Drs. Fernando Goldberg, Denise Alfie, Juan Pablo Miraglia, Carlos Cantarini, and Gonzalo Garcia illustrate a case of internal root resorption, an interesting and challenging inflammatory condition.
Drs. Fernando Goldberg, Denise Alfie, Juan Pablo Miraglia, Carlos Cantarini, and Gonzalo Garcia discuss treatment for an inflammatory condition
Introduction
According to the American Association of Endodontists,1 internal root resorption (IRR) is a unique entity, unlike external root resorption, which can take different shapes. For IRR to occur, a damage or loss of the predentin and odontoblast layer must precede it, leaving the mineralized dentin wall exposed.2,3 A chronic pulpal inflammation is an additional factor needed to activate the action of the clastic cells on the dentin wall triggering its resorption. For the IRR to start, part of the pulp tissue must be vital to provide the clastic cells responsible for the resorption (active resorption).
This chronic inflammatory condition progresses until the pulp is removed or becomes totally necrotic, and at that point, the resorption ceases (inactive resorption). Haapasalo and Endal3 reported that the progress of internal root resorption is dependent on two things: 1) the pulp tissue at the resorption area must be vital, and 2) the pulp coronal to the resorption must be partially or completely necrotic, allowing bacterial infection and microbial antigens to enter the root canal. If the progression of the infection is slow and the necrosis of the whole pulp takes time, the IRR can continue and create a communication between the root canal and the surrounding periodontium, complicating the treatment with a poor prognosis. The IRR can be very small and radiographically not visible or produce a noticeable cavity of different shapes and sizes, generally with symmetrical walls, which appears as a radiolucent area that deforms the dentin wall.
In the radiographic image, the internal resorption cavity continues with the walls of the root canal. In contrast, in the case of an external resorption, the original shape of the canal remains radiographically intact because the resorption only projects over the root canal. The prevalence of IRR is very low. Haapasalo and Endal3 suggest that this prevalence is between 0.01% and 1%, and it can be in any third of the root canal. Patel, et al.,4 detail several etiological factors proposed as antecedents of IRR: trauma, caries, periodontal infections, excessive heat generated during restorative procedures on vital teeth, orthodontic treatment, etc.
There is always a determining factor that is the reason for its initiation. However, the advancement of internal root resorption depends on bacterial stimulation. Patel, et al.,4 emphasize that without this stimulation, the resorption will be self-limiting.
Wedenberg and Lindskog5 divide IRR into two types: transient and progressive. The authors mention that the transient type develops in the absence of pulpal infection, while the progressive type requires continuous stimulation by bacterial inflammation.
Many lesions are found accidentally during routine checkup radiographs, as teeth with internal resorption are typically symptom- free, and in cases of doubt, the CBCT can be of great help to clarify the diagnosis.6,7
Purpose
The purpose of this article is to analyze morphological and therapeutic aspects of IRR in different clinical situations.
Materials and methods
This study was performed with the approval of the Ethics Committee of the Department of Coordination of General Research of the Argentinian Dental Association (resolution number 0422). The STROBE (Strengthening the Reporting of Observational Studies in Epidemiology) checklist and statement were followed.
Periapical radiographs and medical records corresponding to 48 teeth with IRR were collected from five different dental offices. The following aspects of the IRR were then analyzed: number of tooth in which it was found, location, presence or absence of periapical radiolucency, shape of the affected dentin walls, type of treatment performed, filling technique used, degree of adaptation of the filling to the resorption, presence of perforation communicating with the periodontium. Of the 48 cases diagnosed with IRR, all have been endodontically treated, and 29 of them have received initial treatments and 19 retreatments. Of the total number of cases, 29 had long-term follow-ups, while 19 do not have them.
The observations of the different aspects analyzed were carried out by five specialists in endodontics, and data were tabulated.

Results
The results of the items proposed in materials and methods are described in Tables 1 and 2.
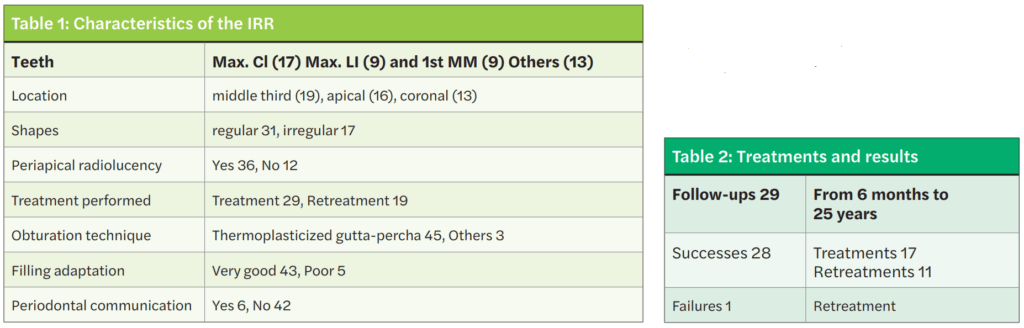
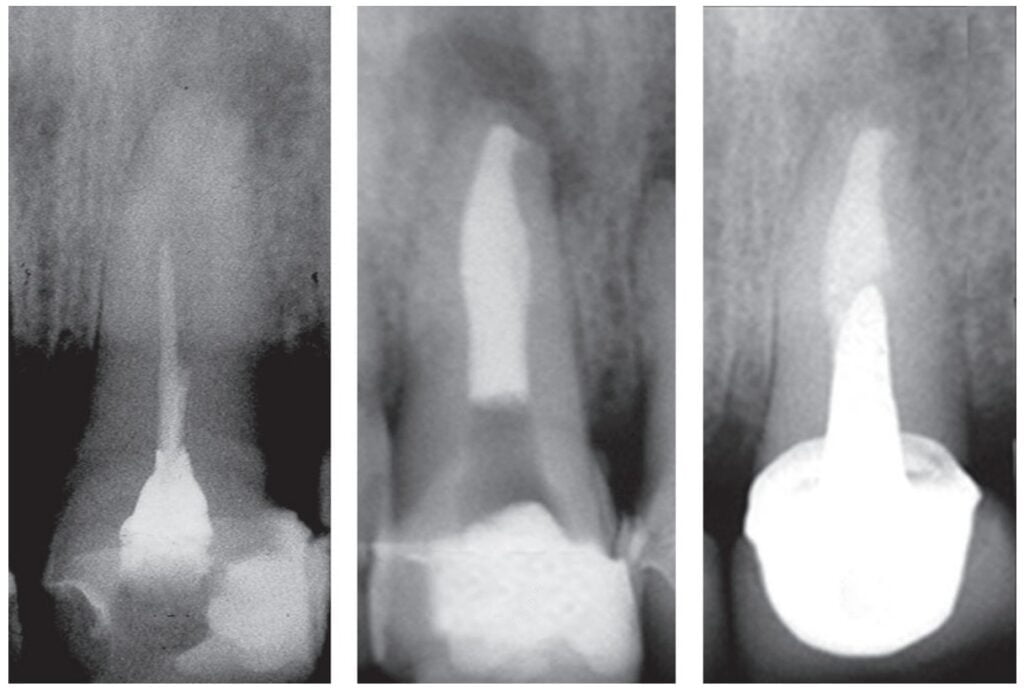
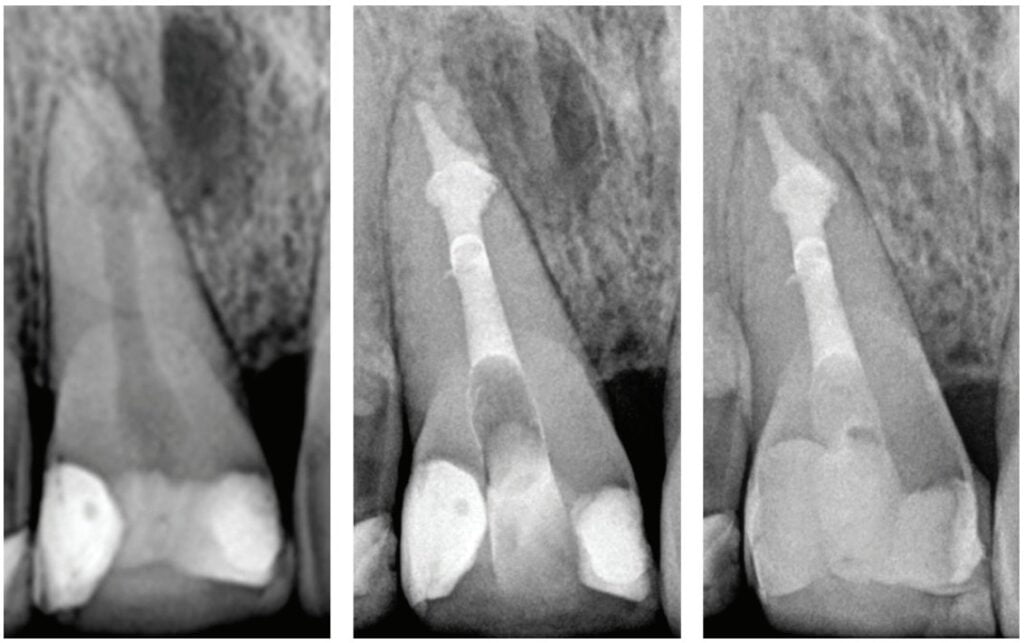
Of the total, 29 had long-term radiographic follow-ups that ranged from a minimum of 6 months to a maximum of 25 years, with an average of 5 years, 4 months. Of the cases with radiographic follow-ups, 28 were considered successful and one failure (Table 2). Of the successful cases, 17 corresponded to treatments and 11 to retreatments (Figures 1A, 1B, 1C, and 2A, 2B, 2C). The tooth considered failed was a retreatment.
Discussion
IRR is a disease of the dental pulp that affects the dentin wall, which is reabsorbed by clastic action. It can occur in any tooth, although its presence is more frequent in those more susceptible to different kind of trauma. According to what was observed in this study, the upper incisors and the lower first molars are the most likely to present IRR, and this could be since the former are the ones that often suffer traumatic injuries, while the lower molars suffer more the action of orthodontic forces (Figures 3A, 3B, 3C).

The results of the present retrospective study are consistent with previous findings.8 Çaliişkan and Türkün8 reported that the most affected teeth with IRR were the upper incisors and agreed that the middle-third of the root was the area where it was located most frequently after an evaluation of 28 cases.
The radiographic appearances that generates the IRR are varied. The most common one observed in the present study was a circular shape with regular and symmetrical walls specially in single-rooted teeth (Figure 4A), although there were also some irregular ones with asymmetrical walls (Figure 4B). In molars, when resorption affects the pulp chamber, it was commonly seen as an irregularly shaped radiolucent cavity2 (Figure 4C).

Most of the IRR develop without clinical symptoms, although as they progress, necrosis of the pulpal tissue may progress, and pulpal symptoms become noticeable.3
When the IRR is diagnosed, root canal treatment is the treatment of choice. The prognosis is, in general, very good except when the resorption has perforated the dentin wall connecting the root canal with the periodontium.3,4,8 In many cases, this communication can’t be observed radiographically. Before performing endodontic therapy, it is always important to evaluate if the tooth is deemed restorable and what kind of reconstruction is needed. Properly cleaning and shaping the area of resorption may be very challenging because in many cases, it presents a complex access.
Different strategies have been proposed for instrumentation, such as use of sonic and ultrasonic activation of sodium hypochlorite,9,10 activation with the XP-Endo® Finisher file10 (FKG, Dentaire SA, La Chaux de Fonds, Switzerland), the use of precurved files in the RDI area,11 multiple visits using calcium hydroxide as intracanal medication, and sodium hypochlorite as irrigant in order to improve the disinfection of areas that are difficult to access.3,4 In the present study, calcium hydroxide was used as intracanal medication in only three of the 48 cases, while in 45 cases, the treatment was carried out in one single visit. However, complete removal of the calcium hydroxide used as temporary medication can be difficult in canals with normal morphology,12-14 so the situation would be aggravated in teeth with IRR given the difficulty of removing it from the retentive cavity of the resorption. Topçuoğlu, et al.15 and Marques-da-Silva, et al.16 used different irrigation techniques in simulated IRR, observing that none of them completely removed the calcium hydroxide from the resorptive cavities.
Regarding the obturation, the best results were observed with the use of thermoplasticized gutta-percha injection techniques.3,4,8,17-20 In this study, a thermofluid gutta-percha technique was used in 45 teeth, presenting adequate filling adaptation to the dentin walls in 43 of those cases. It is important to highlight the studies by Ulusoy, et al.,21 who mention that the ex vivo use of System B™ and Obtura II in IRR fillings produced a temperature increase above the critical limit. In any case, these authors consider that the few seconds of thermal increase and the cooling action of the periodontium ligament in vivo would be a barrier to avoid thermal damage.
When the IRR communicates with the periodontium area, MTA, Biodentine® (Septodont USA) or similar product is the filling of choice,3,4 (Figures 5A, 5B, 5C).
Conclusions
The prevalence of IRR was higher in the upper incisors and lower molars, being located predominantly in the middle and apical thirds of the root canal. Its walls are generally regular and continuous. The use of thermoplasticized gutta-percha techniques allowed the adequate filling of the IRR cavities. Root canal treatment and retreatment provided adequate conditions to achieve a successful outcome.
Dr. Cameron Howard discusses the importance of CBCT in endodontics in his article, “Resorption: one of dentistry’s big mysteries,” at https://endopracticeus.com/resorption-one-dentistrys-big-mysteries/.
- American Association of Endodontists, Communique, By Blicher B. Differentiating resorption January 2021;5:1-5.
- Tronstad L. Root resorption-etiology, terminology, and clinical manifestations. Endod Dent Traumatol. 1988;4:241-252
- Haapasalo M, Endal U. Internal inflammatory root resorption: the unknown resorption of the teeth. Endod Topics. 2006;14:60-79.
- Patel S, Ricucci D, Durak C, Tay F. Internal root resorption: a review. J Endod. 2010;(36)7:1107-1121.
- Wedenberg C, Lindskog S. Experimental internal resorption in monkey teeth. Endod Dent Traumatol. 1985;1:221-227.
- Patel S, Dawood A, Wilson R, Horner K, Mannocci F. The detection and management of root resorption lesions using intraoral radiography and cone beam computed tomography: an in vivo investigation. Int Endod J. 2009;42(9):831-838
- Kamburoğlu K, Kurşun Ş, Yüksel S, Öztaş B. Observer ability to detect ex vivo simulated internal or external cervical root resorption. J Endod. 2011;37(2):168-175.
- Çaliişkan MK, Türkün M. Prognosis of permanent teeth with internal resorption: a clinical review. Endod Dent Traumatol. 1997;13(2):75-81.
- Stamos DE, Stamos DG. A new treatment modality for internal resorption. J Endod. 1986;12(7):315-319.
- Hernandez Restrepo C, García G, Alfie D, Oyhanart SR, Goldberg F. Efficacy of different procedures in removing radiopaque organic material from simulated internal root resorption cavities: an ex vivo study. Endod Practice US. 2020;13:24-27.
- Manzur E. Evaluación in vitro de diferentes técnicas para la instrumentación de reabsorciones dentinarias internas simuladas. Rev Asoc Odontol Argent. 2003;63(5-6):107-111.
- Wiseman A, Cox TC, Paranjpe A, et al. Efficacy of Sonic and Ultrasonic Activation for Removal of Calcium Hydroxide from Mesial Canals of Mandibular Molars: A Microtomographic Study. J Endod. 2011;37(2):235-28.
- Alturaiki S, Lamphon H, Edrees H, Ahlquist M. Efficacy of 3 different irrigation systems on removal of calcium hydroxide from the root canal: a scanning electron microscopic study. J Endod. 2015;41:97-101.
- Zorzin J, WieBner J, WieBner T, et al. Removal of radioactively marked calcium hydroxide from the root canal: influence of volume of irrigation and activation. J Endod. 2016;42(4):637-40.
- Topçuoğlu HS, Düzgün S, Ceyhanlı KT, et al. Efficacy of different irrigation techniques in the removal of calcium hydroxide from simulated internal root resorption cavity. Int Endod J. 2015;48:309-16.
- Marques-da-Silva B, Alberton CS, Tomazinho FSF, et al. Effectiveness of five instruments when removing calcium hydroxide paste from simulated internal root resorption cavities in extracted maxillary central incisors. Int Endod J. 2020;53(3):366-375.
- Goldberg F, Massone EJ, Esmoris M, Alfie D. Comparison of different techniques for obturating experimental internal resorptive cavities. Endod Dent Traumatol. 2000;16(1):116-1121.
- Goldberg F, Manzur E, Mignanelli ME. Estudio comparativo entre diferentes técnicas para la obturación de reabsorciones internas creadas artificialmente. Rev Asoc Odontol Argent. 2001;89:125-1259.
- Gencoglu N, Yildirim T, Garip Y, Karagenc B, Yilmaz H. Effectiveness of different gutta-percha techniques when filling experimental internal resorptive cavities. Int Endod J. 2008;41(10):836-842.
- Keles A, Ahmetoglu F, Uzun I. Quality of different gutta-percha techniques when filling experimental internal resorptive cavities: A micro-computed tomography study. Aust Endod J. 2013;40:131-135.
- Ulusoy ÖI, Yilmazoglu Z, Görgül. Effect of several thermoplastic canal filling techniques on surface temperature rise on roots with simulated internal resorption cavities: an infrared thermographic analysis. Int Endod J. 2015,48(2):171-176.
Stay Relevant With Endodontic Practice US
Join our email list for CE courses and webinars, articles and more..


