CE Expiration Date:
CEU (Continuing Education Unit): Credit(s)
AGD Code:
Educational aims and objectives
The aim of this article is to describe the surgical extrusion and endodontic treatment for comminuted and complicated crown-root fractures following a young patient’s bike injury.
Expected outcomes
Endodontic Practice US subscribers can answer the CE questions to earn 2 hours of CE from reading this article. Correctly answering the questions will demonstrate the reader can:
- Realize the endodontic treatment required for comminuted crown-root fractures following dental trauma in a child, including the precautions and sensitivities.
- Realize some clinical characteristics of an injury of this type.
- Realize some treatments options for treatment for an injury of this type.
Dr. Judy McIntyre describes endodontic treatment for comminuted and complicated crown-root fractures after trauma
An 11-year-old female patient presented to a pediatric dental clinic having reported a bike injury the day prior. The pediatric dental examination concluded that both UR1 and UL1 were in need of endo-dontic treatment, and as a result, I was contacted. Clinical examination revealed an over-the-counter dental temporary material over both UR1 and UL1, which had been placed by a resourceful neighbor (Figure 1). Radiographs of UR1 and UL1, as well as the lower anterior incisors, were also taken (Figures 2A-2F) (DiAngelis, et al., 2012; American Association of Endodontists, 2013; Andreasen, Andreasen, Andersson, 2007). The patient was in good spirits and denied any loss of consciousness. She did have a contusion on her forehead consistent with that of a bike injury. Clinically, there was very little coronal tooth structure remaining on either UR1 or UL1. Her lateral incisors (UR2 and UL2) were completely intact and fully erupted. Her canines had not yet erupted; however, she did have premolars present.
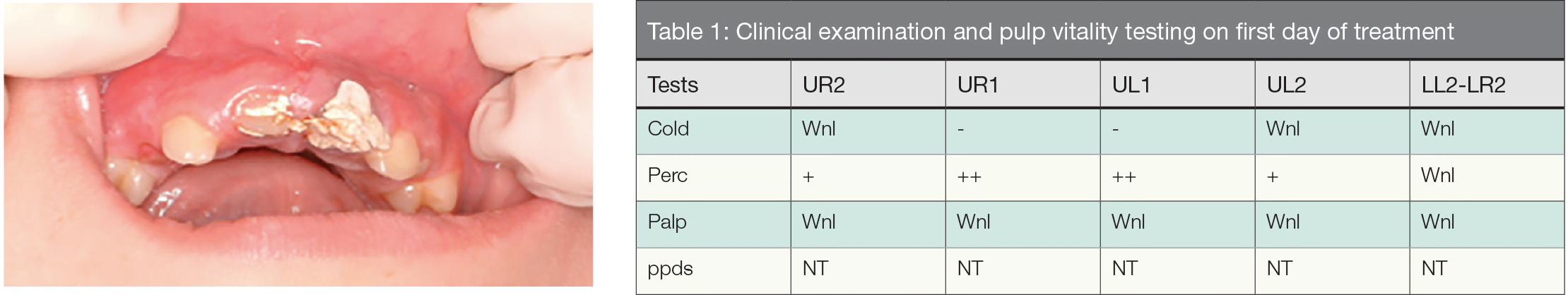
Figure 1: Patient at time of presentation. No treatment yet performed | Wnl = within normal limits NT = not taken

Figures 2A-2C: Preoperative radiographs; 1-day post-traumatic injury. Several angled films were indicated; the extent of coronal and coronal/root fractures revealed. Pulpally and periodontally, these would be considered our “baseline” radiographs, unless the patient could provide very recent photographs showing these same teeth

Figures 2D-2F: “Baseline” angled radiographs of the patient’s mandibular anteriors. As the injury was on the opposing arch, it is recommended to take images on the opposing teeth (of injury site) to rule out any other incidental and concomitant dental injuries. Angled images of the mandibular anterior teeth were repeated throughout the follow-up period; all of those images were within normal limits and showed no changes pulpally or periodontally. We would suspect and be looking for visual changes along or within the root surfaces to be able to trace the periodontal ligament, and for any changes in the pulpal space getting smaller, indicating pulp canal obliteration
Treatment this first day consisted of removing the dental temporary and visualizing the extent of the traumatic dental injury, as well as ruling out any other dental injuries that could have possibly been sustained on adjacent or opposing teeth (DiAngelis, et al., 2012; American Association of Endodontists, 2013; Andreasen, Andreasen, Andersson, 2007). Many clinicians in this emergency scenario might possibly forget to consider any injury to the opposing arch. It is an important reminder that traumatic dental injuries are rarely a focal point of contact but rather a larger area of impact, thereby clinically affecting multiple teeth to varying extents — even ones in the opposing arch. Clinical examination and pulp vitality testing at that time is shown in Table 1.
Diagnosis and treatment
As such, the diagnosis for UR1 was irreversible pulpitis and pulp exposure, and for UL1, irreversible pulpitis secondary to traumatic dental injury; the periodontal diagnosis for both teeth was acute apical periodontitis. Traumatic diagnosis for both UR1 and UL1 were comminuted and complicated (involving the pulp) coronal and root fractures. UR2 and UL2 exhibited possible dental subluxations as they were slightly percussion positive. For documentation and future treatment, it is highly recommended to document a trauma diagnosis to the best of one’s ability as well as the pulpal and periodontal diagnosis (DiAngelis, et al., 2012; American Association of Endodontists, 2013; Andreasen, Andreasen, Andersson, 2007). A clinician can always revise the trauma diagnosis later (if more involved than originally suspected), but this baseline diagnosis will serve everyone well for treatment planning as well as prognosis.
Risks, benefits, and options were discussed with the parents (Andreasen, et al., 1995; Kinirons, et al., 2000). It was agreed that root canal therapy would commence this first treatment day. Without incident, the patient was extremely cooperative, and the pulps of both UR1 and UL1 were extirpated — without rubber dam isolation, but instead with cotton roll isolation. This is the only case ever in which I have not used rubber dam isolation, and it was solely because I did not want the shards of tooth structure to embed themselves further into the gingival tissue since the severity of the tooth and root fractures could be clearly visualized. There were many tooth fragments — like shards of glass; this was unlike any trauma I had seen before (Figures 5D-5F).

Figure 3: Treatment postoperatively at first visit. Patient temporized with glass ionomer cement and cleaned up; pulpal debridements performed. Note the mixed dentition and no apparent trauma to lower mandibular anterior teeth

Figure 4: Radiograph of the maxillary anteriors after pulpal debridement with calcium hydroxide slurry as intracanal medicament

Figures 5A-5C: A. Surgical extrusion of UR1 and UL1. Extraction of UR1; only the crown portion of the tooth is held. Great precaution is taken to avoid any contact with the tooth root and its periodontal ligament cells. After this photo, the tooth was immediately placed into HBSS. B. UR1 and UL1surgically extruded and secured in their newly coronally placed positions with the functional (wire-resin) splint. C. Palatal photograph of the surgically extruded teeth with splint secured; glass ionomer access cavities shown
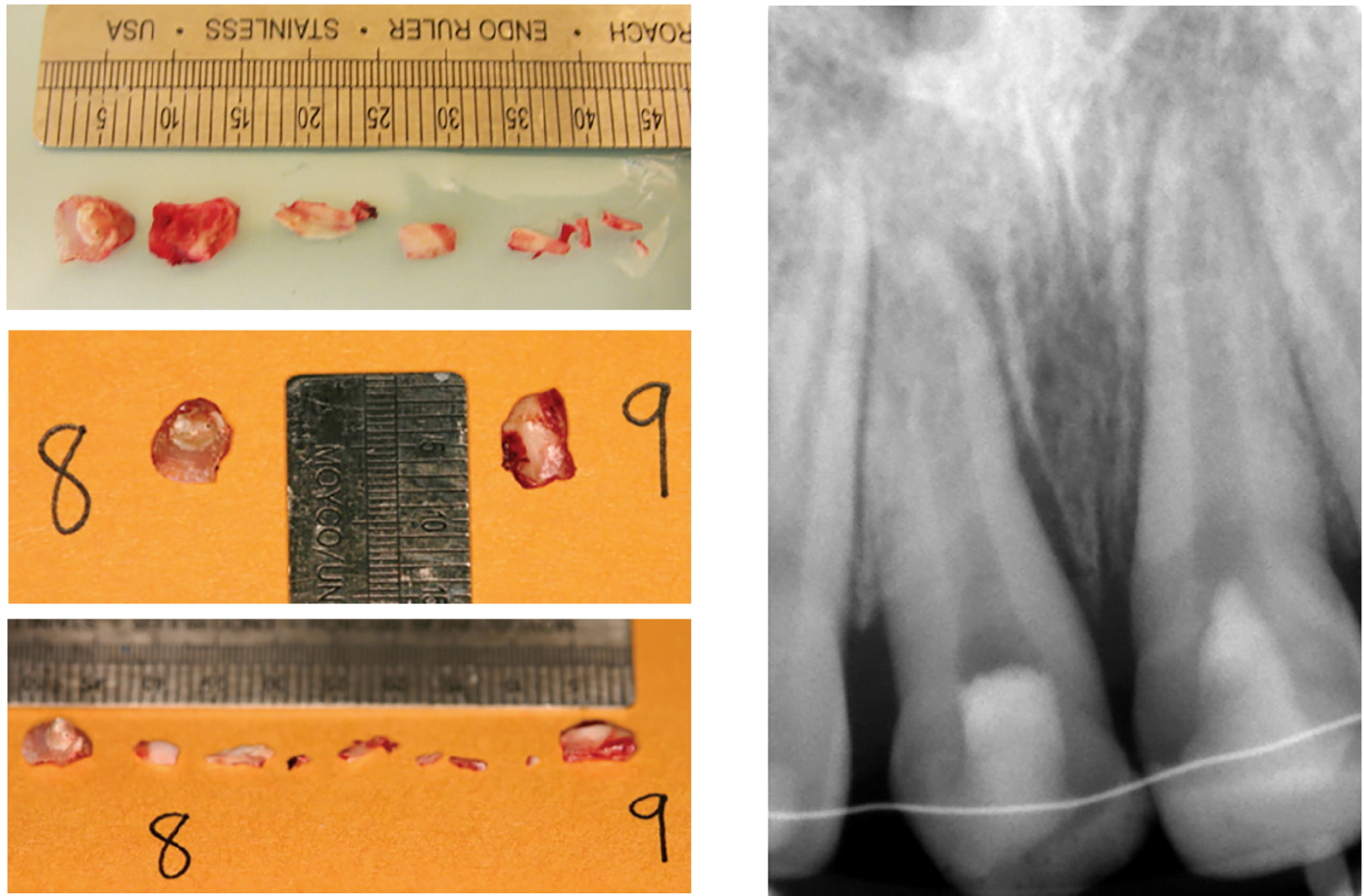
Figures 5D-5F: Images of the tooth fragments removed during the surgical procedure, measured against the ruler in millime-ters. Each tooth had one large fragment (UR1 fragment was about 6 mm long and UL1’s was about 7 mm) and several tiny fragments
Figure 5G: Angled radiographs of the teeth after surgical repositioning with the splint in place were taken; one radiograph shown here. Note the change of new space in between the teeth and the periodontal ligament due to the more coronal “new” position of both teeth
The patient was fully anesthetized, and the pulpal debridement went smoothly. An intracanal medicament made of calcium hydroxide powder mixed on a glass slab with 2% chlorhexidine gluconate was then placed with a lentulo spiral filler into both canal spaces. This is a very common technique as a treatment modality in traumatic dental injury cases; it is called for when there is a potential need for a long-term intracanal medicament, so as to aid in periodontal healing (Panzarini, et al., 2012). I temporized with Fuji IX® glass ionomer cement (GC America) and reappointed her (Figures 3 and 4).
At the next visit, we explored the extent of her injuries further after an orthodontic consultation to determine if orthodontic extrusion would be an option — as there was no remaining coronal tooth structure (DiAngelis, et al., 2012; American Association of Endodontists, 2013; Andreasen, Andreasen, Andersson, 2007; Andreasen, et al., 1995; Kinirons, et al., 2000). We decided instead upon surgical extrusion of both UR1 and UL1 after completion of root canal treatments (all after a minimum of 2 weeks of calcium hydroxide intracanal medicament) (Panzarini, et al., 2012) primarily due to the shattered state of the tooth.
Approximately 1 month after the traumatic dental injury, the patient returned with her parents for definitive treatment: Surgical extrusion of both UR1 and UL1 was planned, as it was suspected that additional sub-gingival tooth and root fragments, as well as root fractures, remained on both, despite previous pulp extirpation and pulpal medicament. Pulp vitality tests were repeated prior to any treatment or anesthesia, as the patient reported that her lower teeth had been “hurting” at this visit.
After much discussion and reviewing the risks, benefits, and options, both the parents and the patient consented to continue root canal therapy completion on both UR1 and UL1 — as well as surgical extrusion to remove any possible remaining fragments from the trauma site and to make the crowns and root fractures become, essentially, solely crown fractures (with the coronal surgical repositioning), so that both teeth could be restored. Extensive education and possible complications were discussed. The family was informed that the teeth would likely not be perfect esthetically, but that her teeth could hopefully be saved until she was old enough to seek other options: crowns, implants, veneers, etc.
Treatment that day consisted of topical followed by four carpules (1.8ml) of 2% lidocaine (1:100k epinephrine) given as buccal and palatal infiltrations; two carpules preoperatively and two carpules postoperatively for pain. A No. 15 blade was used to reflect a palatal full-thickness mucoperiosteal envelope flap (UR2 to UL2). UR1 was elevated, and the fragments were visualized and removed (Figures 5A-5F). A bigger fragment (running obliquely and more subgingival/cervical) was visualized, and it was decided to extract UR1 with forceps after elevation (Figure 5A). UR1 was immediately placed in Hank’s Balanced Salt Solution (HBSS) for 3 minutes.
Fragments remained in some granulation tissue that had grown around the gingival cuff; all visible fragments were removed, and other fractures were checked subgingivally. The tooth was reinserted back after the latter was curetted and irrigated with sterile saline. The total extraoral time for UR1 was 4 minutes; the tooth was soaking in HBSS for 3 (of the 4) minutes.
UL1 was then elevated and the visible fragments removed. Again, a bigger fragment, which ran oblique and more sub-gingival/cervical, was seen (Figures 5D-5F). As such, it was decided to also extract UL1 with forceps after elevation. It was placed immediately in HBSS for 2 minutes. Another large fragment was removed as well as others. UL1 was reinserted after the socket was curetted and irrigated with sterile saline. The total extraoral time for UL1 was 3 minutes; it was in HBSS for 2 of the 3 minutes. The optimal replantation time for the best prognosis has been declared as 5 minutes in clinical studies (Andreasen, et al., 1995; Kinirons, et al., 2000). All fragments were saved and clinical photos taken.
A cotton pellet and Fuji IX glass ionomer cement were placed to close the access. A sulcular gingivectomy was performed on UR2 to UL2 on both the buccal and palatal mucosa with a No. 12 blade; 4×4-0 Monocryl® (Ethicon) sutures were placed intrapapillary. Ultimately, UR1 was extruded approximately 4 mm-5 mm and repositioned at this point coronally; UL1 was extruded approximately 3 mm and repositioned at this point. UR2 to UL2 were prepared for a functional (nonrigid) splint with an orthodontic steel ligature with flowable resin (Figures 5B-5G) (DiAngelis, et al., 2012; American Association of Endodontists, 2013; Andreasen, et al., 2004; Andreasen, et al., 2006; Andreasen, et al., 2004; Robertson, et al., 2000; Andreasen, Andreasen, Bayer, 1989; Humphrey, Kenny, Barrett, 2003; Welbury, et al., 2002; Ebeleseder, et al., 2000).
Occlusion was checked and adjusted. Verbal and written postoperative instructions were given to the patient and parents, and the patient was informed to return if pain persisted or swelling developed. She tolerated the treatment very well, and a fair-to-guarded prognosis on both UR1 and UL1 was given at this time with the understanding that the patient was to return for root canal treatment completions and final restorations on both. Ibuprofen 400 mg was given immediately postoperatively as well as written prescriptions for doxycycline 100 mg bid, ibuprofen 400 mg qid, PRN pain x 28 tablets, and twice daily swish of 0.1% chlorhexidine (alcohol-free) oral rinse (bottle) for 1 to 2 weeks (DiAngelis, et al., 2012; American Association of Endodontists, 2013; Andreasen, Andreasen, Andersson, 2007; Andreasen et al, 2004; Andreasen, Bakland, Andreasen, 2006). An appointment was made for a 1-week checkup for a likely suture removal, with splint removal to follow in 2 to 6 weeks, as suggested by the American Academy of Pediatric Dentistry (AAPD) and American Association of Endodontists (AAE) guidelines for follow-up of traumatic dental injuries.
Follow-up
One week later, the patient returned, and periapical films of UR1 and UL1 were taken; structures appeared within normal limits. The splint was intact, and three sutures were removed (one had fallen out on its own). We discussed the need for better oral hygiene. At this stage, healing was seen, and an appointment was made for her to return in 2 weeks (Figures 6A and 6B).

Figures 6A and 6B: One week after surgical repositioning and immediately after suture removal; splint still remains
After 2 weeks, the patient returned, and clinical tests were taken (Table 2). Periodontal measurements were performed, and a few gingival defects were noted palatally on UR1 and UL1 (Table 2: “ppds”). At this early stage, the patient and parents were informed that it could still be healing (the PDL attachment reforming) — however, I did caution that the patient may need gum surgery. At this time, periapical radiographs of UR2 to UL2 were taken again to follow-up with our baseline radiographs of the adjacent teeth in case any radiographic changes, such as root resorption (Andreasen, Bakland, Andreasen, 2006; Andreasen, et al., 2004; Robertson, et al., 2000; Andreasen, Andreasen, Bayer, 1989), were to begin — it would be advantageous to see this and treat as soon as possible.

Wnl = within normal limits
That day, the distal root of UR1 appeared to be suspect: It was nonsolid like the other root surfaces. The intracanal medicament was replaced with a fresh slurry of calcium hydroxide and chlorhexidine and condensed incrementally as it was spun into the canal (Figure 7). Inverted coarse paper points were used to “dry” out the medicament some, and then condense some more. This “dry pack” method of calcium hydroxide is a very common technique when any type of root resorption is suspected (Panzarini, et al., 2012).

Figure 7: “Dry-pack” radiograph of UR1 and UL1 — canal space is completely occluded and of the same radiopacity of the tooth root. In a slurry of intracanal medicament, the canal space will appear radiolucent (as in the prior radiographs). However, in a “dry-pack,” the density makes the canal space less radiolucent and more radiopaque.
Periodic radiographic chronicling of the dentition in question is the treatment standard and encouraged with traumatic dental injuries. The American Academy of Pediatric Dentistry and American Association of Endodontists have published extensive guidelines regarding traumatic dental injuries and detailed their follow-up care at 4 weeks, 6 to 8 weeks, 4 months, 6 months and then annually for 5 years (DiAngelis, et al., 2012; American Association of Endodontists, 2013). Furthermore, it is always prudent to rule out any concomitant trauma to the opposing arch/teeth by taking a baseline radiograph of the opposing teeth at the first or second appointment. In this case, the radiograph of the lower anterior incisors was taken at the first visit for this very reason; this baseline radiograph could then be subsequently referred to if resorption or pulpal calcification were to commence and compared to at a later date.
While the patient did not attend for some of her appointments, she ultimately returned approximately 3 months later to complete the root canal treatments (Figures 8A and 8B). She reported no pain, discomfort, or symptoms. After topical anesthesia and 2.7ml of 2% lidocaine (1:100k epinephrine) given as buccal and palatal infiltrations, treatment under rubber dam isolation with premolar clamps on the buccal and palatal maxillary bone (not on the teeth), and betadine cleanse on the rubber dam access sites commenced. The GIC temporary access restorations were removed on both teeth, and the remaining calcium hydroxide medicament was irrigated out with sodium hypochlorite. Both canals were instrumented with nickel-titanium hand files and RC-Prep® (Premier Dental Products Company) (flushing with periodic sodium hypochlorite) to ISO 80.04. Working lengths were confirmed with PA films.

Figures 8A and 8B: Radiographs taken on the last treatment to build up UR1 and UL1 esthetically with composites. Both teeth were stable at this visit. Root canal treatments on UR1 and UL1 were completed about 2 months prior to this visit
After final copious sodium hypochlorite irrigation and an EDTA final rinse, the canals were dried with coarse paper points, and 80.04 master apical cones were placed with sealer. A periapical “trial obturation” film was taken, and the obturation process was completed. The pulp chamber was cleaned very well with ethanol pellets. The access cavities were prepared and flowable white composite placed, followed by incremental Z250 A1 and cured. Occlusion was checked in static and excursive function and adjusted appropriately, and then the composites were polished (Olsburgh, Jacoby, Krejci, 2001).
Again, verbal and written postoperative instructions were given, and the patient tolerated treatment well. Once again, a fair-to-guarded prognosis was given (DiAngelis, et al., 2012; American Association of Endodontists, 2013; Andreasen, Andreasen, Andersson, 2007; Kahler, Heithersay, 2008; Andreasen et al, 2004; Olsburgh, Jacoby, Krejci, 2001; Andreasen, Bakland, Andreasen, 2006; Andreasen, et al., 2004; Robertson, et al., 2000; Andreasen, Andreasen, Bayer, 1989; Humphrey, Kenny, Barrett, 2003; Welbury, et al., 2002; Ebeleseder, et al., 2000; Hinckfuss, Messer, 2009; Oikarinen, 1990; Berthold, Thaler, Petschelt, 2009; Cvek, Andreasen, Borum, 2001; Cvek, Tsilingaridis, Andreasen, 2008; Ferrazzini, Von Arx, 2008; Jackson, Waterhouse, Maguire, 2006). The patient returned 1 month later for splint removal (DiAngelis, et al., 2012; American Association of Endodontists, 2013; Andreasen, Andreasen, Andersson, 2007; Hinckfuss, Messer, 2009; Oikarinen, 1990; Berthold, Thaler, Petschelt, 2009), and periapical images were taken of the anterior teeth in both arches. All periodontal ligaments were visible and intact on all the images. The splint was removed with 169L bur and polished with white stone (Figures 9A and 9B).

Figures 9A and 9B: Clinical and palatal view photographs of UR1 and UL1 after composites. The patient and her parents were extremely satisfied with the result
Periodontal measurements were per-formed for the first time, and a few gingival defects were noted palatally on UR1 and UL1. At this early stage, the patient and parents were informed that it could still be healing (the PDL attachment reforming) – however, I did caution that the patient may need gum surgery.
A few months later, the patient returned and again reported no discomfort, pain, or symptoms since the last visit. UR1 and UL1 were built-up with composite slightly further to the patient’s satisfaction (Figures 9A and 9B). Periapical films of UR1, UL1 and LL2 to LR2 were taken, and the tests were repeated on UR2 to UL2. All of these teeth were within normal limits to percussion, palpation, mobility, and periodontal probing (less than 4 mm).
Another follow-up in 6 months with X-rays was recommended, as well as the need for annual assessments with X-rays for 5 years. The prognosis of both of these teeth was again reiterated, with the goal of ensuring their survival for as long as possible; hopefully until age 18, if not longer (at least until the patient had matured as an adult).
Discussion
Ultimately, despite great efforts, the patient never returned. Although the last set of radiographs seemed cautiously optimistic, a few scenarios (DiAngelis, et al., 2012; American Association of Endodontists, 2013; Andreasen, Andreasen, Andersson, 2007; Andreasen, et al., 1995; Kinirons, et al., 2000; Andreasen, et al., 2004; Andreasen, Bakland, Andreasen, 2006; Andreasen, et al., 2004; Robertson, et al., 2000; Andreasen, Andreasen, Bayer, 1989; Humphrey, Kenny, Barrett, 2003; Welbury, et al., 2002; Ebeleseder, et al., 2000; Cvek, Andreasen, Borum, 2001; Cvek, Tsilingaridis, Andreasen, 2008; Ferrazzini, Von Arx, 2008; Jackson, Waterhouse, Maguire, 2006) predictably occurred:
- The patient’s UR1 and UL1 healed without any further sequelae, and she still has them both present and functioning well.
- One or both of her maxillary incisors might have undergone some inflammatory root resorption and, therefore, might have had needed extracting at some point down the road, hopefully after her growth spurt, or a good amount of growth having lapsed.
- Replacement root resorption (also known as ankylosis) of one or both teeth.
While ankylosis is usually seen as negative sequelae, in this case, it would actually be quite beneficial. In a growing patient, extraction of either of these teeth would have resulted in a collapsed site deficient of cortical and cancellous bone. Maintaining bony width would be beneficial for later implant placement. When ankylosis occurs, bone replaces the tooth. This bone is beneficial, especially in a pediatric patient who is still relying on alveolar bone growth for jaw/tooth development.
When a permanent tooth is prematurely extracted on a child who is not yet fully grown, the teeth adjacent to the extraction site can also suffer negative periodontal sequelae due to the collapsed site. This is not optimal for esthetics if a fixed bridge were to be placed, or for an implant in the future.
As this was a traumatic dental injury on a pediatric patient, loss of these teeth would have been catastrophic and would have left psychosocial effects as well as functional, developmental, and esthetic challenges for her and her family to deal with lifelong. In this scenario, ankylosis is a welcomed and successful outcome as it can be predictably managed. Hence, our definition of success must change when traumatic dental injuries occur.
When ankylosis and growth of the jaw bone (either maxilla or mandible) occurs, the replacement resorption must be followed closely. The moment that the tooth becomes infraoccluded (below the adjacent teeth), further treatment must be done to intervene. In such a scenario, decoronation (Malmgren, 2000; Cohenca, Stabholz, 2007; Filippi, Pohl, Von Arx, 2001; Malmgren, 2013) would be indicated.
Much has been written on decoronation, and it is a fascinating and effective procedure that can be easily performed by a clinician with training; historically, endodontists, periodontists, and oral surgeons might have experience with such a treatment modality.
Once decoronation has been performed after extensive replacement resorption has occurred, the bone will eventually be ready for an implant when growth is complete and a very minimal, if any, alveolar defect might exist. Again, this is taking a negative sequelae and turning it into the best possible outcome.
In conclusion, the patient (and her parents) never returned. In these scenarios, it is very likely that all her teeth are still in position. Overall, I believe the best treatment was performed with the given pejorative circumstance, and the young patient was allowed to continue with maxillary alveolar growth and a semblance of dentition in her smile.
References
- American Association of Endodontists (2013). The Recommended Guidelines of the American Association of Endodontists for the Treatment of Traumatic Dental Injuries. [online] Available at: <https://www.nxtbook. com/nxtbooks/aae/traumaguidelines/#/0> [Accessed 30/06/16]
- Andreasen FM, Andreasen JO, Bayer T. Prognosis of root-fractured permanent incisors–prediction of healing modalities. Endod Dent Traumatol. 1989;5(1):11-22.
- Andreasen JO, Andreasen FM, Andersson L. 2007 Textbook and Color Atlas of Traumatic Injuries to the Teeth, 4th ed. Oxford, UK: Wiley-Blackwell; 2007.
- Andreasen JO, Andreasen FM, Mejàre I, Cvek M. Healing of 400 intra-alveolar root fractures. 2. Effect of treatment factors such as treatment delay, repositioning, splinting type and period and antibiotics. Dent Traumatol. 2004;20(4):203-211.
- Andreasen JO, Andreasen FM, Mejàre I, Cvek M. Healing of 400 intra-alveolar root fractures. 1. Effect of pre-injury and injury factors such as sex, age, stage of root development, fracture type, location of fracture and severity of dislocation. Dent Traumatol. 2004;20(4): 192-202.
- Andreasen JO, Bakland LK, Andreasen FM. Traumatic intrusion of permanent teeth. Part 3. A clinical study of the effect of treatment variables such as treatment delay, method of repositioning, type of splint, length of splinting and antibiotics on 140 teeth. Dent Traumatol. 2006;22(2):99-111.
- Andreasen JO, Borum MK, Jacobsen HL, Andreasen FM. Replantation of 400 avulsed permanent incisors. 4. Factors related to periodontal ligament healing. Endod Dent Traumatol. 1995;11(2):76-89.
- Berthold C, Thaler A, Petschelt A. Rigidity of commonly used dental trauma splints. Dent Traumatol. 2009;25(3):248-255.
- Cohenca N, Stabholz A. Decoronation – a conservative method to treat ankylosed teeth for preservation of alveolar ridge prior to permanent prosthetic reconstruction: literature review and case presentation. Dent Traumatol. 2007;23(2):87-94.
- Cvek M, Andreasen JO, Borum MK. Healing of 208 intra-alveolar root fractures in patients aged 7-17 years. Dent Traumatol. 2001;17(2):53-62.
- Cvek M, Tsilingaridis G, Andreasen JO. Survival of 534 incisors after intra-alveolar root fracture in patients aged 7-17 years. Dent Traumatol. 2008;24(4):379-387.
- DiAngelis AJ, Andreasen JO, Ebeleseder KA, et al.; International Association of Dental Traumatology. International Association of Dental Traumatology guidelines for the management of traumatic dental injuries: 1. Fractures and luxations of permanent teeth. Dent Traumatol. 2012;28(1):2-12.
- Ebeleseder KA, Santler G, Glockner K, Hulla H, Pertl C, Quehenberger F. An analysis of 58 traumatically intruded and surgically extruded permanent teeth. Endod Dent Traumatol. 2000;16(1):34-39.
- Ferrazzini Pozzi EC, von Arx T. Pulp and periodontal healing of laterally luxated permanent teeth: results after 4 years. Dent Traumatol. 2008;24(6):658-662.
- Filippi A, Pohl Y, von Arx T. Decoronation of an ankylosed tooth for preservation of alveolar bone prior to implant placement. Dent Traumatol. 2001;17(2):93-95.
- Hinckfuss SE, Messer LB. Splinting duration and periodontal outcomes for replanted avulsed teeth: a systematic review. Dent Traumatol. 2009;25(2):50-57.
- Humphrey JM, Kenny DJ, Barrett EJ. Clinical outcomes for permanent incisor luxations in a pediatric population. I. Intrusions. Dent Traumatol. 2003;19(5):266-273.
- Jackson NG, Waterhouse PJ, Maguire A. Factors affecting treatment outcomes following complicated crown fractures managed in primary and secondary care. Dent Traumatol. 2006;22(4):179-185.
- Kahler B, Heithersay GS. An evidence-based appraisal of splinting luxated, avulsed and root-fractured teeth. Dent Traumatol. 2008;24(1):2-10.
- Kinirons MJ, Gregg TA, Welbury RR, Cole BO. Variations in the presenting and treatment features in reimplanted permanent incisors in children and their effect on the prevalence of root resorption. Br Dent J. 2000;189(5):263-266.
- Malmgren B. Decoronation: how, why, and when? J Calif Dent Assoc. 2000;28(11): 846-854.
- Malmgren B. Ridge preservation/decoronation. Pediatr Dent. 2013;35(2):164-169.
- Oikarinen K. Tooth splinting: a review of the literature and consideration of the versatility of a wire-composite splint. Endod Dent Traumatol. 1990;6(6):237-250.
- Olsburgh S, Jacoby T, Krejci I. Crown fractures in the permanent dentition: pulpal and restorative considerations. Dent Traumatol. 2001;18(3):103-115.
- Panzarini SR, Trevisan CL, Brandini DA, et al. Intracanal dressing and root canal filling materials in tooth replantation: a literature review. Dent Traumatol. 2012;28(1):42-48.
- Robertson A, Andreasen FM, Andreasen JO, Norén JG. Long-term prognosis of crown-fractured permanent incisors. The effect of stage of root development and associated luxation injury. Int J Paediatr Dent. 2000;10(3):191-199.
- Welbury R, Kinirons MJ, Day P, Humphreys K, Gregg TA. Outcomes for root-fractured permanent incisors: a retrospective study. Pediatr Dent. 2002;24(2):98-102.
Stay Relevant With Endodontic Practice US
Join our email list for CE courses and webinars, articles and more..


