Dr. John West discusses four more reasons why anatomy should matter
Introduction
After nine installments of Anatomy Matters,1-9 I am beginning to feel like a broken record. So, I am writing Anatomy Matters, Part 10, by taking a different perspective — rather than continuing to write about endodontic patient treatments that fail due to underfilled root canal systems, my objective is to pique your interest in a new way, by telling you that the future standard form of procedure reimbursement will be how well endodontists can prove they have filled the cleaned root canal system. It will be called “Pay for Performance” (PFP). Check out QForma on the Internet and begin to be educated that we are being graded; we are being measured; we are being watched.

I have divided my article into four sections: 1) Anatomy and fees, 2) Anatomy and reputation, 3) Anatomy and longevity and 4) Anatomy and because.
Four proofs that anatomy matters
1. Anatomy and fees
What this means is that some day (sooner than we think), insurance companies, government, and the consumer (our patients), will know the following:
- how good dentists’ crown margins are
- the rate of their veneer success/failure
- the number of healthy teeth in the dentists’ patient population
- if their root canal obturations are solid
- if their endodontic preps have continuously tapering funnel shapes
- how clean the clinicians’ root canal systems are
- how many visible portals of exit (POEs) they fill per shaped canal
These will be the quantified measurements that will determine our value and, therefore, our fees (Figure 1).
Forget that anatomy matters to some and not others. I do know this, that endodontists want more patients. And if endodontists are truly going to be paid on performance, and the pretreatment and posttreatment radiographic images are our only metric, then biologic success is not the only reason to make the perfect access cavity, to remove all dentin triangles, to prepare a glide path to the canal terminus no matter what, and to produce appropriate shapes that protect the ferrule and yet are sufficient for gutta percha and sealer fluid hydraulics for 3D obturation.
You may say that fee-for-service is never going to be based on the radiographic quality of my obturated properly shaped root canal system, let alone the number of POEs visibly sealed on a periapical radiograph. Who’s counting? Maybe we should take a cone-beam computed tomography (CBCT) 3D posttreatment image, too, in order to grade and pay for our technical result. I believe that your referring dentist is counting and that your reputation is counting.
2. Anatomy and reputation
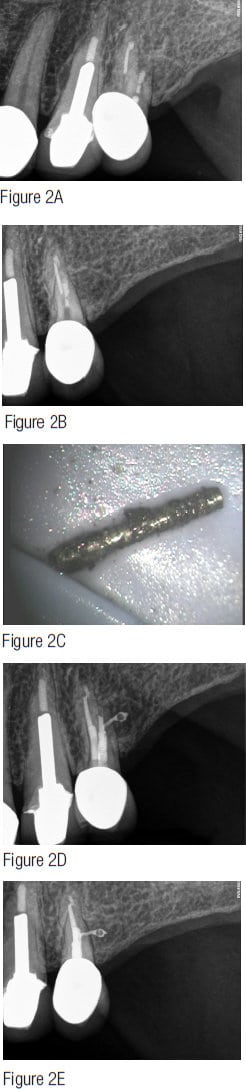
Realistically, I don’t think any PFP future is near in time, but the quality of our measured technical result (the radiographs or digital imaging) does influence the endodontist’s reputation and, quite frankly, our “busy-ness” (Figure 2). For example, if an endodontist cannot predictably perform the big three “F’s” — find all the canals, follow all the canals to their termini, and finish the canals (smooth, funnel shape, 3D clean, conefit, and 3D obturation, or at least the appearance of 3D obturation) — then the word gets out pretty fast, and that endodontist suddenly finds himself or herself competing for referrals not in the top 10% of the market but the bottom 10%. The bottom 10% seems willing to treat for the lowest fee to get some referrals. Often the bottom 10% number of referrals is insufficient for significant profitability, and these patients often lack dental value. Either way, competing in the bottom 10% is dissatisfying, de-energizing, and physically and emotionally exhausting. At least for me, when I go faster or base my treatment on time, I begin to risk making mistakes. I block; I tear; I break things. None of these outcomes is good for the reputation.
3. Anatomy and longevity
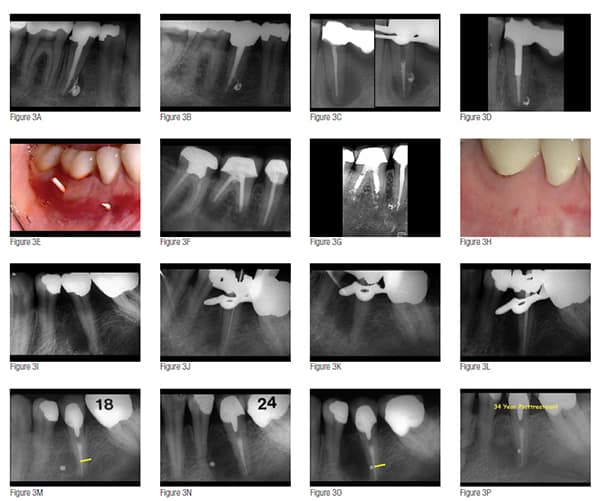
It’s time for me to get off my “strive for quality” soapbox. Let’s just surmise that I have not made a good argument: Our fees will never be based on a radiographic image, and referring dentists don’t care about the only measure of quality, aside from patient feedback, available — the X-ray or image that the endodontist sends back to the dentist after endodontic finish. Is there any other reason to do our best and operate as if anatomy matters? Yes, the better that root canal systems are obturated, the longer they last, and the better the patient investment in saving endodontically diseased teeth.10 And since our population is aging, each new decade requests that dentistry, including endodontics, must last a longer time. It must be built to last (Figure 3).11
4. Anatomy and because
The following text is an excerpt from John F. Kennedy’s “Moon Speech” at Rice University on September 12, 1962:
We choose to go to the moon. We choose to go to the moon in this decade and do the other things, not because they are easy, but because they are hard, because that goal will serve to organize and measure the best of our energies and skills, because that challenge is one that we are willing to accept, one we are unwilling to postpone, and one which we intend to win. … Many years ago the great British explorer George Mallory, who was to die on Mount Everest, was asked why did he want to climb it. He said, “Because it is there.”
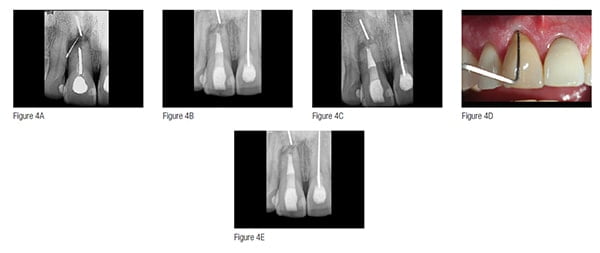
“Because it is there.” Well, consistently performing great endodontics is here; and while great endodontics has never been rocket science, it has always taken a certain willingness, and it has always, like the race to the moon, served to organize and measure “the best of our energies and skills” (Figure 4). It may be that the anatomy doesn’t matter. The LEO may not develop, and the LEO may heal regardless of the quality of the Endodontic Seal.
Instead, it is the “Because” that is the because.
Conclusion
For the purposes of this 10th installment of Anatomy Matters, I have suggested that there are at least four reasons to consider doing better endodontics and that anatomy does matter: 1) value, 2) reputation, 3) longevity, and 4) because. I would offer that for most of us, we can do better endodontics by simply slowing down, improving technical skills, or simply being more intentional. I believe any of us can do as much as we want. Start with the easy cases, and then move to the more complicated. While some people intend on having you do endodontics at a lower, lower, lower level, I guess I am intent on having you do endodontics at a higher, higher, higher level. And I have enough experience of not only doing endodontics but also teaching it that I am right, and it can be done. Professor Herb Schilder once said, “It’s not hard to be the best. There’s no competition.” Compete in the top 10%; there is less competition there. But really, to me, this means compete in the top 10% of your own personal potential. Being and doing your best in delivering endodontic excellence has nothing to do with measuring how good I am compared to you. It has to do with how good I am compared to me.
- West J. Anatomy matters. Endodontic Practice US. 2012;5(2):14-16.
- West J. Anatomy matters — part 2. Endodontic Practice US. 2012;5(4):26-27.
- West J. Anatomy matters part 3. Furcal endodontic seal heals furcal lesion of endodontic origin. Endodontic Practice US. 2012;5(6):22-24.
- West J. Anatomy matters. Long-term case report. Endodontic Practice US. 2013;6(1):50-51.
- West J. Anatomy matters. Root canal system anatomy only matters when it matters. Endodontic Practice US. 2013;6(2):56-58.
- West J. Anatomy matters. Do lateral canals really matter? Part 6. Endodontic Practice US. 2013;6(3):52-53
- West J. Anatomy matters. “What’s it all about?” Part 7. Endodontic Practice US. 2013;6(4):52-54.
- West J. Anatomy matters. “Could it all simply be a coincidence?” Part 8. Endodontic Practice US. 2013;6(5):52-55.
- West J. Anatomy matters. Endodontic accountability: The “X” factor, part 9. Endodontic Practice US. 2014;7(1):43-47.
- West JD. Implants versus endodontics: “As the pendulum swings.” Dent Today. 2014;33(1):10-12.
- Kurzweil R. The Singularity is Near: When Humans Transcend Biology. New York, NY: Penguin; 2005.
Stay Relevant With Endodontic Practice US
Join our email list for CE courses and webinars, articles and more..


