CE Expiration Date: March 18, 2027
CEU (Continuing Education Unit):2 Credit(s)
AGD Code: 010
Educational aims and objectives
This self-instructional course for dentists aims to identify how artificial intelligence (AI) works, as well as its advantages and disadvantages in the endodontic and general dental practice.
Expected outcomes
Endodontic Practice US subscribers can answer the CE questions by taking the quiz online to earn 2 hours of CE from reading this article. Correctly answering the questions will demonstrate the reader can:
- Define AI and the evolving types of AI.
- Identify the basics of how the data is used in a clinical way by interacting with AI-enabled systems and machines.
- Recognize how AI systems are being used to improve aspects of the implant process.
- Realize some of the issues that need to be addressed to ensure patient safety, clinical success, and to safeguard the practice from legal complications.
Drs. Aaron Glick, David Jaramillo, Nisha Manila, and Jennifer Chang discuss AI in the dental practice, and its impact on endodontics.
 Drs. Aaron Glick, David Jaramillo, Nisha Manila, and Jennifer Chang discuss the pros and cons of AI in endodontic and general dental practice
Drs. Aaron Glick, David Jaramillo, Nisha Manila, and Jennifer Chang discuss the pros and cons of AI in endodontic and general dental practice
Introduction
Although artificial intelligence (AI) has been integrated in daily life, most are not aware that it has become an integral part of many aspects of modern life over the past decades given the increased computing power, digitization of data, advances in algorithm, and improvements in accuracy. In fact, when a group of Americans were surveyed, over half were not able to identify that AI was powering wearable fitness trackers, automated chatbots, product recommendations, security cameras that identify unrecognized people, music playlist recommendations, and email services identifying spam messages.1 In dentistry, some of these same AI systems, such as chatbots, have been integrated for general office support and software automations. Other AI systems that are more dental-specific have also been used for approximately a decade. These include systems that automatically identify dental landmarks in CBCT,2 maxillary/mandibular segmentation from radiographic images,3 and digital reconstruction of tooth surfaces.4
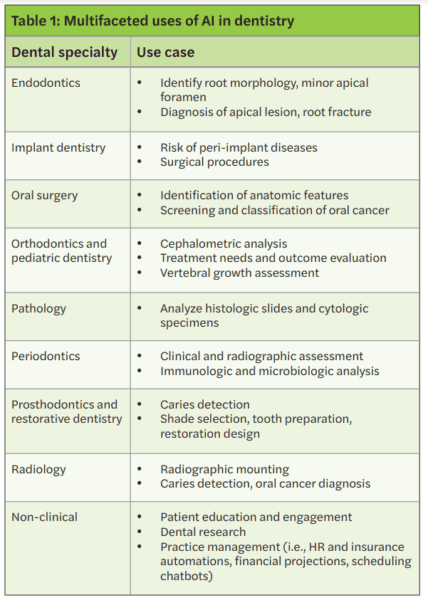
Some examples of more current AI systems in dentistry are decision-support systems to aid clinicians in the diagnosis of caries and periodontal conditions, AI-enabled robotic surgeries, and creation of AI-generated dental restorations/appliances.5 Since AI is a tool, it can be used in multiple applications within the dental field; as the algorithms advance in accessibility and accuracy, the amount of products with embedded AI will likely increase (Table 1). Therefore, it is important as a dental practitioner to understand the tools used, particularly if they can have a direct or indirect effect on patients.
How AI works
AI is a broad term that generally refers to the ability for computers to perform tasks that typically require human intelligence (Figure 1); for example, viewing a dental X-ray and identifying interproximal caries. Machine learning (ML) refers to the mathematical approach to accomplish this perceived human intelligence. These algorithms are programmed to take information and “learn” from these datasets. Since there are alternative methods for artificial intelligence, machine learning is considered a subset of the approaches to achieve artificial intelligence. Multiple types of algorithms can be programmed by the user. In one approach, a convolutional neural network (CNN) can feed a large dataset to identify the features that are most salient in a classification task. For instance, with multiple pictures of apples or cats, the neural network would be a mathematical model used to make the binary decision on if the currently presented image should be classified as an apple or cat. The CNN approach is typically selected for image operations since this algorithm is optimized to process images based on the extraction of
spatial features.
Depending on the task to be performed, there are multiple types of models that are specific to optimizing for the type of data or output intended. For instance, chatbots require a text-based approach with grammatical rules built into sequences of words. Therefore, language-specific models would be used for text-based tasks, typically called natural language processing (NLP).
Further into the black box
While most dentists today don’t consider building custom AI products, there are products that will democratize the use of AI through no-coding technologies.6 Whether coding the algorithms or not, understanding the basics of how the data is used to derive a clinical decision/outcome is important since dentists are increasingly interacting with AI-enabled systems and machines.

When software manufacturers train an AI model, they require a large amount of data to process. In general, the full dataset is split into 3 distinct groups: 1) training set, 2) validation set, and 3) testing set (Figure 1). In a supervised model, a team of clinicians will label the full dataset. For instance, if the classification task is to automatically identify caries in bitewing radiographs, the clinician would identify areas of the radiographs with caries. These labeled radiographs serve as the “ground truth” for the algorithm. The bulk of the data is used in the training set to optimize the weights of the neural network identifying salient features of the categorized dataset. The model is then further optimized by using a validation dataset, where additional processes can improve the accuracy. The final step is to understand how accurate the fully trained AI model can perform on the similar dataset. Therefore, the testing dataset is then categorized by the trained model to provide an accuracy typically reported as a percentage of accurately categorized responses and Receiver Operating Characteristics (ROC) curve/area under the curve (AUC). The ROC curve and AUC offers additional details similar to the true positive rate and false positive rate. Ultimately, the large dataset is trained, and the same isolated dataset is used to assess the accuracy in a non-clinical setting.
When building these algorithms, there are some additional key considerations as to how the algorithm uses data. In an oversimplification, an algorithm can be delineated as 1) supervised/unsupervised or 2) static/continuous learning. Supervised learning is based on a clinician providing the algorithm with a ground truth for labelled data, similar to the previous example. Unsupervised learning is where the model learns without explicitly provided information to classify and can be accomplished through patterns within the data. Static learning algorithms are the traditional type of AI; however, some current algorithms are designed to update and improve themselves based on additional data acquired during use.

AI in endodontics
AI is changing our daily lives and approaches to dentistry in general. In endodontics, AI is being used for the following:
- Radiographic detection of periapical lesions and root fractures
- Treatment assistance for determining working length and root morphology
- Treatment outcome predictions for retreatment and stem cell therapies
Innovations in radiographic identification of endodontic specific features focus mainly on periapical and root fractures.5 Multiple types of radiographs have been used as inputs for machine learning systems, such as periapical, panoramic, and cone-beam computed tomographic (CBCT). Accuracies of periapical lesion identification have been shown to have classification accuracies up to 97%, 84%, and 96% using periapical, panoramic, and CBCT radiographs respectively with generally higher average accuracy with CBCT in published literature.7,8 Similarly, vertical root fracture detection has higher diagnostic accuracy when using machine learning in CBCT versus periapical radiographs.9
AI has been applied in multiple facets for the treatment of endodontic practice such as determining working lengths, assistive tools to navigate root morphology, optimal selection of force/torque during canal preparation, implementing image-guided robotic surgery, and other integrations of AI within hardware used for treatment purposes.10 Another interesting future application to endodontics that has been used in other areas of healthcare is drug delivery and biofilm disruption using nanorobots controlled by machine learning.11
Leveraging one of the key values of AI is complex pattern recognition beyond the human ability. Applying machine learning to large-scale datasets of clinical endodontics information can facilitate predictions of treatment success. For instance, complex patient and clinical interactions hold patterns that can elucidate patient-specific chances for treatment success or failure. AI-powered tools have the potential to discriminate optimal first-line treatment approaches despite these complex interactions. Currently, machine learning techniques have been applied to the prognosis of endodontic microsurgeries, decision to retreat the root canal system, and regeneration technique of dental pulp.12,13 Additionally, clinical decisions such as selecting the patient-specific appropriate course of antibiotics or pain medications could potentially be identified using AI tools. Currently, AI algorithms have been developed to identify the occurrence and severity of postoperative pain based on patient-specific factors.14
A light in the black box
AI presents an exciting tool to simulate human intelligence to help dentists achieve a higher quality of life, better decision-making capability, and fewer postoperative complications.15 However, despite these advances, AI in dentistry is in its infancy. On the horizon are more autonomous systems that do not require human input at the clinical stage within the AI algorithm. While a good understanding of the basics of AI is useful, the actual processes of most algorithms and datasets are not transparent to clinicians. Accuracy, trust, data stewardship, and equity/sustainability are concerns that clinicians and AI software manufacturers need to address to ensure patient safety, clinical success, and safeguarding from legal complications.
Accuracy
The accuracy of an AI system is based on a predefined gold standard. Most clinical decision support tools are supervised algorithms and labeled by clinical dentists without histologic confirmation. Since the amount of data that is required to train the models is so large, it is impractical to build highly accurate datasets that are verified with high-quality standards. In fact, the sensitivity for dentists to detect interproximal caries in bitewings in dentin is low (.36),16 and provider agreement also is low (.4 kappa).17 Similar findings have been seen in other fields such as in periodontal conditions yet are task specific.18 While the quality of the dataset will likely not be transparent, the process for labeling the data as an important factor in the accuracy of the system could be stated by the manufacturer. Another issue that can affect AI is the imbalance of certain conditions like rare pathology that limit the number of instances for the algorithm to learn.
What is the clinical accuracy of these AI models? Is the trained dataset similar to your patient population or data in your EHR? Most report accuracies on the original dataset that was used, yet the true accuracies with different datasets or after clinicians have interacted with the AI system remain limited, and independent testing remains even more limited. In fact, some studies have shown that when AI presents incorrect information, clinicians are more likely to be misled by this recommendation which could result in poor patient outcomes.19,20 Should incorrect guidance be provided by the AI system and patient harm occurs, the current legal climate would hold the clinician liable.21 Additionally, when the AI system is accurate, there are concerns of other biases and trust.
Currently, machine learning techniques have been applied to the prognosis of endodontic microsurgeries, decision to retreat the root canal system, and regeneration technique of dental pulp.
Trust
A human-computer interaction exists between the dentist and AI system that can affect the perception of clinical information and ultimately treatment performance and decision. Trust is a well-studied concept that is affected by many factors with transparency, reliability, and tangibility as some of the commonly cited values that apply most to human-computer interaction.22
Transparency is inherent in trust, and AI systems can be built to be explainable. While most traditional forms of AI suffer from the “black box problem,” some offer detection strategies through computer vision,23 and others provide embeddings through natural language processing.24 Reliability offers a perception that the algorithm is making similar decisions in seemingly similar circumstances. For continuously learning algorithms, there is a potential risk that adaptive learning could introduce new errors and reduce reliable performance.25,26 Tangibility refers to the physical or virtual presence of the AI system and when it appears more real or anthropomorphic, which improves trust.27
Data stewardship
Machine learning sits at the intersection of big data and software algorithms. Given the need for large datasets to train models, the data stewardship in regulated industries, especially dentistry, is important. Dental offices handle private data on patients within their electronic health record system such as financial, demographic, disease state information, and other sensitive clinical information. With the digitization of records and equipment, the dental industry is a prime target for hackers and also lacks adequate knowledge about the prevention of these crimes.28 In fact, Henry Schein, a large distribution, and software company with more than 23,000 employees and 1-million customers globally, halted operations due to a cyber-security incident.29 Large, consolidated datasets with patient data are vulnerable to attacks. Additionally, generative AI that ingests data from multiple sources feeding back into the algorithm can pose a risk if patient data is used. For instance, divulging patient data on a generative AI platform to write patient notes more efficiently could put the dentist at risk of breaching HIPAA with patient data being used to continuously train the model. For example, Sarah Silverman is suing openAI and Meta over violations of her copyrighted book that surfaced when these platforms regurgitated substantial elements of her copyrighted materials.30
Equitability/sustainability
The equitable treatment of patients is an ethical value upheld by the American Dental Association where all treatment decisions should be determined on the same basis as all other patients. As AI systems are built with human inputs, biases can be encoded into the model.32 In one example of this Optum, a health service company, created an AI program to spot high-risk patients that should receive medical follow-up care. However, the follow-up care disproportionately identified white patients with 82% white and 18% black patients identified compared to an independent analysis finding that 53% white and 46% black patients should have been identified based on medical need. Before this error could be detected, the program had already been applied to 100 million patients.33 Additionally, the hardware that powers AI requires high energy and a large local ecological footprint.34 In fact, GPT3 took 1.287 gigawatt hours of electricity and 700,000 liters of clean freshwater.35
Implementation of AI systems
As manufacturers continue to release new and update current AI embedded technologies, dentists should be aware of how these tools operate and can potentially change patient care. Many dentists are likely to already implement embedded AI technologies without fully realizing it since AI is commonly used as a tool to accomplish a task or optimize tasks, and most backend systems are not transparent to the user.
In order to implement new technologies with AI into a dental office, technology acceptance and continual quality assurance should be a consideration. The primary factors for technology acceptance are perceived usefulness and perceived ease of use.36 Therefore, removing barriers to trust within the human-computer interaction can improve usage. Training with technology in a safe environment can build confidence and improve ease of use. Additionally, having a plan for continuous quality assurance with the use of AI can aid in patient safety given that the systems can change with updates or continuously learning models. AI behavior should be periodically monitored, and a set of well-defined metrics are needed to guide regularly scheduled testing.37
The US government also functions to protect patients and dental offices’ implementation of AI through the FDA clearance process of software as a medical device. FDA has become increasingly more stringent on this type of software that predicts and identifies medical/dental conditions.38 As dentists expand their appetite for additional functionality of these software systems, there needs to be a balance between the regulatory burden and the ability to innovate.
Exciting future of AI in dentistry
With the digitization of dental records and radiographs, dentistry is an ideal profession to harness AI. Current applications of AI are already being implemented to change the workflow of dental offices and patient care. Despite risks of inaccuracies, human-computer mistrust, data security concerns, and inequities in applications, it is easy to imagine overcoming these obstacles as the perceived future benefits outweigh the risks.39 Healthcare in general is expected to see an increase in venture investments as the value of AI in health is expected to grow from $4.9B in 2020 to $45.2B in 2026. Dentistry, however, is lacking in the amount and accuracy of data.40 To accelerate the advancement of AI, manufacturers need access to large, structured datasets that contain valid and reliable data. In fact, each of our practices holds valuable data that has the potential to improve the field.
The use of AI in the dental practice is growing. Read this introduction by Dr. Chafic Safi on how to embrace changes and keep up with new technologies here: https://endopracticeus.com/keeping-up/
References
- Kennedy B, Tyson A, Saks E. Public awareness of artificial intelligence in everyday activities. Pew Research Center. (Published February 15, 2023.) https://www.pewresearch.org/science/2023/02/15/public-awareness-of-artificial-intelligence-in-everyday-activities/. (Accessed: November 24, 2023.)
- Cheng E, Chen J, Yang J, Deng H, Wu Y, Megalooikonomou V, Gable B, Ling H. Automatic Dent-landmark detection in 3-D CBCT dental volumes. Annu Int Conf IEEE Eng Med Biol Soc. 2011;2011:6204-6207.
- El-Bialy A. Towards a Complete Computer Dental Treatment System. 2008 Cairo International Biomedical Engineering Conference, Cairo, Egypt. 2008:1-8.
- Sporring J., Hommelhoff Jensen K. Bayes Reconstruction of Missing Teeth. J Math Imaging Vis. 2008;31:245–254.
- Chang J, Glick A. Clinical implementation of artificial intelligence systems. J Greater Houston Dent Soc. 2023; 94(2):18-19.
- Sundberg L, Holmström J. Democratizing artificial intelligence: How no-code AI can leverage machine learning operations. Business Horizons. 2023;66(6):777-778.
- Leonardi Dutra K, Haas L, Porporatti AL, Flores-Mir C, Nascimento Santos J, Mezzomo LA, Corrêa M, De Luca Canto G. Diagnostic Accuracy of Cone-beam Computed Tomography and Conventional Radiography on Apical Periodontitis: A Systematic Review and Meta-analysis. J Endod. 2016 Mar;42(3):356-364.
- Sadr S, Mohammad-Rahimi H, Motamedian SR, Zahedrozegar S, Motie P, Vinayahalingam S, Dianat O, Nosrat A. Deep Learning for Detection of Periapical Radiolucent Lesions: A Systematic Review and Meta-analysis of Diagnostic Test Accuracy. J Endod. 2023 Mar;49(3):248-261.e3.
- Salineiro FCS, Kobayashi-Velasco S, Braga MM, Cavalcanti MGP. Radiographic diagnosis of root fractures: a systematic review, meta-analyses and sources of heterogeneity. Dentomaxillofac Radiol. 2017 Dec;46(8):20170400.
- Khanagar SB, Alfadley A, Alfouzan K, Awawdeh M, Alaqla A, Jamleh A. Developments and Performance of Artificial Intelligence Models Designed for Application in Endodontics: A Systematic Review. Diagnostics (Basel). 2023 Jan 23;13(3):414.
- Singh AV, Chandrasekar V, Janapareddy P, Mathews DE, Laux P, Luch A, Yang Y, Garcia-Canibano B, Balakrishnan S, Abinahed J, Al Ansari A, Dakua SP. Emerging Application of Nanorobotics and Artificial Intelligence To Cross the BBB: Advances in Design, Controlled Maneuvering, and Targeting of the Barriers. ACS Chem Neurosci. 2021 Jun 2;12(11):1835-1853.
- Qu Y, Lin Z, Yang Z, Lin H, Huang X, Gu L. Machine learning models for prognosis prediction in endodontic microsurgery. J Dent. 2022 Mar;118:103947.
- Aminoshariae A, Kulild J, Nagendrababu V. Artificial Intelligence in Endodontics: Current Applications and Future Directions. J Endod. 2021 Sep;47(9):1352-1357.
- Gao X, Xin X, Li Z, Zhang W. Predicting postoperative pain following root canal treatment by using artificial neural network evaluation. Sci Rep. 2021 Aug 26;11(1):17243.
- Nguyen TT, Larrivée N, Lee A, Bilaniuk O, Durand R. Use of Artificial Intelligence in Dentistry: Current Clinical Trends and Research Advances. J Can Dent Assoc. 2021 May;87:l7.
- Schwendicke F, Tzschoppe M, Paris S. Radiographic caries detection: A systematic review and meta-analysis. J Dent. 2015 Aug;43(8):924-933. Epub 2015 Feb 24. Erratum in: J Dent. 2021 Nov;114:103783.
- Naitoh M, Yuasa H, Toyama M, Shiojima M, Nakamura M, Ushida M, Iida H, Hayashi M, Ariji E. Observer agreement in the detection of proximal caries with direct digital intraoral radiography. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 1998 Jan;85(1):107-112.
- Meusburger T, Wülk A, Kessler A, Heck K, Hickel R, Dujic H, Kühnisch J. The Detection of Dental Pathologies on Periapical Radiographs-Results from a Reliability Study. J Clin Med. 2023 Mar 13;12(6):2224.
- Glick A, Clayton M, Angelov N, Chang J. Impact of explainable artificial intelligence assistance on clinical decision-making of novice dental clinicians. JAMIA Open. 2022 May 17;5(2):ooac031.
- Gaube S, Suresh H, Raue M, Merritt A, Berkowitz SJ, Lermer E, Coughlin JF, Guttag JV, Colak E, Ghassemi M. Do as AI say: susceptibility in deployment of clinical decision-aids. NPJ Digit Med. 2021 Feb 19;4(1):31.
- Maliha G, Gerke S, Cohen IG, Parikh RB. Artificial Intelligence and Liability in Medicine: Balancing Safety and Innovation. Milbank Q. 2021 Sep;99(3):629-647.
- Glikson E, Williams Woolley A. Human trust in artificial intelligence: Review of empirical research. Academy of Management Annals. 2020;14.2: 627-660.
- Meske C, Bunde E. “Transparency and trust in human-AI-interaction: The role of model-agnostic explanations in computer vision-based decision support.” Artificial Intelligence in HCI. First International Conference, AI-HCI 2020, Held as Part of the 22nd HCI International Conference, HCII 2020, Copenhagen, Denmark, July 19–24, 2020, Proceedings 22. Springer International Publishing, 2020.
- Zini, JR, Awad M. On the explainability of natural language processing deep models. ACM Computing Surveys. 2022;55.5:1-31.
- Vokinger KN, Feuerriegel S, Kesselheim AS. Continual learning in medical devices: FDA’s action plan and beyond. Lancet Digit Health. 2021 Jun;3(6):e337-e338.
- Pianykh OS, Langs G, Dewey M, Enzmann DR, Herold CJ, Schoenberg SO, Brink JA. Continuous Learning AI in Radiology: Implementation Principles and Early Applications. 2020 Oct;297(1):6-14.
- Kim K, Bölling L, Haesler S, Bailenson, Bruder G, Welch G. Does a digital assistant need a body? The influence of visual embodiment and social behavior on the perception of intelligent virtual agents in AR. 2018 IEEE International Symposium on Mixed and Augmented Reality (ISMAR).
- Melon E, Hernandez W. Cybersecurity in the dental healthcare sector: The need of knowledge for small practitioners. Issues in Information Systems. 2020;21(1):118-124.
- Henry Schein. “Henry Schein provides information on cybersecurity incident.” [Press release]. Available at: https://investor.henryschein.com/news-releases/news-release-details/henry-schein-provides-information-cybersecurity-incident. (Accessed November 25, 2023).
- Hayes, Carol Mullins, Generative Artificial Intelligence and Copyright: Both Sides of the Black Box (July 21, 2023). Available at SSRN: https://ssrn.com/abstract=4517799 or http://dx.doi.org/10.2139/ssrn.4517799. Accessed January 4, 2024.
- American Dental Association. Principles of Ethics & Code of Professional Conduct. https://www.ada.org/-/media/project/ada-organization/ada/ada-org/files/about/ada_code_of_ethics.pdf?rev=ba22edfdf1a646be9249fe2d870d7d31&hash=CCD76FCDC56D6F2CCBC46F1751F51B96. Accessed November 25, 2023.
- Schönberger, Daniel. Artificial intelligence in healthcare: a critical analysis of the legal and ethical implications. International Journal of Law and Information Technology. 2019;27(2):171-203.
- Obermeyer Z, Powers B, Vogeli C, Mullainathan S. Dissecting racial bias in an algorithm used to manage the health of populations. 2019 Oct 25;366(6464):447-453.
- Kopka A, Grashof N. Artificial intelligence: Catalyst or barrier on the path to sustainability? Technological Forecasting and Social Change. 2022;175:121318.
- Baxter K, Schlesinger Y. Managing the risks of generative AI. Harvard Business Review. https://hbr.org/2023/06/managing-the-risks-of-generative-ai. (Accessed November 11, 2023).
- Alhashmi SFS, Alshurideh M, Al Kurdi B, Salloum S. “A systematic review of the factors affecting the artificial intelligence implementation in the health care sector.” Proceedings of the International Conference on Artificial Intelligence and Computer Vision (AICV2020). Springer International Publishing, 2020.
- Mahadevaiah G, Rv P, Bermejo I, Jaffray D, Dekker A, Wee L. Artificial intelligence-based clinical decision support in modern medical physics: Selection, acceptance, commissioning, and quality assurance. Med Phys. 2020 Jun;47(5):e228-e235.
- Harvey HB, Gowda V. How the FDA Regulates AI. Acad Radiol. 2020 Jan;27(1):58-61.
- Tandon D, Rajawat J. Present and future of artificial intelligence in dentistry. J Oral Biol Craniofac Res. 2020 Oct-Dec;10(4):391-396.
- Hassani H, Andi PA, Ghodsi A, Norouzi K, Komendantova N, Unger S. Shaping the future of smart dentistry: From Artificial Intelligence (AI) to Intelligence Augmentation (IA). 2021;2(3):510-523.
Stay Relevant With Endodontic Practice US
Join our email list for CE courses and webinars, articles and more..

 Drs. Aaron Glick, David Jaramillo, Nisha Manila, and Jennifer Chang discuss the pros and cons of AI in endodontic and general dental practice
Drs. Aaron Glick, David Jaramillo, Nisha Manila, and Jennifer Chang discuss the pros and cons of AI in endodontic and general dental practice Aaron Glick, DDS, works in healthcare innovation and is on faculty at the University of Texas Health Science Center at Houston School of Dentistry and Sam Houston State University College of Osteopathic Medicine. He is a Diplomate of the ABDSM, faculty member of the AADSM Mastery Program, and holds fellowship credentials with Academy of General Dentistry and International Congress of Oral Implantology. He enjoys all technologies and has a background in software programming for neuroscience research at Brandeis University and Harvard University using 3D modeling, AI, and fMRI technologies. Dr. Glick has been published in medical and dental journals and lectures nationally on dental sleep medicine and digital/software technologies.
Aaron Glick, DDS, works in healthcare innovation and is on faculty at the University of Texas Health Science Center at Houston School of Dentistry and Sam Houston State University College of Osteopathic Medicine. He is a Diplomate of the ABDSM, faculty member of the AADSM Mastery Program, and holds fellowship credentials with Academy of General Dentistry and International Congress of Oral Implantology. He enjoys all technologies and has a background in software programming for neuroscience research at Brandeis University and Harvard University using 3D modeling, AI, and fMRI technologies. Dr. Glick has been published in medical and dental journals and lectures nationally on dental sleep medicine and digital/software technologies. David Jaramillo, DDS, is a tenured professor at the Department of Endodontics at UTHealth School of Dentistry. He has taught non-stop since 1990 at the University of Southern California and Loma Linda University in California as a clinic director of endodontics and course director of endodontics in the International Dentist Program. Dr. Jaramillo’s main research focus is in the irrigation of the root canal system. He has dictated more than 100 conferences worldwide, published over 22 peer-reviewed papers, written seven book chapters, and is a member of the International College of Dentists, AAE, and IFEA.
David Jaramillo, DDS, is a tenured professor at the Department of Endodontics at UTHealth School of Dentistry. He has taught non-stop since 1990 at the University of Southern California and Loma Linda University in California as a clinic director of endodontics and course director of endodontics in the International Dentist Program. Dr. Jaramillo’s main research focus is in the irrigation of the root canal system. He has dictated more than 100 conferences worldwide, published over 22 peer-reviewed papers, written seven book chapters, and is a member of the International College of Dentists, AAE, and IFEA. Nisha Manila BDS, PhD, is an Associate Professor and Director of Oral and Maxillofacial Radiology at California Northstate University College of Dental Medicine. With a dental degree from India, and a Ph.D. in Oral Radiation Oncology from Tokyo Medical and Dental University, Japan, she completed Oral and Maxillofacial Radiology training at Texas A&M University. Dr. Manila is a fellow of the American College of Dentists, and her research interests include applications of AI in dentistry, CBCT imaging, and advanced diagnostic imaging modalities. Dr. Manila is an active member of several professional organizations.
Nisha Manila BDS, PhD, is an Associate Professor and Director of Oral and Maxillofacial Radiology at California Northstate University College of Dental Medicine. With a dental degree from India, and a Ph.D. in Oral Radiation Oncology from Tokyo Medical and Dental University, Japan, she completed Oral and Maxillofacial Radiology training at Texas A&M University. Dr. Manila is a fellow of the American College of Dentists, and her research interests include applications of AI in dentistry, CBCT imaging, and advanced diagnostic imaging modalities. Dr. Manila is an active member of several professional organizations. Jennifer Chang DDS, MSD, is an assistant professor and program director in the Department of Periodontics at The University of Texas School of Dentistry at Houston. She completed her Doctor of Dental Surgery degree and 2 years of general practice residency in Taiwan. She obtained her Master of Science in Dentistry degree in periodontics from Indiana University School of Dentistry. Dr. Chang is a board-certified Diplomate in Periodontology and Dental Implant Surgery. She maintains a part-time practice at the school’s faculty group practice and in the greater Houston area. Her clinical and research interests focus on improving treatment options for periodontal/peri-implant disease.
Jennifer Chang DDS, MSD, is an assistant professor and program director in the Department of Periodontics at The University of Texas School of Dentistry at Houston. She completed her Doctor of Dental Surgery degree and 2 years of general practice residency in Taiwan. She obtained her Master of Science in Dentistry degree in periodontics from Indiana University School of Dentistry. Dr. Chang is a board-certified Diplomate in Periodontology and Dental Implant Surgery. She maintains a part-time practice at the school’s faculty group practice and in the greater Houston area. Her clinical and research interests focus on improving treatment options for periodontal/peri-implant disease.
