CE Expiration Date:
CEU (Continuing Education Unit): Credit(s)
AGD Code:
Educational aims and objectives
This clinical article aims to examine the beneficial aspects of a certain bioceramic sealer.
Expected outcomes
Endodontic Practice US subscribers can answer the CE questions by taking the quiz to earn 2 hours of CE from reading this article. Correctly answering the questions will demonstrate the reader can:
- Identify some previous research on BC HiFlow Sealer.
- Identify some functional characteristics of this particular bioceramic sealer.
- Realize the importance of sealers as a needed component of a successful RCT fill.
- Recognize differences in single-cone obturation when using BC Sealer compared to lateral condensation.
Dr. Stephen Buchanan discusses the advantageous properties of this bioceramic sealer
I just changed the sealer that I use in practice after successfully using Kerr Pulp Canal Sealer (KPCS) for 40 years — for an endodontist, this is a big move.
If you asked endodontists what part of their RCT procedure they are least willing to change, a majority of them would say they are most anxious about changing their filling materials because that is the greatest long-term risk to an endodontic specialty practice. If you change filling materials because somebody convinced you that the new sealer is better because of the customary reasons, or if you are a typical endodontist who does 800-1,000 cases a year, and the new material starts failing after 3 years, you could have thousands of cases coming back to haunt you! Practices have failed over less.
Although this may sound like an over-dramatization, it is not. The last new obturation material to flame-out was Resilon®, a polycaprolactone-based endodontic composite filling material.1 Designed by Pentron Dental to replace traditional gutta percha and sealers, this insidious material began failing after 6 years, doubling the failures in the preceding example because, over the additional 3 years, 3,000 more cases were treated with it before the backlash. Let’s be conservative and say the fees averaged $500 per RCT. $500 X 3,000 potential failures = $1,500,000 of liability. And that one is not a made-up number.
What would convince me to change from the sealer I’ve successfully used with my Continuous Wave (CW) Obturation Technique for 40 years? Am I throwing Rickert’s sealer (KPCS) — formulated over a century ago — over for a new trophy sealer? Absolutely not.
I changed to BC HiFlow Sealer (Brasseler USA®, Savannah, Georgia) because our best researchers have proved all of Brasseler’s claims for more than a decade. Drs. Spangberg, Haapasalo, Kim, Setzer, Kohli, and scores of others have shown BC Sealer to be completely biocompatible to pulp cells,2-15 to be an excellent pulp capping agent that incites odontoblastic proliferation, mineralization, and osteogenesis,9-11,15-19 and somehow, at the same time, this bio-ceramic material has significant anti-bacterial properties20-22 — all of this in a material that seals like MTA23-30 but doesn’t stain dentin.31-34
I changed to this sealer because Brasseler reformulated BC Sealer™ to meet my warm gutta-percha obturation needs. The new BC HiFlow Sealer (Figure 1) was designed for higher heat resistance (good to 220ºC), and it also has 20% greater radio-opacity.
I changed to this sealer because the functional characteristics of these bioceramic materials profoundly change everything in endo obturation — in more ways than first meets the eye.
This changes everything
The literature tells us that BC Sealer has a slight (0.2%) net expansion when it sets,35 instead of the significant shrinkage (up to 6.5% for AH+) seen in all sealers before. How does this change things in profound ways? As a practitioner, I value this sealer because it streamlines Continuous Wave Obturation36 (CW), increasing my practice productivity. As an educator, I value this sealer because it simplifies the technique, making warm gutta-percha obturation more accessible to dentists of all skill and experience levels.

The most complex parts of traditional warm gutta-percha condensation methods have always been:
1. The need to downpack within 4 mm-6 mm of the terminus, even when obturating small, curved molar canals.
2. Syringe backfilling these narrow spaces without leaving voids.

Continuous Wave Obturation — with its dead-soft stainless steel electric heat pluggers (elements™Free; by Kerr Endodontics, Orange, California) and its nickel-titanium hand pluggers (Buchanan Pluggers also by Kerr Endodontics) — enables clinicians to downpack within 4 mm-6 mm of the end of most any small, curved canal — a huge improvement over the Schilder technique with its rigid pluggers. However, the CW technique, as done with traditional sealers, requires pre-fitting the electric heat pluggers in the canals before cementing the master cone in the canal with sealer. This pre-fitting routine is done by pressing the appropriate size plugger into the canal as it is rocked back and forth. This rocking action causes the plugger to work its way into the canal; in the process, the canal very accurately bends the plugger to match its curvature (Figure 2A). It was this improvement that enabled a much deeper downpack than the Schilder Warm Vertical Technique, while filling all lateral canals in less than 2 seconds (Figure 2B).
Why have clinicians felt compelled to downpack that far into the canal? Sealers are a needed component of a successful RCT fill, as gutta percha is not an effective sealing medium; however, all conventional sealers shrink as they set. Because of this sealer shrinkage, clinicians’ best procedural workaround to prevent this shrinkage from pulling the sealer off canal walls, has been to downpack deeply into even small curved canals to thermo-plastically move the heat-softened gutta percha into the intaglio of the canal, thereby thinning the sealer layer.
This is a well thought-out procedure, considering previous sealer constraints; however, this is also setup to backfilling voids. Despite voids being clinically the least important part of the CW procedure, seeing a backfill void on a post-RCT radiograph leaves clinicians with disappointment instead of the “thrill of the fill.”
Good riddance to lateral condensation
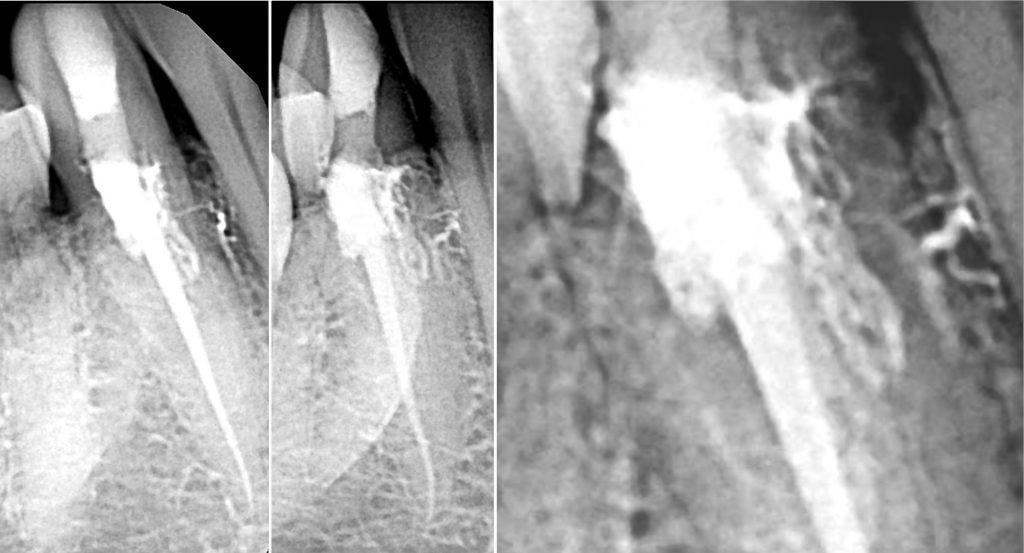
Change 6.5% shrinkage to 0.2% expansion, and suddenly nobody cares how thick the sealer layer is; clinicians only care if they can move it into all the lateral irregularities that have been cleaned out. Combine net expansion on setting with extremely low surface tension and high wettability,40 and suddenly we find that just a 3 mm-4 mm downpack will fill every nook and cranny in the most complicated anatomy. This pivot in the Continuous Wave Obturation procedure simplifies the downpack as electric heat pluggers no longer need to be prefit and bent before cementing master cones. This reduced need to achieve depth in the downpack also means it is much easier to backfill without voids.
An easy way to explain the importance of the wetting characteristics of BC HiFlow Sealer over traditional sealers is to consider the difference in technique sensitivity between flowable and traditional composite materials. This surprising ability of BC Sealer to flow into lateral spaces with very little pressure needed has significantly changed the dynamic around cold gutta-percha filling techniques in general practices. Dr. Herbert Schilder was known to say, “Lateral condensation of cold gutta percha is single-cone technique with a conscience.” Now we can say that single-cone obturation with BC Sealer is far better than lateral condensation because:
1. This sealer will fill the primary canal next to the master cone and lateral canals 1 mm-2 mm long by simply cementing the master cone into a BC Sealer-laden canal (Figure 3).
2. Lateral condensation of cold gutta percha requires over-cutting coronal canal shapes, so a spreader (basically a thin wedge) can be forced into the canal (an enormous root-splitting force) to push the master cone aside and allow an inconsequential accessory cone to be placed in that space.
For these reasons, lateral condensation of cold gutta percha — a technique that requires the weakening of teeth to allow a filling method that doesn’t improve the result — should be extinct. It is a technique without rationale.
Continuous Wave Obturation 2.0
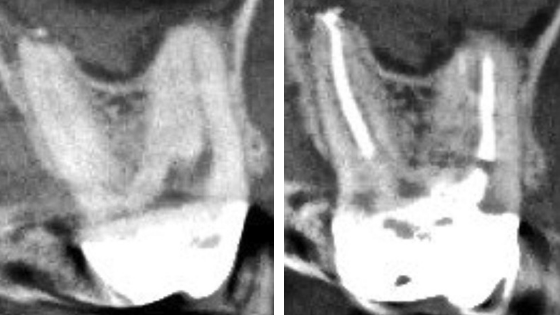
If BC Sealer fills lateral canals 1 mm-2 mm in length when doing single-cone obturation, why do we need to heat gutta percha and downpack at all? Unfortunately, lateral canal spaces in molars are way bigger than that. Forget about the 4 mm-wide isthmus forms found in mesial roots of lower molars. Forget about the fins, webs, loops, and lateral canals that commonly project off of single primary canals. Be worried about MB2 and MB3 canals in upper molars that bifurcate midroot off the MB1, turn 90º, and bifurcate before exiting (Figures 4A and 4B). These can be 7 mm-8 mm in length, so I’m still a warm gutta-percha user. With BC HiFlow Sealer, I just don’t have to work as hard to get the 3D results I expect to see on post-obturation radiographs.

How does this simplify warm gutta-percha obturation? Primarily by shortening the required downpack distance into the canal. As previously mentioned, with net expansion of bioceramic sealers, the warmed gutta percha and the sealer beneath it need just half the previous depth of Continuous Wave downpack to move sealer into the full apical and lateral extents of root canal systems (Figure 5B). The shortening of the downpack means that pluggers no longer need to be pre-fit in canals before cementation of the master cone, and it also means that backfilling can be done with a small squirt of GP from a backfill syringe, or better yet, with a sealer-coated backfill cone. (Autofit Backfill Gutta Percha, Kerr Endodontics).
BC HiFlow Sealer also works well for carrier-based obturation. A 3 mm aliquot of sealer is syringed into the orifice of each canal, an XP-Finisher (Brasseler USA®) is used to spread a thin coat of sealer on canal walls, then the oven-heated obturator is placed 1 mm short of full length. With the heat resistance of HiFlow, carrier placement with bioceramic sealer is identical to placement of carriers with traditional sealers, except patients have little or no postoperative discomfort due to BC HiFlow Sealer’s complete biocompatibility (Figure 6).
Conclusion
Changing sealers is a very important decision for an endodontist because thousands of patients could be hurt if the new sealer fails before a couple of decades go by. BC HiFlow Sealer checks all the required safety boxes such as biocompatibility, antibacterial, etc., however, the greatest advantage of this sealer (besides 10-year history of success) is its net-expansion upon setting. Single cone obturation with BC HiFlow Sealer can provide much better results than lateral condensation and will replace it as the most efficient endodontic sealing method.

References
- Barborka BJ, Woodmansey KF, Glickman GN, Schneiderman E, He J. Long-term Clinical Outcome of Teeth Obturated with Resilon. J Endod. 2017;43(4):555-560.
- Zhang W, Li Z, Peng. Ex vivo cytotoxicity of a new calcium silicate-based canal filling material. Int Endod J. 2010;43(9):769.
- Jingzhi M, Shen Y, Stojicic S, Haapasalo M. Biocompatibility of two novel root repair materials. J Endod. 2011;37(6):793-798.
- Alanezi AZ, Jiang J, Safavi KE, Spangberg LSW, Zhu Q. Cytotoxicity evaluation of endosequence root repair material. Oral Surg Oral Med Oral Path Oral Radiol Endod. 2010;109(3):122-125.
- Ruparel NB, Ruparel SB, Chen PB, Ishikawa B, Diogenes A. Direct effect of endodontic sealers on trigeminal neuronal activity. J Endod. 2014;40(5):683-687.
- Chang SW, Lee SY, Kang SK, Kum KY, Kim EC. In vitro biocompatibility, inflammatory response, and osteogenic potential of 4 root canal sealers: Sealapex, Sankin apatite root sealer, MTA Fillapex, and iRoot SP root canal sealer. J Endod. 2014;40(10):1642-1648.
- Ciasca M, Aminoshariae A, Jin G, Montagnese T, Mickel A. A comparison of the cytotoxicity and proinflammatory cytokine production of EndoSequence root repair material and ProRoot mineral trioxide aggregate in human osteoblast cell culture using reverse-transcriptase polymerase chain reaction. J Endod. 2012;38(4):486-489.
- Hirschman W, Wheater M, Bringas J, Hoen M. Cytotoxicity comparison of three current direct pulp-capping agents with a new bioceramic root repair putty. J Endod. 2012;38(3):385-388.
- Zhou HM, Du TF, Shen Y, Wang ZJ, Zheng YF, Haapasalo M. In vitro cytotoxicity of calcium silicate–containing endodontic sealers. J Endod. 2015;41(1):56-61.
- Shi ZF, Bao Y, Liu DD, Zhang X, Chen LM, Jiang, Zhong M. Comparison of in vivo dental pulp responses to capping with iRoot BP Plus and mineral trioxide Aggregate. Int Endod J. 2015;49(2):154-160.
- Öncel Torun Z, Torun D, Demirkaya K, Yavuz ST, Elçi MP, Sarper M, Avcu F. Effects of iRoot BP and white mineral trioxide aggregate on cell viability and the expression of genes associated with mineralization. Int Endod J. 2015; 48(10): 986-993.
- Liu S, Wang S, Dong Y. Evaluation of a bioceramic as a pulp capping agent in vitro and in vivo. J Endod. 2015;41(5):652-657.
- Shinbori N, Grama AM, Patel Y, Woodmansey K, He J. Clinical outcome of endodontic microsurgery that uses EndoSequence BC root repair material as the root-end filling material. J Endod. 2015;41(5):607-612.
- Chen I, Karabucak B, Wang C, et al. Healing after root-end microsurgery by using mineral trioxide aggregate and a new calcium silicate-based bioceramic material as root-end filling materials in dogs. J Endod. 2015;41(3):389-399.
- Khalil WA, Abunasef SK. Can mineral trioxide aggregate and nano-particulate EndoSequence root repair material produce injurious effects to rat subcutaneous tissues? J Endod. 2015;41(7):1151-1156.
- Zhang S, Yang X, Fan M. BioAggregate and iRoot BP Plus optimizes the proliferation and mineralization ability of human dental pulp cells. Int Endod J. 2013;46(10):923-929.
- Zhang W, Li Z, Peng B. Effects of iRoot SP (aka BC Sealer™) on mineralization-related genes expression in MG63 cells. J Endod. 2010;36(12):1978-1982.
- Machado J, DDS, Johnson JD, Paranjpe A. Effects of EndoSequence root repair material on differentiation of dental pulp cells. J Endod. 2016;42(1):101-105.
- Chen I, Salhab I, Setzer FC, Kim S, Nah HD. A new calcium silicate–based bioceramic material promotes human osteo- and odontogenic stem cell proliferation and survival via the extracellular signal-regulated kinase signaling pathway. J Endod. 2016;42(3):480-486.
- Zhang H, Shen Y, Ruse ND, Haapasalo M. Antibacterial activity of endodontic sealers by modified direct contact test against Enterooccus faecalis. J Endod. 2009;35(7):1051-1055.
- Lovato K, Sedgley M. Antibactieral activity of EndoSequence root repair material and ProRoot MTA against clinical isolates of Enterococcus faecalis. J Endod. 2011;37(11):1542-1546.
- Wang Z, Shen Y, Haapasalo M. Dentin extends the antibacterial effect of endodontic sealers against Enterococcus faecalis biofilms. J Endod. 2014; 40(4):505-508.
- Zhang W, Zhi L, Peng B. Assessment of a new root canal sealer’s apical sealing ability. Oral Sur Oral Med Oral Path Oral Radiol Endod. 2009;107(6):79-82.
- Nagas E, Uyanik MO, Eymirli A, et al. Dentin moisture conditions affect the adhesion of root canal sealers. J Endod. 2011;38(2):240-244.
- Leal F, De-Deus G, Brandao C, Luna A, Souza E, Fidel S. Similar sealability between bioceramic putty ready-to-use repair cement and white MTA. Braz Dent J. 2013;24(4):362-366.
- Ersahan S, Aydin C. Dislocation Resistance of iRoot SP (aka BC Sealer), a calcium silicate-based sealer, from radicular dentine. J Endod. 2010;36(12):2001-2002 .
- Ghoneim AG, Lutfy RA, Sabet NE, Fayyad DM. Resistance to fracture of roots obturated with novel canal-filling systems. J Endod. 2011;37(11):1590-1592.
- Jiang Y, et al. A comparative study on root canal repair materials: a cyto-compatibility assessment in L929 and MG63 Cells. Scientific World Journal. 2014.
- DeLong C, He J, Woodmansey KF. The effect of obturation technique on the push-out bond strength of calcium silicate sealers. J Endod. 2015;41(3);385-388.
- Topçuoğlu HS, Tuncay O, Karataş E, Arslan H, Yeter K. In vitro fracture resistance of roots obturated with epoxy resin–based, mineral trioxide aggregate–based, and bioceramic root canal sealers. J Endod. 2013;39(12):1630-1633.
- Keskin C, Demiryurek EO, Ozyurek T. Color stabilities of calcium silicate-based materials in contact with different irrigation solutions. J Endod. 2015;41(3);409-411.
- Kohli MR, Yamagucbi M, Setzer FC, Karabucak B. Spectrophotometric analysis of coronal tooth discoloration induced by various bioceramic cements and other endodontic materials. J Endod. 2015;41(11):1862-1866.
- Shokouhinejad N, Nekoofar MH, Pirmoazen P, Shamshiri AR, Dummer PM. Evaluation and comparison of occurrence of tooth discoloration after the application of various calcium silicate–based cements: an ex vivo study. J Endod. 2015; 42(1):140-144.
- Marconyak LJ Jr, Kirkpatrick TC, Roberts WH, et al. A Comparison of Coronal Tooth Discoloration Elicited by Various Endodontic Reparative Materials. J Endod. 2015;42(3):470-473.
- Richardson IG. The calcium silicate hydrates. Cement and Concrete Research. 2008;38(2):137-158.
- Ingle JL, et al. Continuous Wave of Obturation. In Ingle JI, Bakland LK, eds. Endondontics. 5th ed. London, England, UK: BC Decker; 2002
Stay Relevant With Endodontic Practice US
Join our email list for CE courses and webinars, articles and more..

 Stephen Buchanan, DDS, FICD, FACD, Dipl. ABE, was valedictorian of his class at the University of the Pacific School of Dentistry and completed the Endodontic Graduate program at Temple University in Philadelphia, Pennsylvania, in 1980. Dr. Buchanan began pursuing 3D anatomy research early in his career, and in 1986, he became the first person in dentistry to use micro CT technology to show the intricacies of root structure. In 1989, he established Dental Education Laboratories and subsequently built a state-of-the-art teaching laboratory devoted to hands-on endodontic instruction, where he continues to teach today. Through Dental Education Laboratories he has lectured and conducted participation courses around the world, published numerous articles, and produced an award-winning video series, “The Art of Endodontics.” In addition to his activities as an educator and practicing clinician, Dr. Buchanan holds a number of patents for dental instruments and techniques.
Stephen Buchanan, DDS, FICD, FACD, Dipl. ABE, was valedictorian of his class at the University of the Pacific School of Dentistry and completed the Endodontic Graduate program at Temple University in Philadelphia, Pennsylvania, in 1980. Dr. Buchanan began pursuing 3D anatomy research early in his career, and in 1986, he became the first person in dentistry to use micro CT technology to show the intricacies of root structure. In 1989, he established Dental Education Laboratories and subsequently built a state-of-the-art teaching laboratory devoted to hands-on endodontic instruction, where he continues to teach today. Through Dental Education Laboratories he has lectured and conducted participation courses around the world, published numerous articles, and produced an award-winning video series, “The Art of Endodontics.” In addition to his activities as an educator and practicing clinician, Dr. Buchanan holds a number of patents for dental instruments and techniques.
