Dr. Randy W. Garland discusses a technique to thoroughly debride and disinfect complex anatomy
Abstract
Thorough debridement and disinfection are essential for long-term endodontic success. Molars are more likely to have complex and uncommon canal configurations, accessory canals, and isthmi, which increase the likelihood of missing anatomy during the root canal treatment. This case report details a 57-year-old male smoker that presented with moderate pain in the upper right quadrant. Based upon clinical and radiographic findings, a diagnosis of pulpal necrosis with symptomatic apical periodontitis was made for the right maxillary second molar. Preoperative cone beam computed tomographic images indicated fusion of the mesiobuccal and palatal roots. A complex isthmus between a mesiobuccal and palatal canal that would not be accessible by standard methods was also visualized. Although calcification was present throughout all canals, minimal instrumentation to an apical diameter of size No. 20 was completed. Because the mesiobuccal and palatal isthmus was inaccessible with standard methods, the GentleWave® Procedure was used to debride and disinfect the root canal system and allow a path for obturation. Postoperative radiography demonstrated complete obturation throughout the complex root canal system. Radiographs at 9 and 15 months’ follow-up revealed a clinically asymptomatic tooth and a healed periapical lesion at 15 months. In conclusion, this case report demonstrates the ability of the GentleWave Procedure to thoroughly debride and disinfect complex anatomy.
Introduction
Successful long-term root canal treatment requires thorough debridement, disinfection, and obturation of the entire root canal system to eliminate bacteria and prevent reinfection.1-3 A seemingly simple or ordinary case may present with an anomalous root or root canal morphology; such complex internal anatomy and the inability to identify and treat all canals are common reasons for failure of endodontic treatment.4-6 Previous studies on resected roots with failed root canal therapy have linked persistent apical periodontitis with anatomy that was not prepared or filled adequately.7 Thus, thorough knowledge of both root and root canal morphology is needed to ensure optimal outcomes.8
While all types of teeth may have extra roots and/or canals, molars are more likely to have complex and aberrant canal configurations, accessory canals, and isthmi that increase the risk of untreated anatomy following root canal treatment.5 Maxillary second molars were shown to have more variations in root morphology than maxillary first molars.9 Maxillary second molars also have a higher prevalence of fused roots when compared to maxillary first molars and mandibular second molars. The prevalence of fused roots varies by geographic region, ranging from 7.94% in Brazil to 43% in Ireland.10-14 Yang, et al., described five types of root fusion in maxillary molars. Fusion between the mesiobuccal root and palatal root occurred most commonly in maxillary second molars in 18.1% (56 of 309) of the teeth studied.13 Other studies have reported the frequency of this type of fusion to be approximately 6%-8%.10,13,15-17
Not only do fused roots have wide variability in the number and type of canals, they also may contain isthmi or additional canals that connect some or all of the roots. This anatomy creates a challenge for cleaning and shaping, which may increase the failure rate of root canal therapy. The percentage of isthmi seen in fused roots ranges from 9% to 43%, depending on the type of root fusion. For the mesiobuccal-palatal root fusion, isthmi were seen up to 40% of the time in these teeth.7 Small isthmi have been shown to be inaccessible to standard hand and rotary instrumentation and may even be too thin to be radiographically evident.18-19 Thus, it is likely that proper recognition and treatment of isthmi will reduce the failure rate of some endodontic procedures.
The following case report depicts the successful endodontic treatment of a maxillary second molar with fused mesio-buccal and palatal roots with an isthmus connecting the two canals using a novel endodontic device.
Materials and methods
A 57-year-old male presented with moderate pain in the upper right quadrant. Review of the patient’s clinical history indicated that he was a current smoker. After clinical examination, the right maxillary second molar (tooth No. 2) elicited a mild pain response to percussion. The tooth did not respond to vitality testing with Endo-Ice® (Coltene/Whaledent, Cuyahoga Falls, Ohio). After periodontal probing, an abnormal distolingual periodontal pocket depth was measured at 7 mm. A perceptible mobility <1 mm in the buccolingual direction was documented (Class I mobility). No soft tissue lesions were noted, but preoperative radiographs and intraoral examination with tactile exploration revealed a Class II furcation involvement. Radiographic examination showed tooth No. 2 with a periapical radiolucency (Figure 1). Based upon the clinical and radiographic findings, a periradicular diagnosis of symptomatic apical periodontitis with necrotic pulp was made.i Pre-operative cone beam computed tomography (CBCT) indicated fusion of the mesiobuccal and palatal roots with a possible isthmus connecting a mesiobuccal and palatal canal (data not shown). It was determined that this complex intercanal anatomy would be difficult to access by standard endodontic methods. Therefore, the GentleWave® Procedure (Sonendo® Inc., Laguna Hills, California) which uses advanced fluid dynamics, acoustics, and tissue dissolution chemistry was employed to simultaneously debride and disinfect the entire root canal system.20-21,34 The treatment plan was reviewed with the patient, who agreed and consented to receiving the GentleWave Procedure.
The patient received local anesthesia per standard techniques, and a dental dam was applied to isolate the tooth for endodontic treatment. A conservative straight-line access was prepared, including removal of all pulp horns, overhangs, and ledges. Three distinct canals were noted: the mesiobuccal, distobuccal, and palatal. No isthmi were visible in the pulp chamber. Each of the three canals exhibited calcification throughout its length. A minimally invasive endodontic protocol was utilized that included the use of K-type hand files and rotary file instrumentation to an apical diameter of size No. 20. The isthmus between the fused mesiobuccal and palatal roots could not be accessed with instrumentation, so the GentleWave Procedure was used to debride and disinfect the area. Canals were dried with absorbent paper points and then obturated using a warm vertical compaction technique with gutta-percha and AH Plus® sealer (Dentsply Sirona, York, Pennsylvania). The pulp chamber floor was sealed with flowable glass ionomer.
There was no patient discomfort during or after the procedure, and the procedure was completed without complication. A postoperative radiograph was obtained, revealing complete obturation of the root canal system with obturation material evident throughout the mesiobuccal-palatal complex anatomy (Figures 1B and Figure 2).
The patient returned for follow-up 4, 9, and 15 months postoperatively. No pain or discomfort was reported by the patient at any of the follow-up timepoints. Clinical assessment revealed improvement with normal responses to percussion and mobility testing. Upon periodontal assessment, furcation involvement was noted to improve to Class I, and mobility was restored after 4 months. The patient continued to exhibit general periodontal issues and had only minor improvement of the abnormal pocket depth to 6 mm at 15 months; however, the treated tooth had healed within normal limits and was clinically asymptomatic (Figures 1 and 2).

Figure 1: Periapical radiographs of the second maxillary molar (tooth No. 2) 1A. Preoperative. 1B. Postoperative. 1C. 9 months. 1D. 15 month recall. Healing of the periapical lesion is evident at 15 months
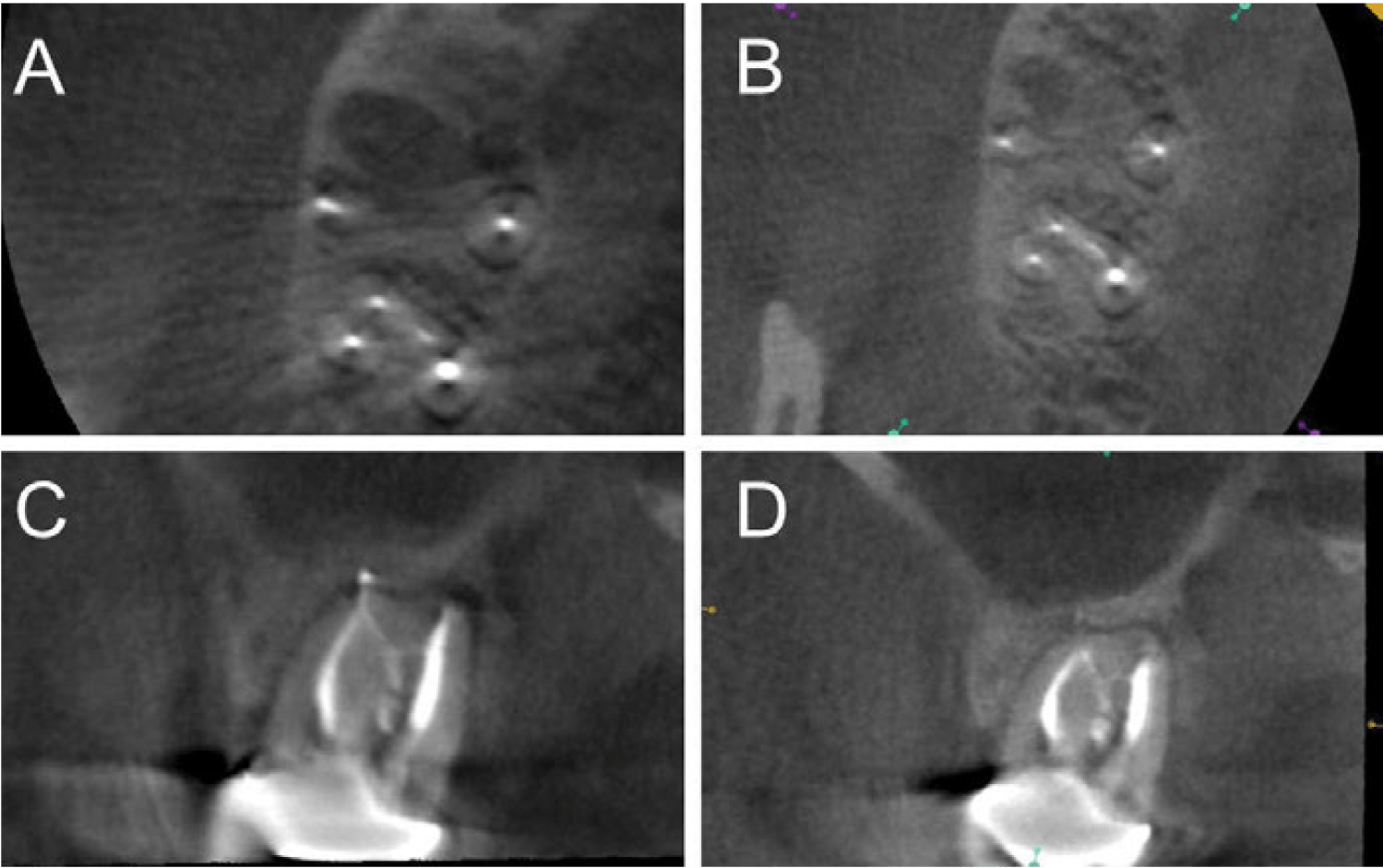
Figure 2: CBCT images of the second maxillary molar (tooth No. 2). 2A, 2C are postoperative and 2B, 2D are at the 15-month recall. Cross-sectional slices detailing the isthmus are seen in the upper panel of each image. In the bottom panels, the isthmus is seen as a thin line connecting the palatal and mesiobuccal roots
Results and discussion
Even with the advent of improved imaging such as CBCT, limitations of current instrumentation, including the inability to access canals or isthmi, may result in inadequate debridement and disinfection of the entire root canal system in such complex anatomy. In fact, the frequency and risk of missed anatomy are strongly linked to the complexity of the root canal system.5,18 Such difficulties may lead to eventual failure, necessitating retreatment.22 In a study of 493 teeth with failed root canal treatments, missed canals and anatomical complexity were the cause of 19.7% and 8.7% of failed cases, respectively.23 A prospective in vivo study by Hoen and Pink demonstrated that 42% of 1,100 endodontically treated teeth that were failing had an untreated canal space, while 85% had periradicular radiolucencies.24
While maxillary molars are the second-most frequently treated group of teeth endodontically, they are also the most complex.4 Maxillary second molars are even more challenging as they have been shown to have more variation in the number of roots, canals, and 4 times greater prevalence of root fusion than maxillary first molars.10,15-16,25 An ex vivo study by Ordinola-Zapata, et al., examined 100 maxillary second molars with fused roots and found that mesiobuccal-palatal fusion, similar to the current case report, occurred in 15% of the fused teeth studied.7 Isthmi were seen 40% of the time in mesiobuccal-palatal fused teeth, thus making this type of maxillary second molar challenging to treat.
Cleaning of the isthmus can thus be quite difficult and problematic. Whereas wider isthmi are more readily accessible to instruments and irrigants, small isthmi are often inaccessible to standard hand and rotary instrumentation.18 Complications such as strip perforations are possible if too large of a file is used.19 Despite continuous irrigation during and after rotary instrumentation, up to 35.2% of the isthmus volume can be filled with apparent hard dentin debris, which can prevent adequate debridement and obturation.26 Debris removal is much more difficult in a small isthmus versus an instrumented canal.
Several studies have examined the debridement efficacy of hand/rotary instrumentation and ultrasonics in small isthmi. One study compared the manual hand file/rotary instrumentation cleaning and shaping technique with or without the addition of ultrasonic irrigation. Isthmus cleanliness values were significantly different between the two groups, with 33% cleanliness observed with the use of hand/rotary instrumentation. The addition of ultrasonic irrigation improved the cleanliness value to 83%.27 Similar results were noted by Gutarts, et al., where isthmus cleanliness ranged from 15%-38% for hand/rotary instrumentation compared to 73%-96% with the addition of ultrasonic activation.18 Another study demonstrated that continuous ultrasonic irrigation removed significantly more debris in non-instrumented isthmi than side-vented needle irrigation (87.53%-99.93% versus 52.14%-99.32%).28 Susin, et al., compared manual dynamic irrigation and apical negative pressure techniques in mandibular molars with narrow isthmi. Neither technique completely removed debris from isthmi, though considerably less debris was found in the apical negative pressure group.29 However, none of these approaches completely cleaned the isthmi. Since microorganisms have been shown to exist for more than a decade in extremely harsh and nutrient-deficient environments such as an isthmus area, the need for alternate approaches to enhance cleaning and disinfection are needed.30
The GentleWave Procedure is designed to enhance cleaning and disinfection throughout the entire root canal system using Multisonic Ultracleaning.20-21 The system is comprised of a console and a sterile, single-use GentleWave Procedure Instrument, which delivers distilled water, sodium hypocholorite, and ethylenediaminetetraacetic acid (EDTA) throughout the entire root canal system using advanced fluid dynamics, tissue dissolution chemistry, and acoustic technology to debride and disinfect the entire root canal system, even areas untouched or undetected by standard techniques.20-21,31 As detailed by Haapasalo, et al., the GentleWave Procedure provides 7 times faster tissue dissolution than standard root canal therapy devices, including ultrasonic-based irrigation devices, and creates negative pressure at the apex as compared to the positive apical pressure generated by syringe irrigation devices.32-33 When the cleaning efficiency of the GentleWave Procedure was compared with a passive ultrasonic system and standard needle irrigation configuration, the GentleWave Procedure was the only technique that removed all calcium hydroxide from mesial and distal canals of 30 mandibular molars, even in the apical third.31 Similar conclusions were drawn by Molina, et al., in 45 freshly extracted molars when root canal debridement of the GentleWave Procedure was compared to standard rotary instrumentation with needle irrigation; cleaning effectiveness was 97.2% versus 67.8%, respectively, for the mesial canals.21 As healing is a focus in this case report, a long-term, prospective, multicenter clinical study of 75 molars treated with the GentleWave Procedure showed a 97% healing rate at 12 months with 96.2% of patients being free from severe and moderate posttreatment pain in the first 2 postoperative days and no incidence of pain reported by day 14.34
Calcification was also noted in all three canals; excessive calcification can impede successful navigation of the canals and may even reduce long-term success for teeth with pre-existing apical disease.23 The probability of long-term endodontic success was further complicated since the patient was a smoker. Smoking has been shown to impair the body’s response to infection, which could delay periapical healing and promote a higher incidence of apical periodontitis in smokers.35-36 Smokers are also ~1.7 times more likely to require root canal treatment.37 The fact that the periapical lesion shows extensive healing for the maxillary second molar in this patient over the 15 month follow-up period, despite the patient’s generalized periodontal issues and lifestyle choices, indicates that the GentleWave Procedure was able to debride and disinfect the root canal system, including the isthmus, sufficiently to eradicate the periradicular infection and allow obturation materials to enter the space.
Clinical implications
- Complex anatomy may be difficult to clean or inaccessible using standard instru-mentation techniques.
- The GentleWave Procedure was able to clean and disinfect complex anatomy that was otherwise inaccessible; the 15-month recall indicated the patient was clinically and radiographically healing.
- This technique may be a useful approach to clean and disinfect challenging cases involving complex anatomy, which may improve patient outcomes.
Conclusion
Some patients often have complex anatomy that is not easily accessible by standard endodontic methods. It is well-known that endodontic therapy cannot succeed without adequate debridement and disinfection and that untreated canals are a major cause of endodontic failure. The GentleWave Procedure was able to debride and disinfect the entire root canal system in a difficult case with complex and inaccessible anatomy. This report demonstrates that the GentleWave Procedure may be a useful approach for treating teeth with complex anatomy.
- Ford MW. Complex Apical Anatomy Revealed Following Endodontic Treatment of a Maxillary Molar Using the GentleWave System: A Case Report. Dentistry. 2017;7:446.
- Holderrieth S, Gernhardt C. Maxillary molars with morphologic variations of the palatal root canals: a report of four cases. J Endod. 2009;35(7):1060-1065.
- Siqueira J Jr, Rôças IN. Clinical implications and microbiology of bacterial persistence after treatment procedures. J Endod. 2008;34(11):1291-1301.
- Nosrat A, Verma P, Hicks ML, Schneider SC, Behnia A, Azim A. Variations of Palatal Canal Morphology in Maxillary Molars: A Case Series and Literature Review. J Endod. 2017;43(11):1888-1896.
- Cantatore G, Berutti E, Castellucci A. Missed Anatomy: frequency and clinical impact. Endod Topics. 2009;15(1):3-31.
- Vertucci F. Root canal morphology and its relationship to endodontic procedures. Endod Topics. 2005;10(1):3-29.
- Ordinola-Zapata R, Martins JNR, Bramante CM, Villas-Boas MH, Duarte MH, Versiani MA. Morphological evaluation of maxillary second molars with fused roots: a micro-CT study. Int Endod J. 2017;50(12):1192-1200.
- Ahmed H, Abbott P. Accessory roots in maxillary molar teeth: a review and endodontic considerations. Aust Dent J. 2012;57(2):123-131.
- Kim Y, Lee SJ, Woo J. Morphology of maxillary first and second molars analyzed by cone-beam computed tomography in a Korean population: variations in the number of roots and canals and the incidence of fusion. J Endod. 2012;38(8):1063-1068.
- Rwenyonyi CM, Kutesa AM, Muwazi LM, Buwembo W. Root and canal morphology of maxillary first and second permanent molar teeth in a Ugandan population. Int Endod J. 2007;40(9):679-683.
- Neelakantan P, Subbarao C, Ahuja R, Subbarao C, Gutmann J. Cone-beam computed tomography study of root and canal morphology of maxillary first and second molars in an Indian population. J Endod. 2010;36(10):1622-1627.
- Silva EJ, Najaim Y, Silva AI, Haiter-Neto F, Zaia AA, Cohenca N. Evaluation of root canal configuration of maxillary molars in a Brazilian population using cone-beam computed tomographic imaging: an in vivo study. J Endod. 2014;40(2):173-176.
- Yang ZP, Yang SF, Lee G. The root and root canal anatomy of maxillary molars in a Chinese population. Endod Dent Traumatol. 1988;4(5):215-218.
- Al Shalabi R. Omer O, Gle Yang Z-P, Yang S-F, Lee G. The root and root canal anatomy of maxillary molars in a Chinese Population. Endod Dent Traumatol. 1988;4:215-218.
- Martins J, Mata A, Marques D, Carames J. Prevalence of Root Fusions and Main Root Canal Merging in Human Upper and Lower Molars: A Cone-beam Computed Tomography In Vivo Study. J Endod. 2016;42(16):900-908.
- Tian X, Yang X, Qian L, Wei B, Gong Y. Analysis of the Root and Canal Morphologies in Maxillary First and Second Molars in a Chinese Population Using Cone-beam Computed Tomography. J Endod. 2016;42(5):696-701
- Ghobashy A, Nagy MM, Bayoumi AA. Evaluation of Root and Canal Morphology of Maxillary Permanent Molars in an Egyptian Population by Cone-beam Computed Tomography. J Endod. 2017;43(7):1089-1092.
- Gutarts R, Nusstein J, Reader A, Beck M. In vivo debridement efficacy of ultrasonic irrigation following hand-rotary instrumentation in human mandibular molars. J Endod. 2005;31(3):166-170.
- Jafarzadeh H, Wu YN. The C-shaped root canal configuration: a review. J Endod. 2007;33(5):517-523.
- Wohlgemuth P, Cuocolo D, Vandrangi P, Sigurdsson A. Effectiveness of the GentleWave System in Removing Separated Instruments. J Endod. 2015;41(11):1895-1898.
- Molina B, Glickman G, Vandrangi P, Khakpour M. Evaluation of Root Canal Debridement of Human Molars Using the GentleWave System. J Endod. 2015;41(10):1701-1705.
- von Arx T. Frequency and type of canal isthmuses in first molars detected by endoscopic inspection during periradicular surgery. Intl Endod J. 2005;38(3):160-168.
- Song M, Kim H, Lee W, Kim E. Analysis of the cause of failure in nonsurgical endodontic treatment by microscopic inspection during endodontic microsurgery. J Endod. 2011;37(11):1516-1519.
- Hoen MM, Pink FE. Contemporary endodontic retreatments: an analysis based on clinical treatment findings. J Endod. 2002;28(12):834-836.
- Ratanajirasut R, Panichuttra A, Panmekiate S. A Cone-beam Computed Tomography Study of Root and Canal Morphology of Maxillary First and Second Permanent Molars in a Thai Population. J Endod. 2018;44(1):56-61.
- Endal U, Shen Y, Knut A, Gao Y, Haapasalo M. A high-resolution computed tomographic study of changes in root canal isthmus area by instrumentation and root filling. J Endod. 2011;37(2):223-227.
- Burleson A, Nusstein J, Reader A, Beck M. The in vivo evaluation of hand/rotary/ultrasound instrumentation in necrotic, human mandibular molars. J Endod. 2007;33(7):782-787.
- Adcock J, Sidow S, Looney S, et al.. Histologic evaluation of canal and isthmus debridement efficacies of two different irrigant delivery techniques in a closed system. J Endod. 2011;37(4):544-548.
- Susin L, Liu Y, Yoon J, et al. Canal and Isthmus debridement efficacies of two irrigant agitation techniques in a closed system. Intl Endod J. 2010;43(7):1077-1090.
- Fan B, Pan Y, Gao Y, Fang F, Wu Q, Gutmann JL. Three-dimensional morphologic analysis of isthmuses in the mesial roots of mandibular molars. J Endod. 2010;36(11):1866-1869.
- Ma J, Shen Y, Yang Y, et al. In vitro study of calcium hydroxide removal from mandibular molar root canals. J Endod. 2015;41(4):553-558.
- Haapasalo M, Wang Z, Shen Y, Curtis A, Patel P, Khakpour M. Tissue dissolution by a novel multisonic ultracleaning system and sodium hypochlorite. J Endod. 2014;40:1178-1181.
- Haapasalo M, Shen Y, Wang Z, et al. Apical pressure created during irrigation with the GentleWave system compared to conventional syringe irrigation. Clin Oral Investig. 2016;20(7):1525-1534.
- Sigurdsson A, Garland R, Le KT, Woo SM. 12-month Healing Rates after Endodontic Therapy Using the Novel GentleWave System: A Prospective Multicenter Clinical Study. J Endod. 2016;42(7):1040-1048.
- Krall EA, Abreu Sosa C, Garcia C, Nunn ME, Caplan DJ, Garcia RI. Cigarette smoking increases the risk of root canal treatment. J Dent Res. 2006;85(4):313-317.
- Kirkevang LL, Vaeth M, Hörsted-Bindslev P, Bahrami G, Wenzel A. Risk factors for developing apical periodontitis in a general population. Intl Endod J. 2007;40:290-299.
- Ghattas Ayoub C, Aminoshariae A, Bakkar M, et al. Comparison of IL-1β, TNF-α, hBD-2, and hBD-3 Expression in the Dental Pulp of Smokers Versus Nonsmokers. J Endod. 2017;43(12):2009-2013
Stay Relevant With Endodontic Practice US
Join our email list for CE courses and webinars, articles and more..

 Randy W. Garland, DDS, received his Bachelor’s degree in Biology from San Diego State University. He then attended University of Southern California where he earned a Doctorate of Dental Surgery (DDS) in 1988. After practicing general dentistry for 7 years, he decided to go back to school to specialize in endodontics. He was accepted into the postdoctoral residency program at Loma Linda University where he received a Certificate in Endodontics in 1997. Since that time, he has operated a private practice in Encinitas, California.
Randy W. Garland, DDS, received his Bachelor’s degree in Biology from San Diego State University. He then attended University of Southern California where he earned a Doctorate of Dental Surgery (DDS) in 1988. After practicing general dentistry for 7 years, he decided to go back to school to specialize in endodontics. He was accepted into the postdoctoral residency program at Loma Linda University where he received a Certificate in Endodontics in 1997. Since that time, he has operated a private practice in Encinitas, California.