Drs. Hamid R. Abedi and Farzad Foroughi of Cornerstone Dental Specialties describe a new technique for flapless endodontic microsurgery.
Drs. Hamid R. Abedi and Farzad Foroughi explain a novel approach for flapless endodontic surgery
Introduction
It has been shown that endodontic microsurgery is the most cost-effective treatment modality for failing endodontically treated molar teeth.1 The success rate of endodontic surgery in a large study of 424 molars over 10 years shows an average of 84% to 88.5%.2 Another study shows survival as even higher at 94%.3 This is similar to the success rate of implants, which often uses less strict criteria for success relying on survivability and retention instead of success.4 There are very few studies looking at tooth retention comparing endodontic surgery and single-tooth implants.
What should a clinician do with a tooth that has not healed after conventional root canal therapy? The choices range from retreatment and/or new coronal restoration to endodontic microsurgery and extraction and replacement with a fixed dental partial or single-tooth implant. Over the past few decades, considerable advances have been made in both dental implants and endodontic microsurgery (EMS). Traditional endodontic surgery (TES) has been performed for over 100 years and consisted of anesthesia, raising a full-thickness flap, root-end resection, retrograde preparation of the apical part of the canal using a handpiece and bur, and placement of a root-end filling often in the form of amalgam.5

Current endodontic microsurgery (EMS) uses newer technologies in the form of enhanced lighting and magnification, often entailing the use of an operating microscope to better identify canals, fractures, and isthmuses; dyes to delineate lamina dura, piezo, or ultrasonic root-end preparation instruments facilitating accurate root-end preparation along the long axis of the root canal in a conservative manner without blocking visibility; and new root-end filling materials, such as mineral trioxide aggregate (MTA), and nano bioceramic materials that have improved leakage resistance, biocompatibility, antimicrobial properties, and moisture tolerance.6,7 In addition, better bone grafting and membranes can help in certain periodontal defects that can occur during surgery. Recent meta-analyses indicate that EMS is more successful than TES.8 Surprisingly, healing tends to occur more rapidly after endodontic surgery than conventional nonsurgical root canal therapy.9
With the increased usage of CBCT, there is undoubtedly an increase in the diagnosis of periradicular lesions and pathologies. Many studies have shown much improvement in diagnosis of periradicular lesions with CBCT compared to conventional periapical radiographs by a factor of 3 times to 4 times.10 Endodontic microsurgery is inherently a difficult procedure, and in the last decade, there have been efforts to simplify the procedure by using guides. CAD/CAM guides were used in 2007 to help with the osteotomy and root-end resection.11
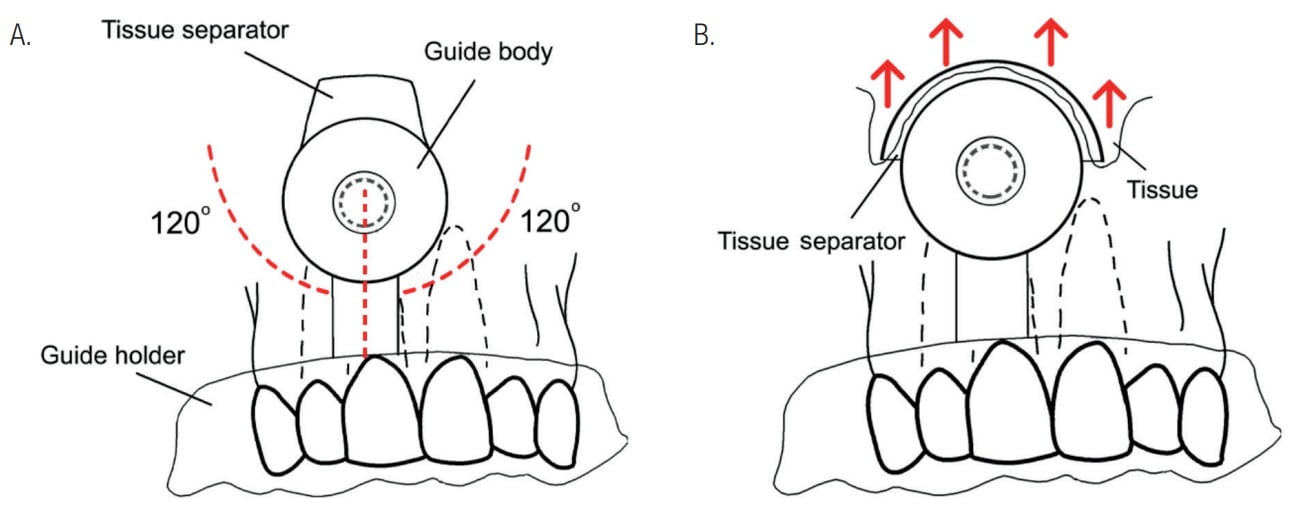
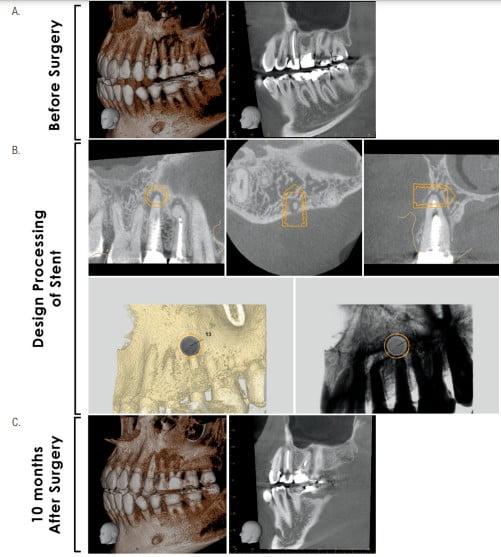
Guided endodontic microsurgery (GEMS) is a proven technique for treating failing nonsurgically retreated teeth. By using cone beam computed tomographic imaging (CBCT), design by CAD software, and 3D-printing technology, it is possible to address some of these challenging cases, while a small number of research articles and presentations in this area explain the use of a single surgical hard tissue guide adapted from implant surgery.12 There are limited comprehensive techniques that address both the hard and soft tissues in a flapless technique. The authors have developed a soft tissue guide that integrates with the hard tissue guide to allow minimally traumatic surgery for both the hard and soft tissues. The authors have performed more than 30 surgeries using the GEMS procedure and are currently working with the University of California, San Francisco, on clinical trials. In addition, there is exciting work being done to allow guided root-end filling placement. The GEMS protocol was written by the Cornerstone Specialty Products’ (CSPs’) R&D team (Protocol number CSP20210115-V2) and the surgical stent filed for patent in June 2018 (Patents number: US2020/0000549A1, US2020/0306008A1 and US2021/0022831A1). First, the doctor should take a full CBCT and intraoral scan of the patient. The intraoral scan must sufficiently cover enough buccal soft tissue up to the mesiobuccal fold. Many IO scanners allow operators to disable the artificial scan to extend beyond the limits of the attached gingiva. After completion, the DICOM and STL files are sent to CSPdental.com to design and create the GEMS guide.
Insert the trephine bur with the stopper attached into the surgical stent. Practice caution, and move slowly while drilling through bone until the stopper touches the stent body. In some cases, there is debris from the root tip or bone left in the surgical site. You can remove it with bone curette. The surgical site is flushed with copious amounts of sterile saline to remove soft and hard tissue debris, hemorrhage, blood clots, and excess root-end filling material. Before injecting the bone graft, take a radiograph to verify that the canal is properly prepared with the rotary instruments.
By developing a robust methodology, the authors can help clinicians perform the GEMS approach and maintain a natural dentition.
The GEMS method is wholly owned by Cornerstone Specialty Products (CSP), LLC. For information, visit www.cspdental.com.
Courses will be available, including live patient demonstrations. To register, go to www.ctidental.org.
Endodontic microsurgery is the future of endodontics. Endodontic specialists Bertrand Khayat, DDS, MSD, and Guillaume Jouanny, DDS, wrote a book entitled Microsurgical Endodontics that gives the reader access to videos by scanning QR codes. Read more about it here: https://endopracticeus.com/microsurgical-endodontics/.
- Kim SG, Solomon C. Cost-effectiveness of endodontic molar retreatment compared with fixed partial dentures and single-tooth implant alternatives. J Endod. 2011;37(3):321-325.
- Bliggenstorfer S, Chappuis V, von Arx T. Outcome of Periapical Surgery in Molars: A Retrospective Analysis of 424 Teeth. J Endod. 2021;47(11):1703-1714.
- Taschieri S. Fabbro M. Testori T. Weinstein R. Microscope versus endoscope in root-end management: a randomized controlled study. Int J Oral Maxillofac Implants. 2008;37(11):1022-1026.
- Norton MR, Wilson J. Dental implants placed in extraction sites implanted with bioactive glass: human histology and clinical outcome. Int J Oral Maxillofac Implants. 2002;17(2):249-257.
- Tsesis I, Rosen E, Schwartz-Arad D, Fuss Z. Retrospective evaluation of surgical endodontic treatment: traditional versus modern technique. J Endod. 2006;32(5):412-416.
- Wuchenich G. Meadows D. Torabinejad M. A comparison between two root end preparation techniques in human cadavers. J Endod. 1994;20(6):279-282.
- Torabinejad M, Pitt Ford TR, McKendry DJ, et al. Histologic assessment of mineral trioxide aggregate as a root-end filling in monkeys, J Endod. 1997;2:223(4)5-228.
- Setzer FC, Shah SB, Kohli MR, et al. Outcome of endodontic surgery: a meta-analysis of the literature–part 1: Comparison of traditional root-end surgery and endodontic microsurgery. J Endod. 2010;36(11):1757-1765.
- Iqbal MK, Kratchman SI, Guess GM, et al. Microscopic periradicular surgery: perioperative predictors for postoperative clinical outcomes and quality of life assessment. J Endod. 2007;33:239-244.
- Patel S, Dawood A, Mannocci F, et al. Detection of periapical bone defects in human jaws using cone beam computed tomography and intraoral radiography. Int Endod J. 2009;42(6):507-515.
- Pinsky HM, Champleboux G, Sarment DP. Periapical surgery using CAD/CAM guidance: preclinical results. J Endod. 2007;33(29:148-151.
- Strbac GD, Schnappauf A, Giannis K, Moritz A, Ulm C. Guided Modern Endodontic Surgery: A Novel Approach for Guided Osteotomy and Root Resection, J Endod. 2017;43(3):496-501.
Stay Relevant With Endodontic Practice US
Join our email list for CE courses and webinars, articles and more..

 Hamid R. Abedi, DDS, MS, MBA, has been practicing dentistry and is a former Assistant Professor at Loma Linda University, Department of Endodontics. He enjoys teaching endodontics and has lectured extensively in his specialty field both in the United States and abroad.
Hamid R. Abedi, DDS, MS, MBA, has been practicing dentistry and is a former Assistant Professor at Loma Linda University, Department of Endodontics. He enjoys teaching endodontics and has lectured extensively in his specialty field both in the United States and abroad. Farzad Foroughi, MBA, PhD in Biomedical engineering (Dental Materials), is a biomaterials and tissue engineering scientist with substantial hands-on experience in 3D biomaterials. His interests are in dental materials and dentistry devices design.
Farzad Foroughi, MBA, PhD in Biomedical engineering (Dental Materials), is a biomaterials and tissue engineering scientist with substantial hands-on experience in 3D biomaterials. His interests are in dental materials and dentistry devices design.