (Figure 2) or orthodontic extrusion (Figure 3). Should the answer be “no,” then extraction and replacement with an implant is the treatment that is indicated.

Clinical decisions for multi-rooted teeth
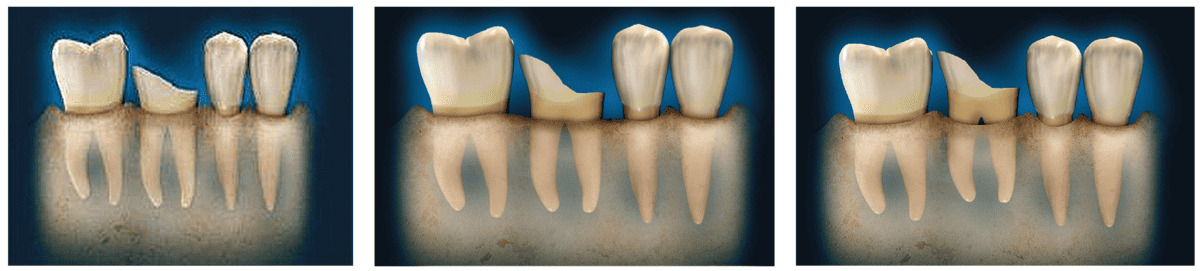
A common clinical occurrence involves the presentation of a molar with significant coronal breakdown either because of fracture or decay (Figure 4). The presence of a furcation presents unique variables compared to single-rooted teeth. When analyzing the restorability of a molar, practitioners need to consider: repositioning the crestal bone margin either through osseous crown lengthening (Figure 5) or extrusion (Figure 6) to expose the furcation and complicate long-term patient home care and tooth maintenance. Teeth with short cervical areas (portion of the tooth superior to the start of the furcation) limit what treatments may be performed to provide restorative ferrules. Teeth with long cervical areas or fused roots may be better suited to those procedures, providing clinical outcomes that can be maintained over the long-term by the patient. When these objectives cannot be met, extraction and implant placement offer a better prognosis.
Conclusion
Dentistry is restoratively-driven, supplemented by endodontic and surgical components. When a tooth cannot be restored, then it does not matter whether endodontic treatment can be or is rendered — long-term survival of that tooth cannot be predictably achieved. Treatment planning decisions need to focus on the restorability of the tooth when deciding what treatment will provide reasonable long-term success. The patient’s age plays a factor in those treatment-planning decisions. A patient in their 80s with the same lack of restorative ferrule presents less long-term considerations than a similar tooth on a patient who is 70 years old or younger in better health. If the tooth can be restored, then pursuing endodontic treatment is the best treatment decision. But when this cannot be accomplished or the restorative prognosis cannot provide reasonable long-term success, then extraction and implant placement is the more prudent treatment option.
Dr. Kurtzman enjoys many aspects of dentistry, whether endodontics or implants, or other innovative treatments. Read more about his practice here: https://endopracticeus.com/gregori-kurtzman-dds-magd-fpfa-facd-fadi-dicoi-dadia/
- Libman WJ, Nicholls JI. Load fatigue of teeth restored with cast posts and cores and complete crowns. Int J Prosthodont. 1995 Mar-Apr;8(2):155-161.
- Tan PL, Aquilino SA, Gratton DG, Stanford CM, Tan SC, Johnson WT, Dawson D. In vitro fracture resistance of endodontically treated central incisors with varying ferrule heights and configurations. J Prosthet Dent. 2005 Apr;93(4):331-336.
- Ichim I, Kuzmanovic DV, Love RM. A finite element analysis of ferrule design on restoration resistance and distribution of stress within a root. Int Endod J. 2006 Jun;39(6):443-452.
- Juloski J, Radovic I, Goracci C, Vulicevic ZR, Ferrari M. Ferrule effect: a literature review. J Endod. 2012 Jan;38(1):11-19.
- Meng Q, Chen Y, Ni K, Li Y, Li X, Meng J, Chen L, Mei ML. The effect of different ferrule heights and crown-to-root ratios on fracture resistance of endodontically-treated mandibular premolars restored with fiber post or cast metal post system: an in vitro study. BMC Oral Health. 2023 Jun 3;23(1):360.
- Planciunas L, Puriene A, Mackeviciene G. Surgical lengthening of the clinical tooth crown. 2006;8(3):88-95.
- Marzadori M, Stefanini M, Sangiorgi M, Mounssif I, Monaco C, Zucchelli G. Crown lengthening and restorative procedures in the esthetic zone. Periodontol 2000. 2018 Jun;77(1):84-92.
- Camargo PM, Melnick PR, Camargo LM. Clinical crown lengthening in the esthetic zone. J Calif Dent Assoc. 2007 Jul;35(7):487-498.
- Patil K, Khalighinejad N, El-Refai N, Williams K, Mickel A. The Effect of Crown Lengthening on the Outcome of Endodontically Treated Posterior Teeth: 10-year Survival Analysis. J Endod. 2019 Jun;45(6):696-700.
- Brignardello-Petersen R. There is probably a higher risk of undergoing tooth extraction in teeth that received crown-lengthening procedures. J Am Dent Assoc. 2019 Oct;150(10):e163.
- Huang G, Yang M, Qali M, Wang TJ, Li C, Chang YC. Clinical Considerations in Orthodontically Forced Eruption for Restorative Purposes. J Clin Med. 2021 Dec 18; 10(24):5950.
- Bruhnke M, Krastl G, Neumeyer S, Beuer F, Herklotz I, Naumann M. Forced Orthodontic Extrusion to Restore the Unrestorable: A Proof of Concept. Int J Periodontics Restorative Dent. 2023 Sep-Oct;43(5):560-569.
- Bajaj P, Chordiya R, Rudagi K, Patil N. Multidisciplinary approach to the management of complicated crown-root fracture: a case report. J Int Oral Health. 2015 Apr;7(4): 88-91.
- Cordaro M, Staderini E, Torsello F, Grande NM, Turchi M, Cordaro M. Orthodontic Extrusion vs. Surgical Extrusion to Rehabilitate Severely Damaged Teeth: A Literature Review. Int J Environ Res Public Health. 2021 Sep 10;18(18):9530.
- Kocadereli I, Taşman F, Güner SB. Combined endodontic-orthodontic and prosthodontic treatment of fractured teeth. Case report. Aust Dent J. 1998 Feb;43(1):28-31.
- Pedullà E, Valentino J, Rapisarda S. Endodontic Surgery of a Deviated Premolar Root in the Surgical Orthodontic Management of an Impacted Maxillary Canine. J Endod. 2015 Oct;41(10):1730-1734.
- Delivanis P, Delivanis H, Kuftinec MM. Endodontic-orthodontic management of fractured anterior teeth. J Am Dent Assoc. 1978 Sep;97(3):483-485.
- Bach N, Baylard JF, Voyer R. Orthodontic extrusion: periodontal considerations and applications. J Can Dent Assoc. 2004 Dec;70(11):775-780.
- Faria LP, Almeida MM, Amaral MF, Pellizzer EP, Okamoto R, Mendonça MR. Orthodontic Extrusion as Treatment Option for Crown-Root Fracture: Literature Review with Systematic Criteria. J Contemp Dent Pract. 2015 Sep 1;16(9):758-762.
- Antrim DD. Vertical extrusion of endodontically treated teeth. US Navy Med. 1981; 72:23-28.
- González-Martín O, Solano-Hernandez B, González-Martín A, Avila-Ortiz G. Orthodontic Extrusion: Guidelines for Contemporary Clinical Practice. Int J Periodontics Restorative Dent. 2020 Sep/Oct;40(5):667-676.
Stay Relevant With Endodontic Practice US
Join our email list for CE courses and webinars, articles and more..

 Gregori M. Kurtzman, DDS, MAGD, FPFA, FACD, FIADFE, DICOI, DADIA, DIDIA, in private general dental practice in Silver Spring, Maryland, was a former Assistant Clinical Professor at University of Maryland in the department of Restorative Dentistry and Endodontics, and a former AAID Implant Maxi-Course assistant program director at Howard University College of Dentistry. He has lectured internationally on the topics of restorative dentistry, endodontics and implant surgery, removable and fixed prosthetics, and periodontics and has over 850 published articles globally, several ebooks, and textbook chapters. He has earned Fellowship in the AGD, American College of Dentists (ACD), International Congress of Oral Implantology (ICOI), Pierre Fauchard, ADI, International Academy for Dental Facial Esthetics (IADFE), Mastership in the AGD and ICOI, and Diplomat status in the ICOI, American Dental Implant Association (ADIA), and International Dental Implant Association (IDIA).
Gregori M. Kurtzman, DDS, MAGD, FPFA, FACD, FIADFE, DICOI, DADIA, DIDIA, in private general dental practice in Silver Spring, Maryland, was a former Assistant Clinical Professor at University of Maryland in the department of Restorative Dentistry and Endodontics, and a former AAID Implant Maxi-Course assistant program director at Howard University College of Dentistry. He has lectured internationally on the topics of restorative dentistry, endodontics and implant surgery, removable and fixed prosthetics, and periodontics and has over 850 published articles globally, several ebooks, and textbook chapters. He has earned Fellowship in the AGD, American College of Dentists (ACD), International Congress of Oral Implantology (ICOI), Pierre Fauchard, ADI, International Academy for Dental Facial Esthetics (IADFE), Mastership in the AGD and ICOI, and Diplomat status in the ICOI, American Dental Implant Association (ADIA), and International Dental Implant Association (IDIA).
