Drs. L. Stephen Buchanan and Christophe Verbanck say that minimally invasive endodontics can be achieved with a conservative taper like the miniKUT file system.
Drs. L. Stephen Buchanan and Christophe Verbanck discuss the benefits of files with conservative tapers
”You cannot clean a root canal with a larger file.” — LSB
Introduction
We are entering a new golden age of endodontics where instrumentation with root canal files is safer, easier, and more efficient. In 1980, when the senior author matriculated from his endo residency at Temple University, the most difficult art form in clinical endodontics was serial step-back (SSB) root canal shaping. Today, endodontic instrumentation can be as simple as cutting a single rotary file to length, and it’s time to irrigate and fill the RC system. This is the story about how we got here.
The Apical Stop Preparation
The Apical Stop Preparation (ASP) described by Kuttler,1 based on the standardized technique,2,3 gained widespread popularity at the end of the 1950s. The technique was to work small files to length, subtract 0.5 mm-1.0 mm from the full length of the canal as determined by radiograph, then progressively enlarge the preparation diameter at that working length to a minimum of 0.35 mm (a #35 KF) in small roots and to at least 0.45 mm (a #45 KF) in larger roots. The intention was to cut — using 1/4-turn, pull motions — an intentional ledge near the end of the canal as resistance-form to contain obturation materials within the canal and prevent overfills.4

The ASP’s unforgiveness of length determination errors, combined with the inaccuracy of radiographic length determination (before apex locator use was widespread), meant that clinicians preferred treating root canals short of their entire length, despite the fact that undertreatment of root canal systems was the most common cause of RCT failure (Figure 1).5,6 The predominant, yet illogical, expert opinion at the time was to stay short of the ends of root canals because we don’t want to damage any apical tissues, however, if the RCT fails, those same experts recommended apicoectomy (cutting off the apical third of the root) because that is where all the lateral canals are found. That is, in essence, saying, “a #10 KF passed through the root canal terminus is bad, but hacking the root end off and cutting all the bone around it is OK.”
In fact, all of our clinical experience and all of our evidence-based research has proven the importance of treating the entire root canal system.7
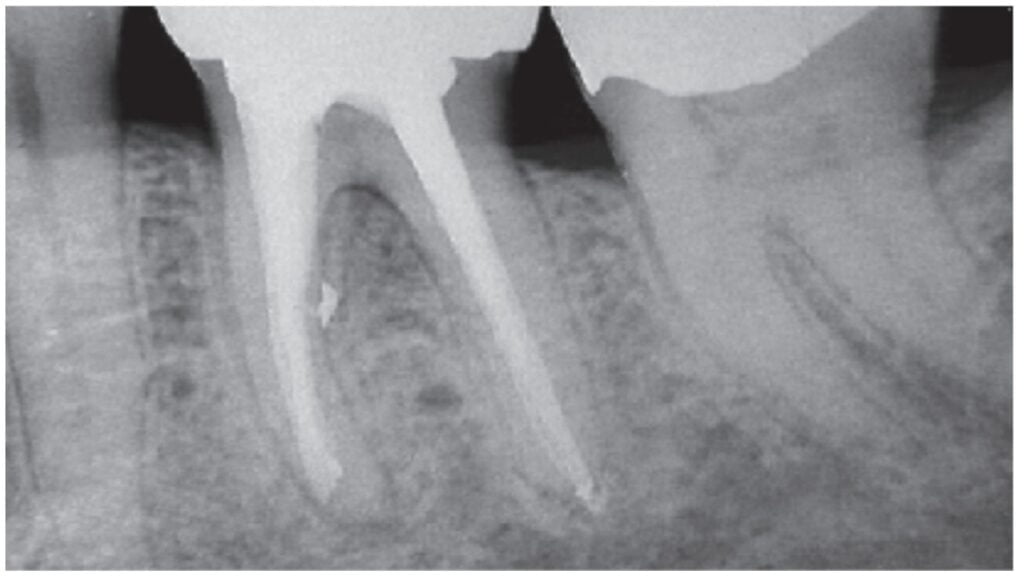
Worse than undertreatment, the ASP encouraged damage of delicate apical anatomy when increasingly larger, more rigid stainless steel files were forced to cut to working length. In 1975, Weine showed how 1/4-turn, pull motions with SS K-files transport apical canal paths, creating ledges in curved canals (Figure 2).8
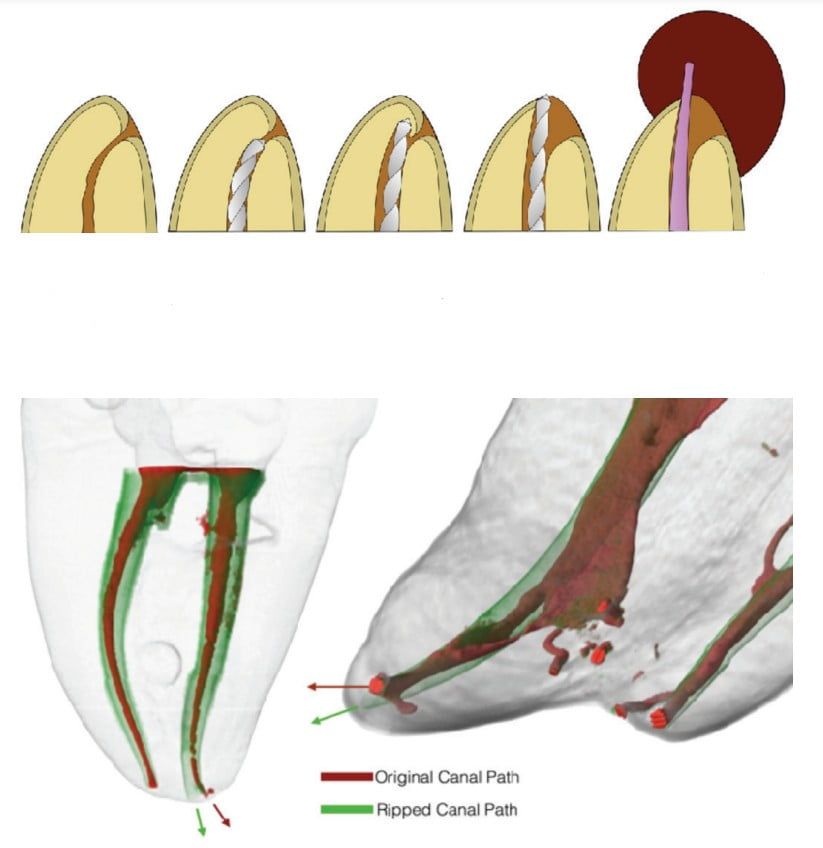
The ASP technique was the most common cause of overfills between 1950 and 1980 when most of the research correlating overfills with RCT failures was done (Figure 3). Sadly, only a few of the over 70 authors who published on this topic were able to understand that overextended filling material was coincidental to the failure, not the etiology for the failure. For the authors, this begs the question, “If the filling materials we use in endodontics must all pass regulatory biocompatibility tests, how does surplus filling material inhibit healing of periapical disease?” In fact, the belief that surplus filling material causes failure is a case of mass hysteria following mistaken etiology.9,10 Overfills are nearly always caused by derangement of the canal path during instrumentation (Figure 4).
The Schilder Serial Step-Back tapered preparation technique
In the 1970s, Dr. Herbert Schilder11 from Boston University popularized the “Serial Step-Back” (SSB) preparation technique, known for its large coronal shapes, its small apical preparations, and its incessant irrigation with sodium hypochlorite. For decades it was the most successful method of treating root canal systems to their full apical extents because he unapologetically espoused the use of patency files passed to and through the ends of primary canals to clear their apical thirds of pulp and dentin debris. Uniquely, his advice to keep the apical foramen as small as is practical empowered instrumentation and obturation of even the most dilacerated canals to their very ends, when clinicians cutting larger apical preps in small molar roots could never complete treatment at length — always ending up blocked out 1, 2, and even 3 mm short of the primary canal terminus.12
Schilder’s technique became best known for its post-op display of filled lateral canals because NaOCl was used to lavage canals after every other file was used, and nobody else in the specialty irrigated with that efficacy, so they seldom saw lateral canals filled. Because they seldom saw lateral canals filled, it was difficult for most of them to understand the importance of treating the commonly occurring lateral anatomy in RC systems. Meanwhile, Schilder and his acolytes cleaned and filled lateral anatomy routinely by using both his cleaning and shaping method as well as his “Vertical Condensation of Warm Gutta Percha” obturation technique.13
Schilder’s recommendation that clinicians cut bigger access cavities and bigger coronal canal shapes was logical considering the limitations of the instruments of his time, and at that time, dentist’s RCT results were improved by it. However, his enlargement concept has been obviated by the improvement of our material science, by the quality of our tool designs, and because the most progressive endodontists are currently pursuing minimally invasive access and shaping objectives. Sadly, some endodontists still equate overcut endo preparations with quality RCT.
Schilder was best known for his warm gutta percha obturation technique, however, in the author’s minds, his enduring legacy in the specialty pivots around his advocacy for tapered apical resistance form, maintaining the apical foramen’s original diameter, and for the irrigation technique embedded in his shaping routine. Until recently, Schilder’s critics didn’t understand how his cases succeeded despite what looked to them like under-enlarged apical preparations because few of them knew how to use NaOCl to its potential in their own cases. Fortunately endodontists are coming to realize that if you optimize irrigation protocols, you can achieve predictable clinical success without cutting any dentin.14 Schilder knew this 50 years ago.
Ultimately, Schilder’s greatest genius was in defining a better objective for clinical RCT, namely, treatment to the full apical and lateral extents of root canal systems.
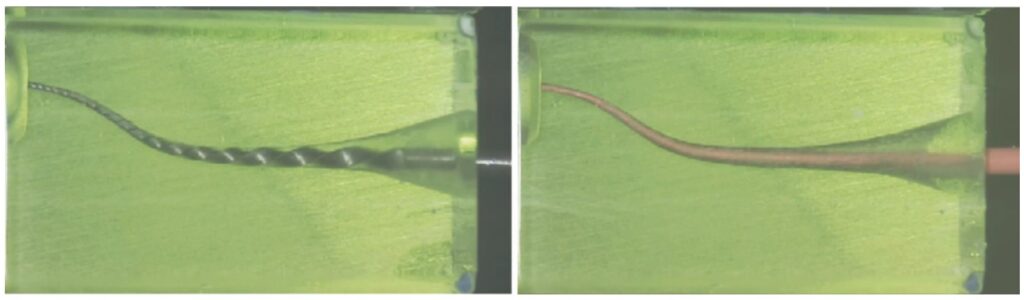
The variably-tapered rotary file revolution
Until 1989, there were no files with tapers greater than the ISO .02 mm/mm standard K-file, so SSB was the only way to cut a tapered prep with the relatively untapered files that were available. However, as the advantages of tapered preparations became apparent, the difficulties of learning, applying, and even teaching SSB shaping routines also became evident, eventually becoming the inspiration for files with greater tapers.15 By posing the question, “Instead of using 12-18 instruments in multiple recapitulations, why not just use a single file with a shape matching the tapered shaping objective?” The answer learned through the development process that followed was that stainless steel is too stiff and too weak for files of greater taper to work. Serendipitously, after prototying in stainless steel failed, nickel titanium came to endo from orthodontics,16 and suddenly variably-tapered shaping files became a reality (Figure 5).
Originally, the objective was to make files with the same shapes we cut during SSB shaping with stainless steel files, namely, .04, .06, .08, .10, and even .12 tapers. During this design process, it became obvious that files with these tapers would be too large at their shank ends if they all had 16 mm flute lengths, so the original GT Hand and Rotary Files were designed with 1.0 mm maximum flute diameter limitations. The first MIE file feature, 20 years ahead of its time, one could also argue the GT Hand File was the industry’s first single-file shaping instrument.
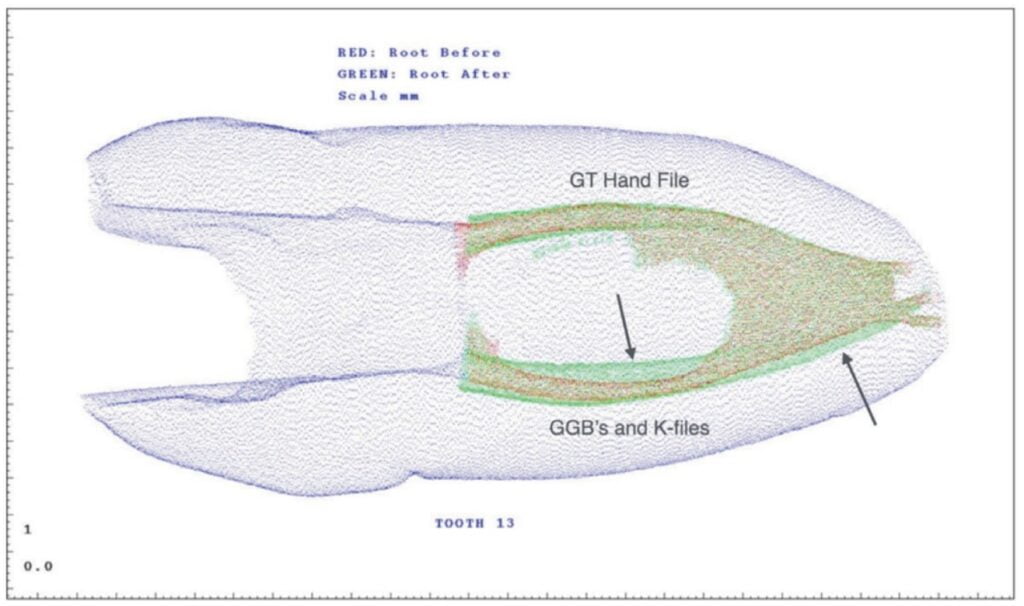
What we found out after giving files of greater taper to dental students (Figure 6)17 was that we did not need the same degree of taper with rotary shaping files that were required with SSB shaping because the quality of the shapes cut with variably-tapered files was so much more precise. Today most endodontists cut .06 tapers at the most, with many limiting their shaping files to .04 tapers and, with the advent of the miniKUT file system, even .03 tapers.
Current instrumentation concepts, tools, and procedures
In the 30 years since, conceptually, we’re finally beginning to accept the fact that to cut is not to cure when instrumenting canals. This offers so many advantages — less file breakage, less laceration of apical architecture, less post-op pain, fewer files to buy, and much less time spent using cutting instruments in canals. Successful MIE instrumentation does not revolve around using files; it hinges on upping our irrigation game. Files are the means, not the end. As proven to the authors by all the successfully treated canals done the past 5 years without cutting any dentin off a canal wall, just better irrigation.
The greatest improvement in our tools has been heat treatment of nickel-titanium files to remove the shape memory that is responsible for so many file separations due to cyclic fatigue.18,19 Before heat treatment, NiTi rotary files would exhibit what appeared to be spontaneous breakage. Now heat-treated files unwind and windup 9 or 10 turns backwards before they come apart. Heat-treated files cost less now than standard files did 10 years ago, so there is no reason for taking the greater risk of file separation associated with non-heat-treated NiTi files.
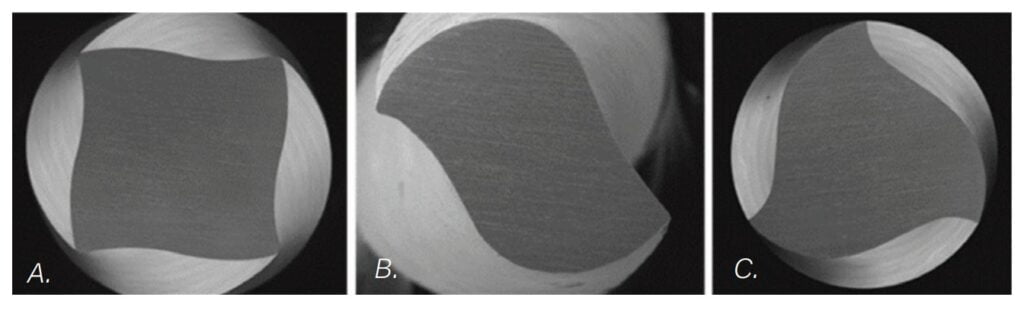
Another improvement in our tool design has been the realization that different file sizes in the same file set can never be optimized if they all have the same geometry. PlanB Dental’s miniKUT® MIE rotary files have variable geometry between their files; a square cross-section for their small EZPass rotary negotiating files, an aggressive two-bladed cross section in their shaping files, and three blades for their retreatment files (Figure 7). The advancements of variable geometry makes using rotaries as the “first files to length” a reality.20
Procedurally, the biggest sea change has been our realization that the mission of endodontic instrumentation is really only about confirming that canals have positive apical architecture before they are irrigated and filled. Once the apical diameter of the foramen has been determined — with gauging instruments, by observing whether there is debris in the last flutes of the first file of a larger diameter cut to length, and even with analysis of pre-op CBCT volumes as they display anatomic dimensions in an isotropic 1:1 scale21 — the only shaping requirement is that the narrowest canal diameter be at the terminus of the canal.

If the natural canal has an ideal shape preoperatively (most common in young adult teeth), the instrumentation plan is to broach the pulp, irrigate the canal, and stuff it. When we encounter canals with reverse apical architecture, meaning the narrowest diameter is coronal to the terminus, then our only instrumentation objective is to cut a shape that repositions the narrowest diameter in the canal to the end of the canal. So, the evolution of Endodontics has approached nearly prepless RCT where chemical cleaning will always play the most significant role (Figure 8).
Recently, reciprocation was touted as the key to single-file shaping, which is patently not true. The two authors, between them, have done thousands of single-file shaping cases with a myriad of rotary files years before reciprocation even existed. This shined a spotlight on the big advantage of rotary cutting tools — to effectively remove pulp tissue and dentin chips from apical regions instead of pushing them laterally and apically — it also revealed that reciprocation was a step backwards.22

State of the art of instrumentation
The current trend among progressive endodontists is toward the application of minimally invasive endodontic principles (Figures 9 and 10). An excellent example is the miniKUT file system of instruments, with conservative tapers of .03 and .05. The unconventional .03 taper is at the low end of the natural taper of small root canals and will work even if the canal has an even smaller or non-tapered canal outline, an extreme curvature, or apical impediment. The .05 taper is closer to an SSB tapered preparation with 1 mm step-back increments and creates the right amount of space for all contemporary methods of irrigation. Used at speeds ranging between 600 and 900 RPMs, their cutting efficiency feels effortless even in long canals. These rotational speeds create centripetal forces that center the file and keep the flutes from stalling against the root canal wall during preparation. They can be used for rotary negotiation (the 15-.03 and 15-.05 EZP) as well as “single-file shaping” with minimal coronal enlargement.

One of the author’s referring prosthodontists once told him that if endodontists could just “suck the pulp out and not cut any dentin” he would be happier. Specialty Endodontics has spent the past 30 years delivering on that virtuous aspiration. The irony of these sea changes in the art and science of instrumentation is that as our conceptual understanding of our mission became more sophisticated, procedural instrumentation became inordinately simple.
Look for our next article, “Irrigation: The Final Frontier,” in the fall edition of Endodontic Practice US.
- Kuttler Y. Microscopic investigation of root apexes. J Am Dent Assoc. 1955 May;50(5):544-552.
- Seidler B. Root canal filling: an evaluation and method. J Am Dent Assoc. 1956 Nov; 53(5):567-576.
- Ingle JI. A standardized endodontic technique utilizing newly designed instruments and filling materials. Oral Surg Oral Med Oral Pathol. 1961 Jan;14:83-91.
- Kerekes K, Tronstad L. Long-term results of endodontic treatment performed with a standardized technique. J Endod. 1979 Mar;5(3):83-90.
- Hess W, Zürcher E, Dolamore W. The anatomy of the root-canals of the teeth of the permanent dentition. New York NY: William Wood and Co.; 1925.
- Coolidge ED. Anatomy of the root apex in relation to treatment problems. J Am Dent Assoc. 1929; 16:1456-1465.
- Arias A, Azabal M, Hidalgo JJ, de la Macorra JC. Relationship between postendodontic pain, tooth diagnostic factors, and apical patency. J Endod. 2009 Feb;35(2):189-192.
- Weine FS, Kelly RF, Lio PJ. The effect of preparation procedures on original canal shape and on apical foramen shape. J Endod. 1975 Aug;1(8):255-62.
- Ricucci D, Langeland K. Apical limit of root canal instrumentation and obturation, part 2. A histological study. Int Endod J. 1998 Nov;31(6):394-409.
- Siqueira JF Jr. Aetiology of root canal treatment failure: why well-treated teeth can fail. Int Endod J. 2001 Jan;34(1):1-10.
- Schilder H. Cleaning and shaping the root canal. Dent Clin North Am. 1974 Apr;18(2): 269-296.
- Senia ES. Canal diameter: the forgotten dimension. Dent Today. 2001 May;20(5):58-62.
- Schilder H. Filling root canals in three dimensions. Dent Clin North Am. 1967 Nov: 723-744.
- Buchanan LS. Chapter 7: Cleaning and Shaping Root Canal Systems. Pathways of the Pulp 5th ed. Mosby-Yearbook 1989.
- Buchanan LS. The art of endodontics: files of greater taper. Dent Today. 1996 Feb;15(2):42, 44-6, 48-9 passim.
- Walia HM, Brantley WA, Gerstein H. An initial investigation of the bending and torsional properties of Nitinol root canal files. J Endod. 1988 Jul;14(7):346-351.
- Gluskin AH, Brown DC, Buchanan LS. A reconstructed computerized tomographic comparison of Ni-Ti rotary GT files versus traditional instruments in canals shaped by novice operators. Int Endod J. 2001 Sep;34(6):476-484.
- Kwak SW, Shen Y, Liu H, Wang Z, Kim HC, Haapasalo M. Heat treatment and surface treatment of Nickel-Titanium Endodontic instruments. Dent. Med. 2021, 2: 769977. https://www.frontiersin.org/articles/10.3389/fdmed.2021.769977/full. Accessed February 14, 2023.
- Pruett JP, Clement DJ, Carnes DL Jr. Cyclic fatigue testing of nickel-titanium endodontic instruments. J Endod. 1997 Feb;23(2):77-85.
- Buchanan LS., Verbanck CLM. Rotary negotiation as first file to length. Endodontic Practice US. 2022; 15(4): 24-26.
- Scarfe WC, Farman AG, Sukovic P. Clinical applications of cone-beam computed tomography in dental practice. J Can Dent Assoc. 2006 Feb;72(1):75-80.
- Bürklein S, Benten S, Schäfer E. Quantitative evaluation of apically extruded debris with different single-file systems: Reciproc, F360 and OneShape versus Mtwo. Int Endod J. 2014 May;47(5):405-409.
Stay Relevant With Endodontic Practice US
Join our email list for CE courses and webinars, articles and more..


