CE Expiration Date:
CEU (Continuing Education Unit): Credit(s)
AGD Code:
Educational aims and objectives
This clinical article aims to demonstrate the use of a new bioceramic material (TotalFill® Putty is also known as EndoSequence® BC RRM Putty™ in the US and CAN – Brasseler USA) to aid endodontic treatment.
Expected outcomes
Endodontic Practice US subscribers can answer the CE questions to earn 2 hours of CE from reading this article. Correctly answering the questions will demonstrate the reader can:
- Recognize how to use this bioceramic material in a case with open apices.
- See how this material works with resorption defects.
- Realize how this material can be used in retrograde endodontic cases.
- Identify the composition of TotalFill putty and requirements for use.
- Recognize the advantages and disadvantages of using this bioceramic material.
Drs. Kazim Mahmood, Obyda Essam, Mike Dodd, and Fadi Jarad present case studies that demonstrate the use of a new bioceramic material
Recent advances in endodontics have seen an increase in the use of bio-ceramic materials. Since its advent, there have been a series of sealers, pastes, and putties produced as an alternative to zinc oxide eugenol, calcium hydroxide, and resin-based systems.
Aims
The aim of this case series is to demonstrate the use of a new bioceramic material (TotalFill® Putty is also known as EndoSequence® BC RRM Putty™ in the US and CAN – Brasseler USA) to aid endodontic treatment. This will involve a review of nine cases treated using this material, including a mixture of open apices, resorption defects, and retrograde endodontic cases that were completed by a DCT and two endodontic postgraduate students from the restorative department at Liverpool Dental Hospital.
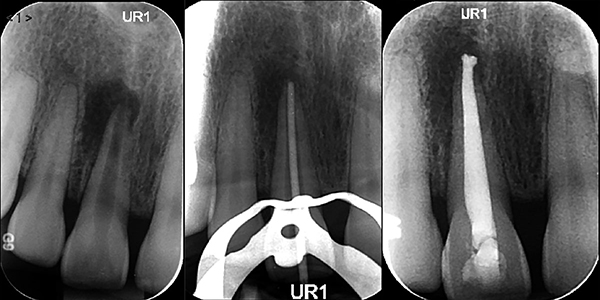
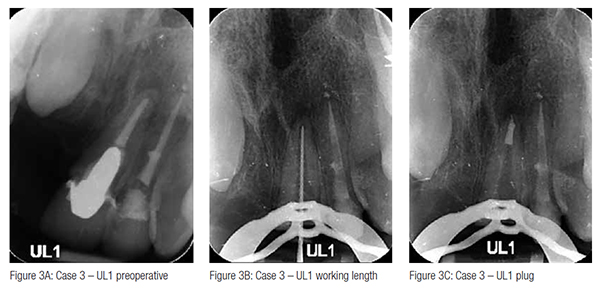
Case 1: open apex apical plug obturation UR1
A 32-year-old female patient presented with chronic periapical periodontitis affecting her non-vital immature UR1. Preoperative radiographs confirmed the presence of an open apex and a periapical radiolucency (Figure 1A). A TotalFill plug of 4 mm was provided followed by GP backfill and a definitive composite restoration (Figures 1B and 1C). There was 1 mm extrusion of the apical plug (Figure 1D).
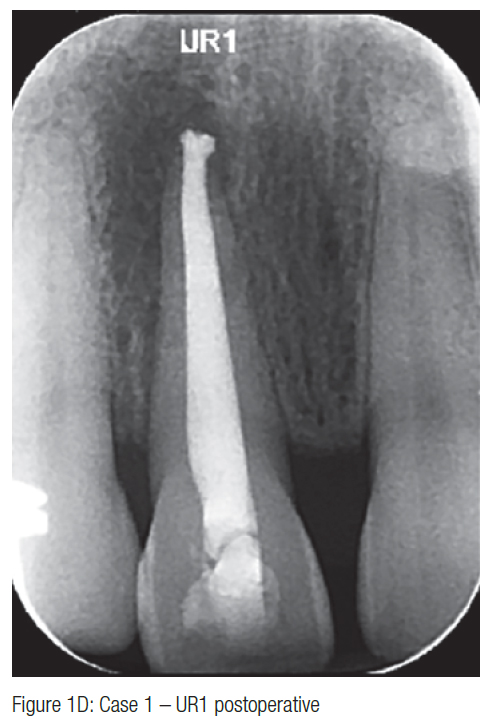
Case 2: internal root resorption defect UR2
A 16-year-old female patient attended with chronic periapical periodontitis affecting her UR2 with evidence of internal root resorption affecting the apical third of the root canal (Figure 2A). The initial treatment strategy involved obturating the canal conventionally with gutta percha (Figure 2B). This was deemed unsuccessful at follow-up, and a decision was made to provide a TotalFill putty apical plug to obturate the resorptive defect with a backfill of gutta percha (Figure 2C). A good quality obturation with minimal extrusion was achieved (Figure 2D).
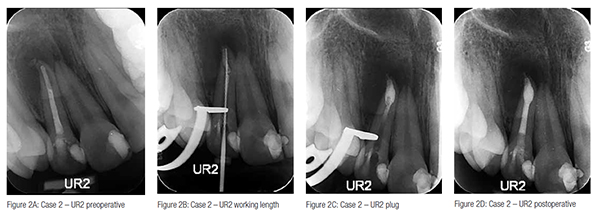
Case 3: failed RCT and post crown UL1
A male patient attended with chronic periapical periodontitis, affecting his root canal treated and post crowned UL1 (Figure 3A). A decision was made to attempt to remove the post/crown and provide a re-root canal treatment. The master apical file exceeded 60K, and a TotalFill putty plug followed by a backfill GP obturation was provided (Figures 3B and 3C). The plug was well condensed with no extrusion.
Case 4: apicectomy LR1 and LL1
A 35-year-old male attended with chronic periapical periodontitis, affecting his LR1 and LL1 associated with failed root canal treatment (Figure 4A). In light of the good quality endodontic treatment already provided, it was decided to provide surgical endodontic treatment with a retrograde TotalFill putty plug on both teeth. The postoperative radiograph confirms the presence of a well-sealed 2 mm apical plug in both canals (Figure 4B).
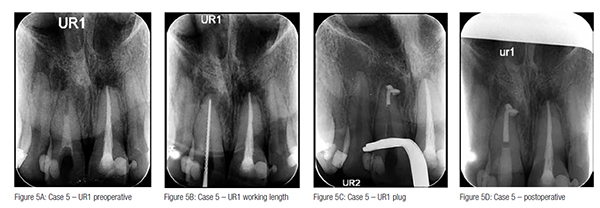
Case 5: open apex apical plug obturation UR1
A 24-year-old male patient presented with chronic periapical periodontitis affecting his non-vital immature UR1. Clinically, the master apical file was 80K at a working length of 20.5 mm. A TotalFill plug of 5 mm was provided, and the remainder of the canal was backfilled with gutta percha (Figure 5C). Unfortunately there was 2 mm extrusion of the apical plug with no postoperative complications (Figure 5D). No symptoms were reported postoperatively.
Case 6: open apex apical plug obturation UL1
A 13-year-old female patient presented with chronic periapical periodontitis, affecting her non-vital immature UL1 (Figure 6A). A TotalFill plug of 5 mm was provided under microscopic guidance, and the remainder of the canal was filled with injectable gutta percha (Figures 6B and 6C). A coronal seal was provided with Vitrebond™ (3M) and a composite restoration. There was 1 mm extrusion of the apical plug (Figure 6D).
Case 7: failed post crown and re-RCT UR1
A female patient attended with chronic periapical periodontitis associated with a failed post/crown and root canal treatment of the UR1 (Figure 7A). A decision was made to attempt to remove the post crown and perform re-root canal treatment via an orthograde approach. The canal was obturated using TotalFill sealer and thermoplastic gutta percha. The tooth was subsequently restored with a fiber post and replacement crown. The obturation of the root canal system is of a good standard terminating within 1 mm of the radiographic apex (Figure 7B).
Case 8: internal root resorption defect UL2
An 18-year-old male patient attended with chronic periapical periodontitis, affecting his UL2, which was also suffering from internal resorption in the mid third (Figure 8A). CBCT investigation revealed the extent and position of the lesion (Figures 8B and 8C). Further management involved the provision of root canal treatment with gutta percha obturation with TotalFill sealer used to obturate the resorptive defect (Figures 8D and 8E). The radiographic result confirmed a well-obturated root canal system/defect (Figure 8F).
Case 9: perforation repair UR2
A 26-year-old male patient attended with chronic periapical periodontitis, affecting his UR2, which also had evidence of a root perforation in the coronal third of the canal on the mesial aspect (Figure 9A). Further management involved use of TotalFill putty to seal the perforation with subsequent obturation with gutta percha. Radiographs confirmed presence of a well-obturated canal and defect sealed with TotalFill putty (Figure 9B).
Biocompatibility
Table 1 shows the percentage cell viability after application of TotalFill compared to MTA and AH+, highlighting the excellent biocompatibility of the material whereby after 3 days, there was 100% cell viability.
Results and discussion
TotalFill putty consists of calcium silicates, zirconium oxide, tantalum peroxide, calcium phosphate monobasic, and fillers. It is provided in a pre-loaded jar, pre-mixed, and can be directly applied. It sets upon exposure to moisture, is insoluble, radiopaque, and does not shrink on setting. The working time is up to 30 minutes. Setting time is a minimum of 2 hours, although it can take longer in extremely dry canals. There is no requirement to add liquid as sufficient moisture is provided by the apical tissues and dentinal tubules. Its consistency is such that it permits manipulation and placement with hand instruments without the need for a carrier unlike conventional MTA materials.
There are several advantages to this material. It has excellent handling characteristics and a shorter setting time than MTA. Its consistency is very much like temporary material Cavit® in that it adheres well to hand instruments and is very easy to pack. Its biocompatibility is similar to that of MTA (AlAnezi, et al., 2010) and, when set, produces a highly crystalline structure that enhances fibroblast adhesion and subsequent biomineralization (Jhingzhi, et al., 2011). Furthermore, during setting, the material produces a pH of 12, creating a highly alkaline and antibacterial environment further facilitating complete disinfection of the root canal system, and the sealer variant of TotalFill has been shown to have less microleakage than resin-based systems such as AH Plus® (Parwar, et al., 2014). Additionally, the omission of heavy metal oxides found in MTA eliminates the risk of tooth discoloration postoperatively.
The main drawbacks are the cost and perhaps the increased risk of apical extrusion in open apices cases. In this case series, there was more evidence of extrusion compared with MTA. The material does require less force to compact into an effective apical barrier, and perhaps due to its different handling capabilities coupled with limited operator experience, it makes it more likely to be extruded.
Conclusion
The cases treated show evidence that TotalFill is a valuable alternative to existing materials with a wide range of clinical indications and excellent radiographic and clinical results evident through its use.
References
- Alanezi AZ, Jiang J, Safavi KE, Spangberg LS, Zhu Q. Cytotoxicity evaluation of EndoSequence root repair material. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 2010;109(3):e122-5.
- Ma J, Shen Y, Stojicic S, Haapasalo M. Biocompatibility of two novel root repair materials. J Endod. 2011;37(6):793-798.
- Parwar S, Pujar MA, Makandar SD. Evaluation of the apical sealing ability of bioceramic sealer, AH plus & Epiphany: An in vitro study. J Conserv Dent. 2014;17(6): 579-582.
- TotalFill premixed bioceramic endodontic materials {Brochure]. La Chaux-de-Fonds, Switzerland: FKG Swiss Endo; Savannah, Georgia: Brasseler USA Dental; 2013.
Stay Relevant With Endodontic Practice US
Join our email list for CE courses and webinars, articles and more..