Editor’s intro: Vital pulp cryotherapy has been shown to reduce postoperative pain, and Dr. James Bahcall discusses clinical case selection and treatment technique for this new procedure.
Drs. James Bahcall, Bradford Johnson, Qian Xie, Mark Baker, and Steve Weeks explore a new application for pulpal tissue
Introduction
The term cryotherapy is derived from the Greek word cryos, meaning “cold.”1 The goal of cryotherapy is to remove the heat by lowering the temperature of the tissue.2 Through the application of cold to human tissue, it has been shown to decrease nerve conduction velocity, reduce hemorrhage and edema, along with inflammation.3 Cryotherapy has also been shown to reduce the number of leukocytes adhering to the endothelial wall of capillaries, thus having fewer of these types of cells migrating to the affected tissue, reducing endothelial dysfunction and providing a further reduction in inflammation.4
The use of cryotherapy has been common practice in medicine and other fields of dentistry.5 In medicine, cryotherapy, sometimes referred to as cryosurgery, is a procedure used to destroy tissue of both benign and malignant lesions by the freezing and re-thawing process. Examples of the uses of cryotherapy in medicine are the treatment (removal) of various types of skin lesions, the treatment of dysplastic (pre-cancerous) tissue of the uterine cervix, and the treatment of some prostate cancers. Cryotherapy can also refer to the use of ice or cold packs applied to a part of the body after an injury to reduce inflammation.6
Within the field of endodontics, although there are no previous vital pulp cryotherapy cases reported in the endodontic literature, there has been recent reports of the success in using cold saline (2°C) irrigation in a root canal prior to canal obturation in order to reduce postoperative pain.7,8
The application of cryotherapy on pulpal tissue that has been exposed or indirectly exposed due to carious lesion excavation in conjunction with ethylenediaminetetraacetic acid (EDTA) irrigation, bioceramics, and a permanent restorative material (composite or amalgam) has shown to reduce post-operative pain after vital pulp cryotherapy. This article will discuss clinical case selection and treatment technique when performing this new vital pulp cryotherapy procedure.
Vital pulp cryotherapy technique
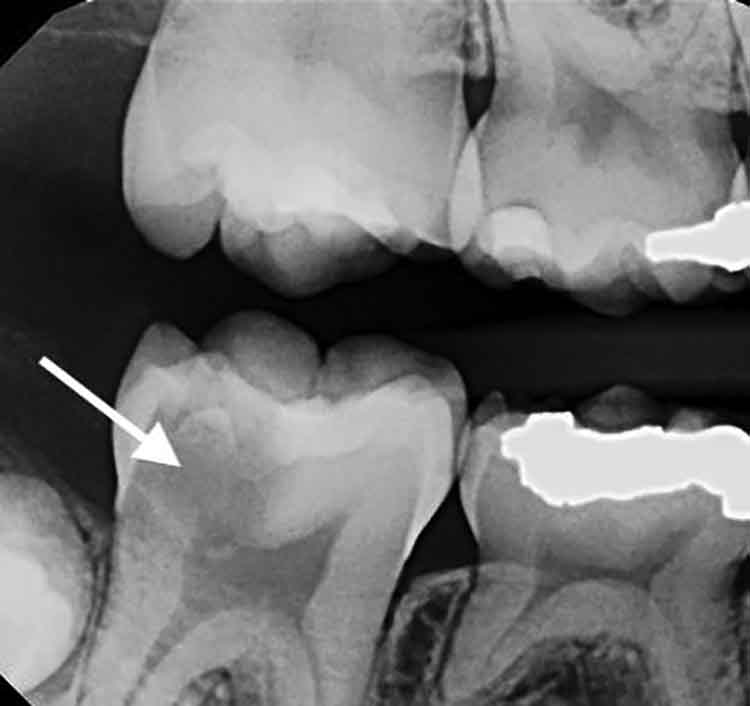
Prior to initiating vital pulp cryotherapy, a pretreatment pulpal and periradicular diagnosis needs to be obtained. The pretreatment pulpal and periradicular diagnosis of a tooth begins by first reviewing the patient’s medical and dental history. This also should include taking a patient’s blood pressure, pulse, and temperature (if indicated). Next, current preoperative radiographs: periapical, bitewing, and cone beam computed tomography (CBCT) (as indicated) should be taken (Figure 1).
After obtaining current radiographs, objective pulpal and periradicular clinical sensibility testing should be performed. Patients that present with a pretreatment pulpal diagnosis of a normal pulp, reversible pulpitis, or irreversible pulpitis, along with the possibility of a direct or indirect pulp exposure as a result from caries excavation, are good candidates for a pulp-capping or a partial pulpectomy procedure.9,10 Pulps that have a pretreatment diagnosis of necrosis or upon pulp chamber access are observed to have partial pulpal necrosis; vital pulp cryotherapy treatment is contraindicated.
In regard to the pretreatment periradicular diagnosis, normal or symptomatic apical periodontitis (percussion and/or palpation-sensitive without radiographic evidence from a periapical radiograph and/or a CBCT, of a periradicular radiolucency [lesion]) are not contraindicated for vital pulp cryotherapy treatment. Asymptomatic apical periodontitis or chronic/acute apical abscesses are contraindicated for vital pulp cryotherapy treatment because these are radiographic and clinical signs the pulpal tissue could be either necrotic or partially necrotic.
Lastly, prior to performing vital pulp cryotherapy, the treatment tooth must be deemed restorable with a permanent restoration of a composite or amalgam. Restoring the tooth posttreatment with a fabricated crown or a temporary filling and then placing a permanent filling at a subsequent appointment is contraindicated. The reason a permanent restoration is placed is twofold: First, it is important to maintain a proper seal in order to prevent penetration related to salivary (microbial) leakage from causing the reoccurrence of pulpal inflammation. Second, if the tooth remains asymptomatic posttreatment, you do not risk the chance of causing further inflammation of the pulpal and periradicular tissue by performing a crown preparation or replacing the temporary filling with a permanent filling at a subsequent appointment.11
In addition, there is always the chance of a patient developing or maintaining the pretreatment pulpal diagnosis of symptomatic irreversible pulpitis after the vital pulp cryotherapy procedure and hence requiring a full pulpectomy. If this does occur, having a permanent restoration (composite or amalgam) in place will allow for a better conventional endodontic treatment access seal as compared to a temporary filling.
After obtaining the proper pretreatment pulpal and periradicular diagnosis for vital pulp cryotherapy, along with the tooth’s restorability meeting the above criterion for a permanent restoration, the clinician can proceed with providing local anesthesia. After local anesthesia is given, and objective testing (no response to cold and/or electric pulp testing) is performed on the treatment tooth to confirm pulpal anesthesia,12 a rubber dam is placed, and the carious lesion is removed with a high-speed bur. If the pulp is exposed or indirectly exposed as a result of removing all the caries, vital pulp cryotherapy is indicated.
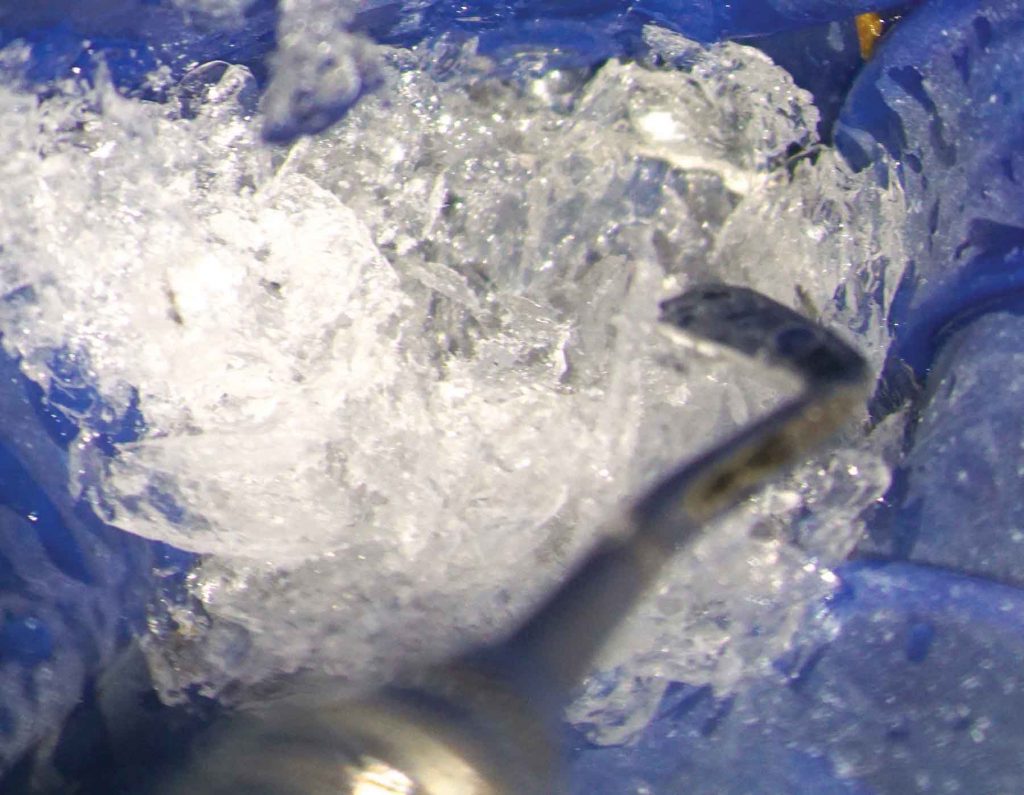
Shaved sterile water ice (0°C) is then placed over the direct or the indirect exposure of the pulpal tissue along with the entire tooth (Figure 2). The shaved sterile water ice is produced by the freezing of sterile water and then placing it in an ice shaving device. After approximately 1 minute, the ice melts and should be removed with a high-speed suction.
Following the removal of the melted sterile ice, the exposed or indirect exposed pulp should be irrigated with 17% EDTA solution for 1 minute.13,14 Although it has been stated in the literature to use sodium hypochlorite to control pulpal hemorrhage,15 it is important to note that sodium hypochlorite should not be applied to a direct or indirect pulp exposure when performing a vital pulp cryotherapy procedure. The reason for this is that sodium hypochlorite can kill the dental pulpal stem cells.14 EDTA solution should be used in place of sodium hypochlorite because it has been shown to release bioactive growth factors from the dentin, thus stimulating matrix secretion, odontoblast differentiation, and tertiary dentin formation. The conditioning of the dentin with EDTA will also promote the adhesion, migration, and differentiation of dental pulp stem cells.13,14,16 In a report by Finnegan, et al.,17 EDTA was shown to have antimicrobial effects on gram-negative and gram-positive bacteria, yeasts, and fungi. EDTA also has been shown to induce antioxidants and anti-inflammatory activities.18
A recent study by Ricucci, et al.,19 found that a clinical pulpal diagnosis of a normal pulp or reversible pulpitis had a 96.6% histological match to the actual pulp tissue in a tooth, whereas in pulp diagnosis of symptomatic irreversible pulpitis, it only had an 84.4% histological correlation to the actual pulp tissue. This study noted that bacterial invasion of the pulp tissue was common in teeth diagnosed with irreversible pulpitis, but was absent in teeth diagnosed with a normal pulp or reversible pulpitis. This research also demonstrated that when a carious lesion encroaches the pulp that is diagnosed as normal or reversible pulpitis, that only the coronal portion of the pulpal tissue immediately adjacent to the caries showed signs of inflammation and not the entire pulp tissue as previously thought.19 Therefore, the clinician can treat the carious exposed or indirect pulp tissue with a pulp cap procedure and does not need to perform a partial or full pulpectomy.
It is important to note that pulpal bleeding can be a clinical marker for the extent of the pulpal inflammation.20 In pulps that have a pretreatment diagnosis of normal or reversible pulpitis, the hemorrhaging tends to be stagnated and easily controlled with the application of ice. In clinical cases that have a pretreatment pulpal diagnosis of symptomatic irreversible pulpitis and, clinically, the caries has entered the pulp chamber on a treatment tooth, the hemorrhaging tends to be greater due to an increase in pulpal inflammation. According to the Ricucci, et al.,19 they found that unlike a clinical pulpal diagnosis of normal or reversible pulpitis, pulps with a pretreatment symptomatic irreversible pulpitis diagnosis, the coronal portion under the decay can demonstrate necrosis, bacterial infection, and increased signs of inflammation.
Therefore, if the bleeding is profuse, the clinician needs to perform a partial pulpectomy to remove the inflamed pulp tissue immediately under the carious dentinal exposure. This can be accomplished with a spoon excavator in order to remove the pulpal tissue while minimizing the tissue trauma that can occur with the use of a high-speed bur. After the partial pulpectomy is performed, the shaved sterile water ice should be placed over the direct pulp exposure until the bleeding is controlled. If the pulp continues to bleed, it means one of two things: First, the practitioner needs to remove more coronal pulpal tissue because the inflammation of the pulp has spread more apically; or second, the sterile water ice needs to be placed for a longer period of time for hemostasis to occur due to the advancement of the inflammation of the pulpal tissue. The clinician can also use epinephrine-soaked cotton pellets to assist in the pulpal hemostasis.
If upon access of a tooth having a pretreatment pulpal diagnosis of symptomatic irreversible pulpitis, the bleeding is stagnated, the pulpal diagnosis is considered clinically reversible pulpitis, and the pulp should be treated the same as if the pretreatment diagnosis is normal or reversible. This correlates with the Ricucci, et al., study19 that reported there is a 15.6% chance a tooth with a pretreatment pulpal diagnosis of symptomatic irreversible pulpitis is clinically a reversible pulpitis.
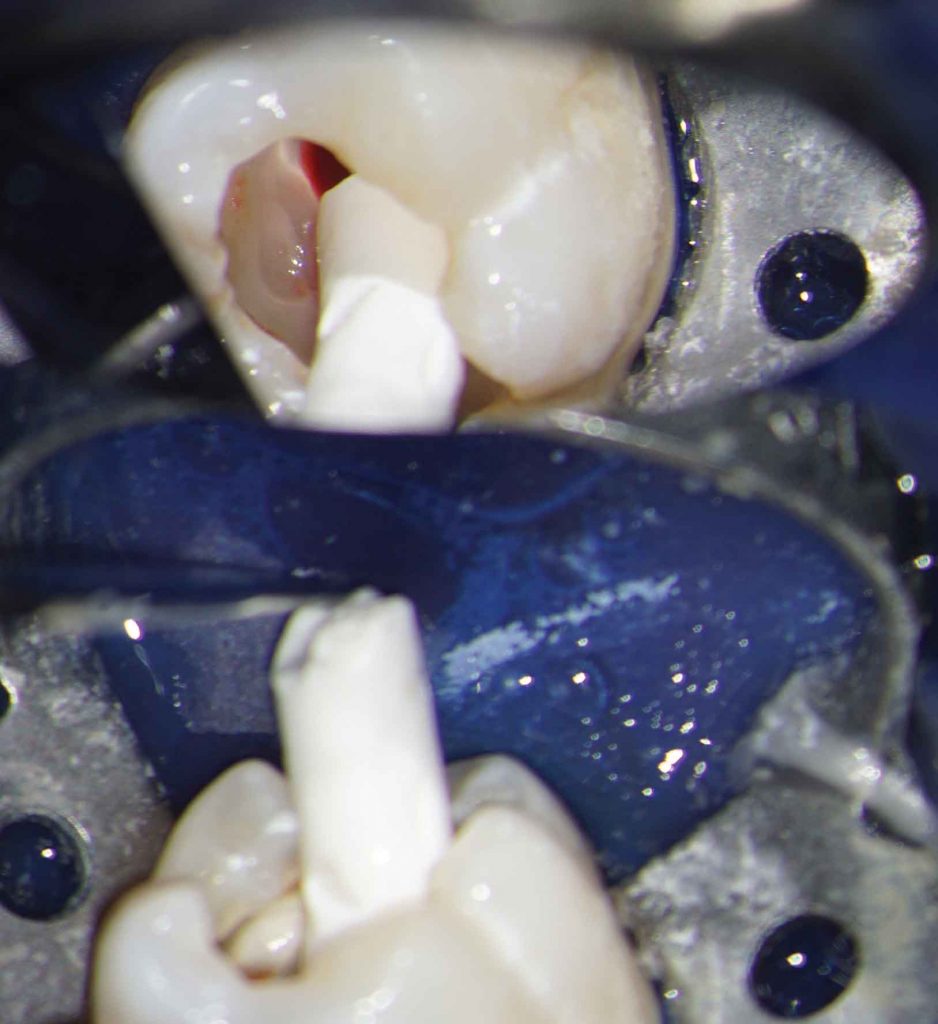
After the exposed or indirect exposed pulp has been treated with shaved sterile ice and EDTA, it is then covered with a bioceramic material: EndoSequence® BC RRM (Root Repair Material) (Brassler USA, Savannah, Georgia) or Biodentine® (BD; Septodont, Saint-Maurdes-Fossés, France) (Figure 3). In a study by Miller, et al.,21 they reported that EndoSequence BC Root Repair Material-Putty (ES; Brasseler, Savannah, Georgia) and Biodentine (BD; Septodont, Saint-Maurdes-Fossés, France) are a better coronal barrier material for vital pulp therapy due to their excellent biocompatibility with stem cells and significantly greater odontoblastic potential than MTA (mineral trioxide aggregate). They state a possible reason for this is that MTA has a high calcium ion release and sustained high pH.
Bioceramics (BC) or calcium silicate-based materials are biocompatible, non-toxic, and non-shrinking and are usually stable within a biological environment. Further advantages of these BC materials are their ability to form calcium hydroxide and hydroxyapatite.22

After performing a BC pulp cap or partial pulpectomy, a light-cured glass ionomer material (Vitrebond™, 3M ESPE, Saint Paul, Minnesota) or non-light-cured glass ionomer material (Ketac™, 3M ESPE, Saint Paul, Minnesota) should be placed directly over the BC pulp cap or partial pulpectomy.23 After this step, a permanent restoration (a composite or amalgam) is placed. A final periapical and bitewing radiograph is then taken after the permanent restoration is in place and the rubber dam has been removed (Figure 4).
The patient should then be placed on 2-week recall. In a study by Linu, et al.,24 they reported that all vital pulp therapy failure occurred in the first 2 weeks after treatment. They also noted that the teeth that remained asymptomatic at the 2-week failure point remained asymptomatic, vital, and functional over the follow-up period of 12 to 18 months. Early clinical failures (within 2-weeks) are multifactorial but certainly can be related to an improper pretreatment pulpal diagnosis.23 If the patient presents within the first 2 weeks or any time after the 2-week period in which a vital pulp cryotherapy treatment has been performed with a symptomatic irreversible pulpitis, which has either not resolved or arose as a result of treatment, a necrotic pulp, asymptomatic apical periodontitis, or chronic/acute apical abscesses, it is recommended to re-evaluate the tooth for conventional endodontic treatment.
Summary
A new vital pulp cryotherapy technique that incorporates the use of cryotherapy, EDTA, bioceramics, and a composite or amalgam permanent restoration on an exposed or indirect exposed pulp tissue was demonstrated in this article. After performing a vital pulp cryotherapy procedure, the patient should be placed on 2-week recall to evaluate postoperative pain. If the patient presents within the first 2 weeks or any time after the 2-week period in which a vital pulp cryotherapy treatment has been performed with either no change in preoperative pain, the development of postoperative pain, or the pulp has become necrotic, the treatment tooth should be re-evaluated for conventional endodontic treatment. Further clinical studies need to be conducted to observe the long-term prognosis of a pulp after undergoing vital pulp cryotherapy.
Acknowledgments
The authors would like to thank Drs. Doris Basali, Vikash Hullyar, and Gail Tischke, second-year endodontic residents at the University of Illinois at Chicago College of Dentistry, for the clinical treatment and documentation of vital pulp cryotherapy procedures.
Dr. Bahcall has shared his valuable insights with Endodontic Practice US readers on other issues as well. Read his other article, “A new expandable NiTi file for residual canal debris removal” here.
- Vera J, Ochoa-Rivera J, Vazquez-Carcaño M, Romero M, Arias A, Sleiman P. Effect of intracanal cryotherapy on reducing root surface temperature. J Endod. 2015;41(11):1884-1887.
- Hubbard TJ, Denegar CR. Does cryotherapy improve outcomes with soft tissue injury? J Athl Train. 2004;39(3): 278-279.
- Modabber A, Rana M, Ghassemi A, Gerressen M, Gellrich NC, Hölzle F, Rana M. Three-dimensional evaluation of postoperative swelling in treatment of zygomatic bone fractures using two different cooling therapy methods: a randomized, observer-blind, prospective study. Trials. 2013;14:238.
- Laureano Filho JR, de Oliveira e Silva ED, Batista CI, Gouveia FM. The influence of cryotherapy on reduction of swelling, pain and trismus after third-molar extraction: a preliminary study. J Am dent Assoc. 2005;136(6): 774-778.
- Gundogdu EC, Arslan H. Effects of various cryotherapy applications on postoperative pain in molar teeth with symptomatic apical periodontitis: a preliminary randomized prospective clinical trial. J Endod. 2018;44(3):349-354.
- Shiel W, Helm S. Cryotherapy in pain management. MedicineNet. https://www.medicinenet.com/cryotherapy/article.htm. Accessed November 11, 2018.
- Vera J, Ochoa J, Romero M, Vazquez-Carcaño M, Ramos-Gregorio CO, Aguilar RR, Cruz A, Sleiman P, Arias A. Intracanal cryotherapy reduces postoperative pain in teeth with symptomatic apical periodontitis: a randomized multicenter clinical trial. J Endod. 2018;44(1):4-8.
- Keskin C, Özdemir Ö, Uzun İ, Güler B. Effect of intracanal cryotherapy on pain after single-visit root canal treatment. Aust Endod J. 2017;43(2):83-88.
- Taha NA, Ahmad MB, Ghanim A. Assessment of Mineral Trioxide Aggregate pulpotomy in mature permanent teeth with carious exposures. Int Endod J. 2017; 50(2):117-125.
- Taha NA, Khazali MA. Partial pulpotomy in mature permanent teeth with clinical signs indicative of irreversible pulpitis: a randomized clinical trial. J Endod. 2017; 43(9):1417-1421.
- Kim S. Neurovascular interaction in the dental pulp in health and inflammation. J Endod. 1990;16(2):48-53.
- Bahcall J, Xie Q. Clinically Enhancing Local Anesthesia Techniques For Endodontic Treatment. Compend Contin Educ Dent. 2017;38(2):80-84.
- Casagrande L, Demarco FF, Zhang Z, Araujo FB, Shi S, Nör JE. Dentin-derived BMP-2 and odontoblast differentiation. J Dent Res. 2010;89(6): 603-608.
- Galler KM, Buchalla W, Hiller KA, Federlin M, Eidt A, Schiefersteiner M, Schmalz G. Influence of root canal disinfectants on growth factor release from dentin. J Endod. 2015;41(3):363-368.
- Witherspoon DE. Vital pulp therapy with new materials: new directions and treatment perspectives—permanent teeth. J Endod. 2008; Jul; 34(7 Suppl):S25-28.
- Cao Y, Song M, Kim E, Shon W, Chugal N, Bogen G, Lin L, Kim RH, Park NH, Kang MK. Pulp-dentin regeneration: current state and future prospects. J Dent Res. 2015;94(11):1544-1551.
- Finnegan S, Percival S. EDTA: An antimicrobial and antibiofilm agent for use in wound care. Adv in Wound Care. 2015;4(7):415-421.
- González-Cuevas J, Navarro-Partida J, Marquez-Aguirre AL, Bueno-Topete MR, Beas-Zarate C, Armendáriz-Borunda J. Ethylenediaminetetraacetic acid induces antioxidant and anti-inflammatory activities in experimental liver fibrosis. Redox Rep. 2011;16(2): 62-70.
- Ricucci D, Loghin S, Siqueira JF Jr. Correlation between clinical and histological diagnoses. J Endod. 2014;40(12):1932-1939.
- Matsuo T, Nakanishi T, Shimizu H, Ebisu S. A clinical study of direct pulp capping applied to carious-exposed pulps. J Endod. 1996;22(10):551-556.
- Miller AA, Takimoto K, Wealleans J, Diogenes A. Effect of 3 bioceramic materials on stem cells of the apical papilla proliferation and differentiation using a dentin disk model. J Endod. 2018;44(4):599-603.
- Brizuela C, Ormeño A, Cabrera C, Cabezas R, Silva CI, Ramírez V, Mercade M. Direct pulp capping with calcium hydroxide, mineral trioxide aggregate, and biodentine in permanent young teeth with caries: a randomized clinical trial. J Endod. 2017;43(11):1776-1780.
- Wang Z. Bioceramic materials in endodontics. Endodontic Topics 2015;32(1): 3- 30.
- Linu S, Lekshmi MS, Varunkumar VS, Sam Joseph VG. Treatment outcome following direct pulp capping using bioceramic materials in mature permanent teeth with carious exposure: a pilot retrospective study. J Endod. 2017;43(10):1635-1639.
Stay Relevant With Endodontic Practice US
Join our email list for CE courses and webinars, articles and more..


