Dr. Nishan Odabashian discusses treating teeth with failing previous root canal treatment exhibiting large radiographic lucencies less invasively
Introduction
A healthy 22-year-old male presented to our office on March 1, 2011, after his mother, a previous patient, insisted that he obtain a second opinion. He was referred to an oral surgeon by his general dentist and was advised that he would need extensive surgery in his lower right mandibular molar area which would include removal of the first and second molars.
[userloggedin]
Clinical and radiographic examination
Clinical findings
The patient had a crown on tooth No. 30. He had an occlusal amalgam restoration on tooth No. 31. He had visible slight-to-moderate intraoral and extraoral swelling in the lower left molar area (Figure 7). He had moderate-to-severe pain on palpation and percussion of tooth No. 30, slight pain to percussion on tooth No. 31, and neither palpation nor percussion sensitivity on tooth No. 29. Both teeth No. 29 and No. 31 responded normally to cold sensitivity testing.
Radiographic findings
Panoramic, periapical, bitewing, as well as 3D imaging pointed to a large unilocular lucency apical to tooth No. 30 and tooth No. 31. The lucency extended almost the entire corono-apical length of the mandible (Figure 2). Tooth No. 30 had a previous root canal treatment (longer than 10 years ago, according to the patient). The tooth had a screw-type post, a PFM crown, with apical resorption apparent in both mesial and distal roots of both tooth No. 30 and tooth No. 31.
Medical history
Non-contributory. Slight fever and swelling on the right molar area upon presentation.
Diagnosis
- Pulpal: Pulpless — previously treated root canal
- Periapical: Symptomatic peri-radicular abscess
Differential diagnosis
- Lesion of endodontic origin
- PA Cyst
- Keratocystic Odontogenic Tumor (KCOT) formerly Odontogenic Keratocyst (OKC)
- Central Giant Cell Granuloma
- Ameloblastoma
- Other
Immediate treatment plan
Incision and drainage (I&D)
Initiate retreatment, and based on results, send for biopsy or continue with endodontic retreatment.

 Treatment
Treatment
Retreatment was initiated by isolating with a rubber dam, accessing the crown, removing the core and the screw post from the distal canal, as well as the removal of gutta percha from all canals. A sero-sanguinous exudate rushed into the chamber, (Figure 5), which was flushed with copious amounts of sodium hypochlorite. The tooth was left to drain for approximately 30 minutes. The canals were then irrigated, dried, and dressed with calcium hydroxide (Figure 6).The tooth was temporized with Cavit™ (3M ESPE). This was followed by an I&D of the buccal swelling. The patient was prescribed clindamycin 300mg, 2 tabs immediately, and 1 tab 3 times a day for 5 days.atient presented 5 days later, and his facial as well as buccal swelling (Figure 9) was considerably better. His symptoms had become tolerable, and retreatment was planned to continue.





Patient was seen monthly with further cleaning of the canals and replacement of the calcium hydroxide paste.
The tooth was obturated with MTA, on August 17, 2011, and apical surgery was planned to remove the thin gutta-percha points, which extruded into the periapical area during retreatment (Figure 14) at the next scheduled appointment.
Follow-up
The patient missed his surgery appointment due to his college classes. He rescheduled in December 2011 during his Christmas break. He presented in December but did not want to have surgery during his Christmas break, and said that he has been asymptomatic since April. He asked if surgery was absolutely necessary and was advised that it would be best if he had the surgery, but was not absolutely necessary. He was given a follow-up during spring break, and he was still asymptomatic and asked if the surgery could be delayed until the summer.
Follow-ups continued every 3 months with the patient declining surgery each time.






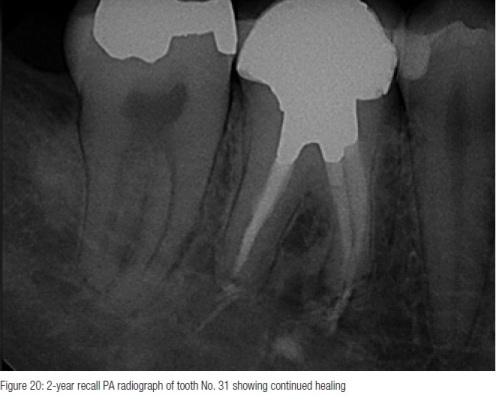

The radiographic presentations (see below) show continued healing of the periapical area. Tooth No. 31 shows complete osseous healing and normal response to temperature testing. Tooth No. 30 shows almost complete osseous resolution of the large radiolucent area, and the patient continues to be asymptomatic.
Discussion
This case presentation is the second in a series of teeth exhibiting large periradicular lucencies associated with failing root canal treatments. (The first article in the series appeared in Endodontic Practice US, May/June 2014, Volume 7, No. 3.) As mentioned in the previous report, treatment of teeth with large lucencies requires more than the garden-variety retreatment or surgery. It requires time, patience, proper follow-up, sound restorative treatment, proper diagnosis, and involvement of other specialists as necessary.
In this instance, the 22-year-old male patient was slated to go through an extensive surgery with the loss of two molar teeth. And although neither the general dentist nor the oral surgeon can be faulted for the treatment that was about to be rendered, it helps to take a step back and think the treatment through given the clinical presentation.
The fact that there was an intraoral and extraoral swelling associated with a previous root canal treatment pointed this clinician to a diagnosis of lesion of endodontic origin. Also, the titrated-type treatment that was rendered, allowed us to “throw in the towel” if the signs and symptoms were not improved. At such time, some type of biopsy would have been performed to render the appropriate treatment for the condition.
This case also shows the capacity of the body to heal if and when the offending insults are removed. It shows the result of patience and taking the time to perform the most conservative dental treatment possible. It would have been much easier to “just extract” and, after extensive surgery and grafting, to place two implants and implant-supported crowns. It was much more time-consuming for this clinician, but also much more rewarding. The treatment rendered was much less invasive, much less expensive, and much less morbid.
Summary
This case shows what is possible with endodontic treatment/retreatment as far as osseous healing of large periradicular lucencies. This case also shows the benefit of multi-visit endodontic retreatment. Titrated treatment, a term that was coined by Dr. Gary Carr, is very useful in these types of cases. It allows for re-evaluation of the results (or lack thereof) during the course of treatment.
[/userloggedin]
[userloggedout][/userloggedout]
Stay Relevant With Endodontic Practice US
Join our email list for CE courses and webinars, articles and more..










