Editor’s intro: Using CBCT for diagnosis and surgical planning can help with removal of gutta percha in the maxillary sinus. This article discusses the benefits of seeing the dental anatomy in 3D.
Drs. Clovis Monteiro Bramante, Jussaro Alves Duque, Murilo Priori Alcalde, Victor de Moraes Cruz, Alexandre Silva Bramante, Talita Tartari, Braulio Pasternak Jr, Cesar Augusto Pereira Oliveira, and Marco Antonio Hungaro Duarte discuss helpful tools to aid in the planning of endodontic surgeries
Abstract
One type of accident that can occur during endodontic treatments is the overextension of gutta percha to periapical tissues, which could necessitate surgical intervention. The purpose of this article is to describe endodontic surgery in the apical region of the maxillary premolar. Radiography showed extrusion of the gutta-percha cone from the apex of the palatal root. A cone beam computed tomography (CBCT) scan confirmed that the extruded material was inside the maxillary sinus. The CBCT scan also was used to assist in surgical planning. During the surgical management of the patient, an osteotomy was performed employing an ultrasonic insert to provide access to the maxillary sinus, and gutta percha was removed. At the 12-month follow-up, both clinical and radiographic exams showed adequate healing. The CBCT proved to be an excellent tool to aid in planning endodontic surgeries. Use of an ultrasonic insert in the osteotomy demonstrated to be a safer alternative.
Introduction

The extrusion of filling material is a type of accident that can occur during endodontic treatments1,2 due to factors such as apical root resorption, overinstrumentation, destruction of the apical constriction, inadequate preparation of the apical stop, or the use of undersized the gutta-percha master cone.2-4 When gutta percha goes beyond the foramen, the prognosis is unfavorable once it can act as a foreign body and contribute to the formation or maintenance of an apical lesion and can lead to postoperative complications such as chronic inflammation.5,6 Thus, it is necessary to remove the extravasated material, which is a challenge since it is performed through the canal, and in many situations, a fragment may remain in the periapical tissues.7
Surgical intervention is a solution to this problem. However, there are several factors to take into consideration during the surgery, such as the relationship between the tooth and anatomical structures such as the maxillary sinus. In these cases, cone beam computed tomography (CBCT) is an excellent tool for diagnosis, including localization of extruded materials into the adjacent anatomic structures,8,9 and surgical planning.9 The CBCT scan will show if there is involvement of the maxillary sinus, provide the relation of the root apices with the neighboring structures, and help to establish the site where the osteotomy should be done to perform a minimally invasive surgery.10,11

A conventional technique to access the area of interest during surgery is the use of manual and rotary instruments. However, this technique can cause thermal injury to the bone and other adjacent structures.12 An alternative to traditional techniques is the use of ultrasound for osteotomies. The advantages of this method include the selective cut of mineralized tissue without damaging the adjacent soft tissue and without generating heat, better visualization of the surgical field, and less vibration and noise.10,13
This case report describes an endodontic surgery to remove an overextended gutta-percha master cone from the maxillary sinus using CBCT to aid in diagnosis and surgical planning and the ultrasound to perform the osteotomy.
Case report
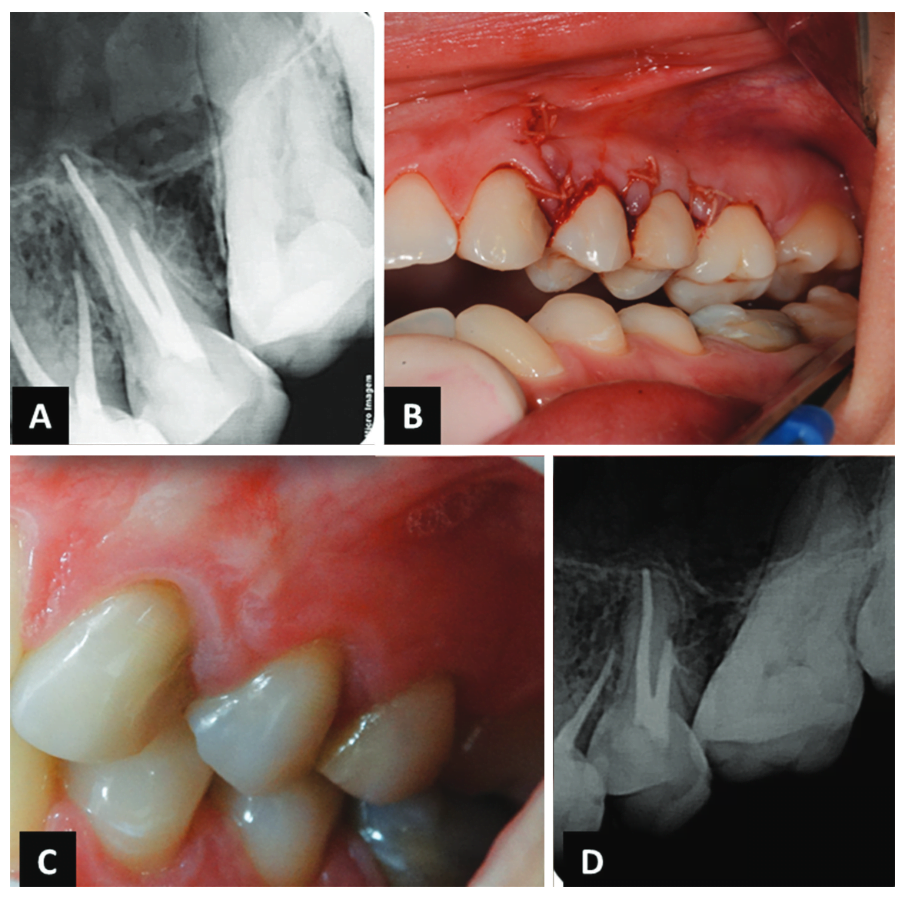
A 27-year-old woman sought dental care due to sensitivity in the apical region of the maxillary left second premolar (tooth No. 25), but without visually noticeable clinical changes. The periapical radiographic showed severe overextension of a gutta-percha cone through the foramen of the palatal of tooth No. 25. A CBCT confirmed the position of the palatal root and the extruded material within the maxillary sinus (Figure 1), which led to the decision to conduct an endodontic surgery to remove the overextended material.
Local anesthesia was performed by alveolar superior posterior terminal infiltration and using the infraorbital nerve block technique with 4% articaine. A horizontal intrasulcular incision that extended from the distal surface of the maxillary left first molar (tooth No. 26) to the mesial region of maxillary left first premolar (tooth No. 24), and a vertical incision, made on the mesial surface of tooth No. 24, were performed in the buccal vestibule to facilitate the elevation of the full-thickness flap.
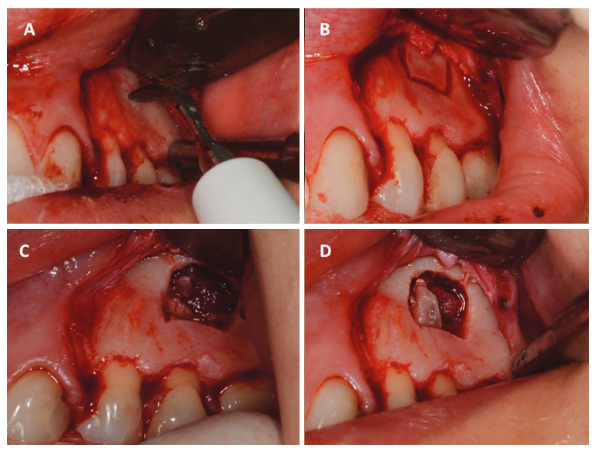
After mucoperiosteal divulsion, no evidence of vestibular cortical bone fenestration was perceived. Once the position of the root apex was established with the aid of CBCT, a quadrangular-shaped sinus window was accomplished to give access to the maxillary sinus. The osteotomy was performed by means of the ultrasonic insert Osteo 19 (Helse Dental Technology, Santa Rosa de Viterbo, SP, Brazil) (Figure 2) attached to the ultrasonic device Jet Sonic (Gnatus, Ribeirão Preto, Brazil) used in endo function with the power level set at 10 and under saline coolant spray. The gutta-percha master cone was easily visualized within the sinus, and then the surgeon proceeded to remove it with the aid of curettes (Figure 3). To prevent the overflow of gutta percha into the maxillary sinus, the palatal side of the root was protected with gauze. In the transoperative radiography, complete elimination of gutta-percha was observed, and then the apical plasty was performed with an apical file.
The bony lid was folded back, covered with the mucoperiosteal flap, and then the horizontal incision was sutured with overlapping points, simple transpapillary, and vertical stiches.
The patient was discharged with instructions regarding necessary postoperative care, and a prescription of an anti-inflammatory medication for 5 days. At a 1-week postoperative appointment, the sutures were removed, and the area presented uneventful healing with no evidence of infection and oroantral communication. At the 12-month follow-up, both clinical and radiographic exams showed an absence of symptoms and an adequate healing (Figure 4).
Discussion
Anatomically, the premolars and molars come into a close relationship with the maxillary sinus, and their roots may project into it.14,15 When there is a need for surgical intervention in any of these teeth, CBCT can be a resource used to obtain a three-dimensional view and the actual relationship of the tooth/lesion with the maxillary sinus.11,16 In this case, CBCT clearly showed that the gutta-percha cone had overpassed the apex of the palatal root and established the distance that it had penetrated the wall of the maxillary sinus.
The roots of the upper posterior teeth are in direct contact with the maxillary sinus, and the extrusion of endodontic sealers or gutta percha into it can trigger an inflammatory process that persists until the material is removed.17 The presence of a foreign substance within the maxillary antrum may lead to the onset of sinusitis,2 pain on mastication, and tenderness palpation.17 Symptoms like sinus tenderness and nasal stuffiness were experienced by a patient because the gutta percha that extruded into the maxillary sinus had migrated to the ethmoid sinus. Furthermore, as most root canal filling materials are zinc oxide-based (including gutta-percha), they can favor the growth of Aspergillus fumigatus, leading to the development of Aspergillosis infection19-21 and a fungus ball formation.22
The attempt to remove extruded gutta percha via the root canal is not always successful, and it is often necessary to perform surgery.2,10 In cases where endodontic surgery is required, the conventional technique, which uses manual and rotary instruments, is the most used in osteotomy and apicectomy. However, the use of ultrasound in oral surgeries in general has gained prominence and has shown some advantages over conventional surgery.10,13 In endodontic surgery, ultrasound has been used for osteotomy procedures, root-end resection, preparation of the apical cavity for retrofilling, and enucleation of radicular cysts, in addition to other types of procedures.10 Ultrasound has been shown to be efficient, more comfortable for both the patient and professional, and has decreased the risk of accidents and contamination. Also, ultrasound produces a more visible surgical field due to less bleeding and allows for greater safety, especially when surgery is close to important areas such as nerves, blood vessels, and the maxillary sinus.10,13,23 In this case report, the osteotomy was performed with conventional nonsurgical ultrasound and a new insert developed by the company Helse Dental Technology, which proved to be very effective in the procedure. This technique allowed a safer osteotomy without risk of sinus membrane perforation, as can happen with the use of chisels and drills, better access to the area, and a more conservative removal of bone. Through the surgical window, it was possible to access the root and remove the extravasated material with a good safety margin and reduced bone loss.
The communication between the surgical cavity and the maxillary sinus is another critical factor to be taken into consideration because contamination can lead to failure of surgery. At the end of the procedure, the juxtaposition of the suture was obtained with simple transpapillary stitches. Perfect re-adaptation of the flap was achieved, thereby avoiding any accidental breakpoints and exposure of the surgical field. The post-operative period was quite comfortable for the patient, confirming previous findings.23,24 Thus, it can be concluded that the osteotomy performed with ultrasound is an alternative technique that provides the patient with a safer and comfortable surgery.
Conclusions
It was concluded that the use of CBCT was important in the diagnosis and surgical planning of this case and that the use of the ultrasound for the osteotomy proved to be a simpler and safer alternative to avoid injuries to vital structures.
For more information on the benefits and limitation of CBCT for diagnosis and surgical planning, check out Dr. Alix Davies’ CE — subscribers can receive 2 credits after passing the quiz!
- Da Silva D, Endal U, Reynaud A, et al. A comparative study of lateral condensation, heat-softened gutta-percha, and a modified master cone heat-softened backfilling technique. Int Endod J. 2002;35(12):1005-1011.
- Oguz Y, Soydan SS. Maxillary sinusitis as a complication of an extruded gutta-percha: a case report. Cumhuriyet Dent J. 2014;17(suppl 1) :36-39.
- Kaplowitz GJ. Penetration of the maxillary sinus by overextended gutta percha cones. Report of two cases. Clin Prev Dent. 1985;7(2):28-30.
- Ritchie GM, Anderson DM, Sakumura JS. Apical extrusion of thermoplasticized gutta-percha used as a root canal filling. J Endod. 1988;14(3):128-132.
- Scarparo RK, Grecca FS, Fachin EV. Analysis of tissue reactions to methacrylate resin-based, epoxy resin-based, and zinc oxide-eugenol endodontic sealers. J Endod. 2009;35(2):229-232.
- Ribeiro DA. Do endodontic compounds induce genetic damage? A comprehensive review. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 2008;105(2):251-256.
- Costa F, Robiony M, Toro C, Sembronio S, Politi M. Endoscopically assisted procedure for removal of a foreign body from the maxillary sinus and contemporary endodontic surgical treatment of the tooth. Head Face Med. 2006;2:37.
- Pasqualini D, Scotti N, Ambrogio P, Alovisi M, Berutti E. Atypical facial pain related to apical fenestration and overfilling. Int Endod J. 2012;45(7):670-677.
- Cotton TP, Geisler TM, Holden DT, Schwartz SA, Schindler WG. Endodontic applications of cone-beam volumetric tomography. J Endod. 2007;33(9):1121-1132.
- Abella F, de Ribot J, Doria G, Duran-Sindreu F, Roig M. Applications of piezoelectric surgery in endodontic surgery: a literature review. J Endod. 2014;40(3):325-332.
- Low KM, Dula K, Burgin W, von Arx T. Comparison of periapical radiography and limited cone-beam tomography in posterior maxillary teeth referred for apical surgery. J Endod. 2008;34(5):557-562.
- Rashad A, Kaiser A, Prochnow N, et al. Heat production during different ultrasonic and conventional osteotomy preparations for dental implants. Clin Oral Implants Res. 2011;22(120:1361-1365.
- Pavlíková G, Foltán R, Horká M, et al. Piezosurgery in oral and maxillofacial surgery. Int J Oral Maxillofac Surg. 2011;40(5):451-457.
- Hauman CH, Chandler NP, Tong DC. Endodontic implications of the maxillary sinus: a review. Int Endod J. 2002;35(2):127-141.
- von Arx T, Fodich I, Bornstein MM. Proximity of premolar roots to maxillary sinus: a radiographic survey using cone-beam computed tomography. J Endod. 2014;40(10):1541-1548.
- Lavasani SA, Tyler C, Roach SH, et al. Cone-beam computed tomography: anatomic analysis of maxillary posterior teeth-impact on endodontic microsurgery. J Endod. 2016;42(6):890-895.
- Brooks JK, Kleinman JW. Retrieval of extensive gutta-percha extruded into the maxillary sinus: use of 3-dimensional cone-beam computed tomography. J Endod. 2013;39(9):1189-1193.
- Ishikawa M, Mizuno T, Yamazaki Y, et al. Migration of gutta-percha point from a root canal into the ethmoid sinus. Br J Oral Maxillofac Surg. 2004;42(1):58-60.
- Khongkhunthian P, Reichart PA. Aspergillosis of the maxillary sinus as a complication of overfilling root canal material into the sinus: report of two cases. J Endod. 2001;27(7):476-478.
- Giardino L, Pontieri F, Savoldi E, Tallarigo F. Aspergillus mycetoma of the maxillary sinus secondary to overfilling of a root canal. J Endod. 2006;32(7):692-694.
- Yamaguchi K, Matsunaga T, Hayashi Y. Gross extrusion of endodontic obturation materials into the maxillary sinus: a case report. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 2007;104(1):131-134.
- Mensi M, Piccioni M, Marsili F, et al. Risk of maxillary fungus ball in patients with endodontic treatment on maxillary teeth: a case-control study. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 2007;103(3):433-436.
- García B, Peñarrocha M, Peñarrocha MA, von Arx T. Apical surgery of a maxillary molar creating a maxillary sinus window using ultrasonics: a clinical case. Int Endod J. 2010;43(11):1054-1061.
- Troedhan A, Kurrek A, Wainwright M. Ultrasonic piezotome surgery: is it a benefit for our patients and does it extend surgery time? A retrospective comparative study on the removal of 100 impacted mandibular 3rd molars. Open J Stomatol. 2011;1(4):179-184.
Stay Relevant With Endodontic Practice US
Join our email list for CE courses and webinars, articles and more..


