Dr. Judy McIntyre tells how CBCT imaging can help clinicians to better diagnose and treat both pediatric and adult patients.

Why did you become an endodontist?
I always knew I wanted to be a dentist. As a child, I had a traumatic dental injury, and I had positive experiences with my dentist; I wanted to be able to provide the same kind of care to others. I’ve always enjoyed working with my hands, and endodontics suited my skill set and personality.
During my residency at the Adams School of Dentistry (UNC-Chapel Hill), I was fortunate to have great mentors and was exposed to many dental trauma cases. In my practice, Hopkinton Endodontics, I treat pediatric and adult patients with dental trauma as well as my traditional endodontic patients, so I can combine both passions. It’s the perfect fit.
What is the most rewarding aspect of your practice?
I find it incredibly rewarding to save teeth and relieve patients’ pain. Being able to put patients at ease and give them their smiles and confidence back is very gratifying. Our pediatric patients are surprisingly good; typically they have fewer past dental experiences, and with the right approach, they turn out to be very cooperative with local anesthesia alone! The parents are so appreciative, especially when they’ve previously been told that nothing can be done for their children/tooth. My young patients with dental trauma have a lot on the line — trying to save a tooth in a growing patient. Treating kids is extremely rewarding.
I also find current technology such as CBCT imaging helps to identify the cause of patients’ pain and to treat issues that have been missed or misdiagnosed. Often, patients have seen other practitioners and have been told that everything appears normal. It makes my day when I’m able to reveal the cause of their pain and problems, to show them on their 3D scan that they were correct in thinking something was not quite right, and then correct and treat the issue. The patients are extremely grateful and relieved. My CBCT unit plays a key role in that.
As endodontists, our priority is to save teeth whenever possible. Sometimes we forget that; we’re doing more than just a root canal procedure — we’re preventing or treating apical periodontitis — we are saving teeth! CBCT enables me to save more teeth and do it more predictably; patients appreciate when they can avoid losing the tooth.
When did you start using CBCT in your practice?
I was first introduced to cone beam technology during my endodontics residency. UNC had a CBCT unit and was one of only a few institutions in the country that did almost 20 years ago. At the time, the technology was new, and we didn’t use it often. Reflecting back, I wish we had used it more. In residency, I planned an autotransplantation on a patient in her early 20s whose lower left first molar had to be extracted. My plan was to move her upper right third molar to the extracted tooth’s position. I measured for this using a panoramic x-ray unit and ended up being far off — even after calculating for the known magnification of the pan. I published a paper about this case. Although it was successful, I could’ve done it better had I used the CBCT with more accurate information while I was planning. That was my first of many aha moments that has helped to shape my current imaging protocols.

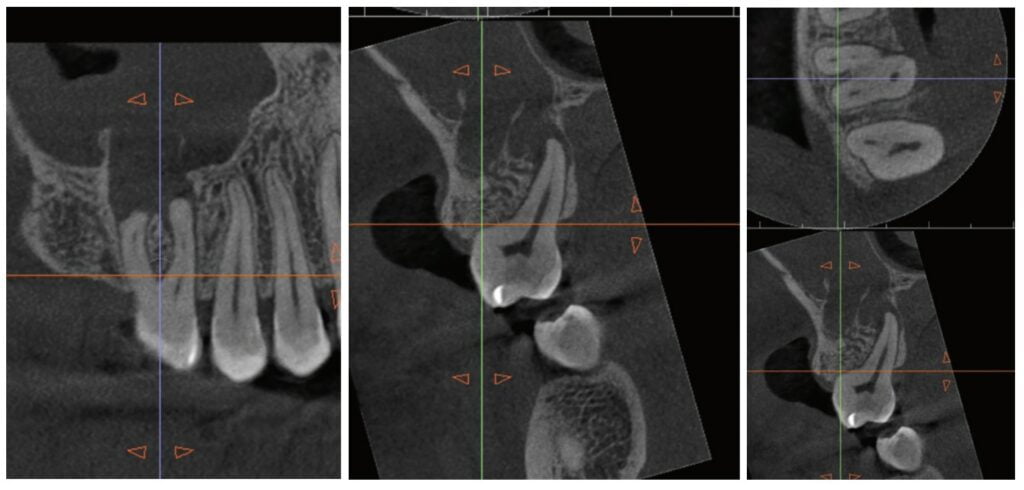
About 10 years after completing residency, I opened my own practice and invested in a DEXIS CBCT. Initially, I only used it for apicoectomies and retreatments. In time, I began to realize how helpful it was for all my cases. With the 3D-scan information (Figure 1), I could have saved myself some humbling experiences and surprises. Endodontists hate surprises, and we really hate failures! Once I started using my CBCT more frequently, I was able to appreciate things that would have otherwise been intra-op surprises and plan for them prior to starting the procedure. The 3D data allows me to properly assess prognosis, determine the best course of treatment, and plan that treatment with a level of precision that is impossible otherwise.

CBCT also allows me to capture issues I might have previously missed, whether related or solely incidental findings. Practitioners can visualize pathology/issues even when a patient is completely asymptomatic. I had a patient referred to me with an issue on one tooth. Cone beam revealed the patient had four teeth that unfortunately needed extractions, and all previous imaging gave no indication of this. Another patient presented for one tooth, but the CBCT showed several cracked molars and a perforated post. I was able to properly diagnose those problems as well. Sadly, those couldn’t be saved with endodontics, but knowing that up front saved time, unnecessary treatment, and resources for the patient.


On a recent second molar case where I did not take a 3D scan prior to root canal treatment, the patient returned several days later still in pain! I took a scan and appreciated their deep split, forked in the last 5 mms of the distal canal (Figure 8). Without a CBCT scan, it’s easy to miss — I did! CBCT helps prevent this from happening by catching those variants and hard-to-find issues, which are not as rare as we think. This was another case that helped shape my current imaging protocol, so that now I scan nearly all of my patients. I honestly can’t imagine practicing without my CBCT unit — similar to when the microscope was introduced to endodontics.
As I did not train with CBCT in residency, I really did have to “invest” the time into improving my interpretation with it. I purchased a CBCT/endodontics book, attended every webinar and lecture I could, began working more closely with oral radiologists, and did more training with my DEXIS Imaging Specialist, Ryan Zager. All of these were really worthwhile, and I’m still learning, but now I can better distinguish a true crack from beam hardening, etc. I feel way more confident in my interpretation. I have to thank DEXIS mainly for that. Their technology and support is unparalleled.
How has CBCT affected your patient experience and outcomes?
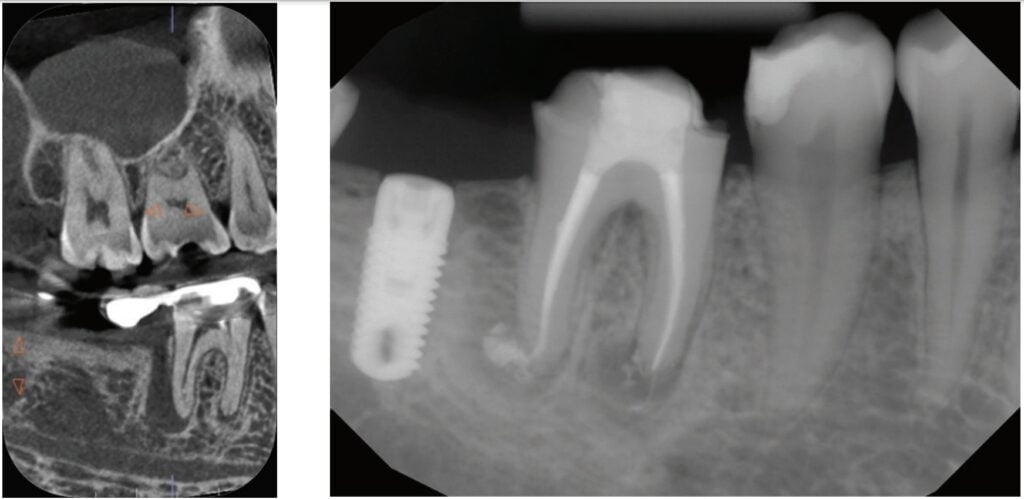
CBCT has greatly improved the patient experience. As an endodontist, a good portion of the teeth I’m treating have already had endodontic treatment. CBCT allows me to figure out why the root canal didn’t work the first time: Sometimes there is a missed canal or a fracture. If something is failing, I need to know why it is failing in order to plan my treatment appropriately and to give the patient the best chance of saving the tooth, as well as a realistic prognosis. Unfortunately, not all teeth can be saved. Some are not candidates for retreatment (Figure 11). Without a CBCT scan, it would be easy to attempt these retreatments only to discover the true problem mid-treatment, or worse — to think I had caused one (Figures 10 and 11). This added information not only helps the practitioner, but also provides patients a higher level of confidence and trust in you.
With retreatments, maybe the root canal looks completely fine on a PA or panoramic x-ray, but the patient says that it just doesn’t feel right. A cone beam can often reveal the cause of the patient’s discomfort. This could be that the tooth was perforated, cracked or has an unfilled canal, and the patient is totally justified in feeling like something’s wrong. Or sometimes the scan will show that there is another issue on an adjacent tooth or in the patient’s sinuses (causing their discomfort). When patients sense a problem but are told that there is not one (usually based on 2D radiographs), that’s not a great feeling. Being able to show the patient the CBCT scan and say, “You were right, and here’s the issue,” improves the patient experience.

I also find with 2D radiographs, patients don’t always understand what we’re trying to share with them in the image, even when they say they do. However, I’ve noticed when I review a 3D scan with patients, their eyes widen and they start nodding, especially when reviewing their volume rendering; it’s definitely helped with patient education and case acceptance. They see their teeth, their jaw, the infection in their bone (as a hole), and they understand this since they recognize themselves in 3D. This better understanding makes them more likely to accept the recommended treatment plan, leading to better outcomes. Ultimately, the patient is glad we took the CBCT scan. They’re thankful to have that information.
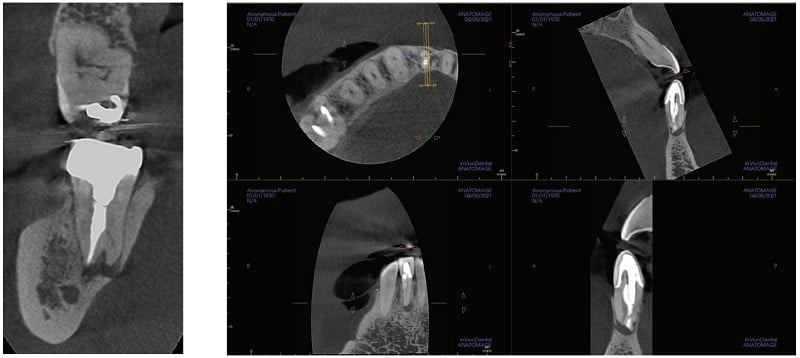
I also see a good amount of resorption cases. Without the scan, I can’t determine how large or destructive the lesion is. I cannot accurately determine the best course for these resorptive cases without knowing what they look like in 3D (Figure 3). I might approach it surgically without endo, or I might plan only for the endo and monitor it after. And, some cases need both at the same time, or closely planned together, or a resorptive defect could be taken care of internally with the endo — all of that thought and planning comes from the scan; usually not possible with 2D imaging alone.
How has CBCT changed your treatment approach?
CBCT has transformed the way I treat patients in many ways. First, with cone beam, I can confidently offer a realistic prognosis on a tooth. Sometimes this means no treatment, saving me — and the patient — the time of pursuing a treatment that may not work, or has a poor prognosis.
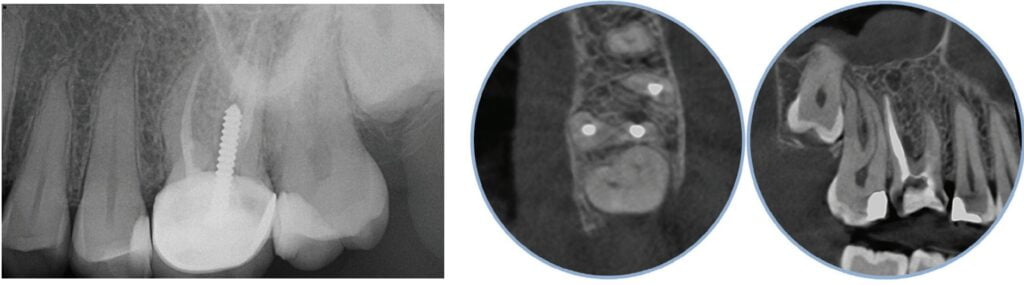
The 3D scan also provides essential information to better treatment planning. Sometimes, this means knowing exactly the number of canals in a tooth, instead of hunting and based on what the literature suggests. And, when I know how many and where the canals are (Figure 13), I can take measurements on the scan and work more efficiently — measuring my working lengths of each canal, appreciating severe curves or calcifications, and knowing where canals can be expected to be located, again, rather than removing unnecessary tooth structure to find if it is there, or not!

As an endodontist, I often treat heavily restored teeth. I am often planning my accesses based on the scan’s information. This saves time and conserves more tooth structure. I’m not looking for canals that may or may not be there, and I’m looking for canals under the targeted/planned access — with the scan, I have an actual map (Figure 7)! CBCT directs me where to go and where to end. It reveals anomalies, which are more common than we think, so I can avoid iatrogenic incidents and provide less invasive treatments. Lower second molars with only two canals occur — often!
I’m also changing my treatment plans based on the data from my CBCT. Sometimes I look at a root canal treated PA and presume I know what I will do: a retreatment or an apico. Another recent, poignant case: a lower incisor with a previous RCT and a previous apico (Figure 9). Usually, once a tooth has had an apico, there may not be much left to offer and most of the time, the default is another apico, especially as there was very little room for an implant on the lower anteriors. I scanned the tooth and saw that a whole canal had been missed — twice! The RCT and the apico had left the buccal canal completely untouched. I changed my treatment plan based on this information!
Cracked teeth are also quite prevalent (Figure 12). Of course, I can suspect them clinically and with transillumination and other tests, I’m fairly confident in my diagnosis. Thankfully, the 3D scan proves it and shows the depth of these cracks and the angular defect. Without a CBCT, sometimes these cases are started unnecessarily.
Lastly, using CBCT also allows me to find issues that should be evaluated by another specialist. For example, when I capture incidental sinusitis, I can inform my patient to see an MD or ENT and can provide the 3D images to share with their physicians; or, to involve another dental specialist. (Figures 2, 4, 6, and 11 show incidental sinus findings.)
What advice would you give to your younger self?
I would tell my younger self that CBCT is as important of a tool for endodontics as a microscope and that I should get proficient with it early. I wish I had started using cone beam technology a lot earlier, on a lot more cases. Thankfully, I had tremendous support from DEXIS to help with my 3D-learning curve, but I wish I had become better with it earlier so that I could have used it to its potential even earlier.
What does the future of endodontics look like?
I would say that the impact of COVID will shape the future of endodontics. Many people delayed dental care during the pandemic, and now that they’re coming back into our practice, we’re seeing more complex cases and bigger problems. We’re seeing a phenomenal number of cases with cracked teeth, for example. Patients are stressed and anxious. All of this can be harder to manage and more challenging to treat.
We need to adapt to this new reality by staying calm, reassuring patients, and having empathy. We should also be taking advantage of all the technological advancements available to us — such as the OP 3D CBCT system from DEXIS — to support better diagnosis, treatment, and patient outcomes for these complex cases. When we have more confidence in our work, patients have more confidence in us.
Read more about CBCT imaging in Dr. West’s article on the effect of 3D scans on endodontic decision-making here: https://endopracticeus.com/cbct-3d-imaging-the-next-endodontic-frontier-of-the-great-endodontist/
Stay Relevant With Endodontic Practice US
Join our email list for CE courses and webinars, articles and more..

