Dr. John West describes how endodontic preparation can set your office up for greater predictability.
Dr. John West explores “The Set Up”
Preparation
When endodontics fails, it often fails before it even begins.
In endodontics, technique isn’t everything. Your endodontic preparation (I call it “The Set Up”) is just as important as technique for becoming a highly skilled endodontic clinician and optimizing your endodontic predictability. The Set Up is, in fact, the start for the successful endodontic thought process of being prepared for that which you are not prepared. In being prepared, there are two distinct areas that require unique skills. Introducing a different terminology, I will call them simply the “Think Box” and the “Play Box.” The intent of this article is to explore the basics of the Think Box (internal and mental) and the Play Box (external and physical). The purpose of the proper Set Up is that it is a prerequisite for enriched endodontic predictability and possibility. In today’s dominant new technology narrative, the endodontic buzzwords have gotten off track. What really matters in creating exceptional endodontic outcomes are “The Fundamentals.”1-3
The context is decisive
The context of today’s endodontic chronicles, education, and marketing is too often focused on a product’s features and benefits being the answer to better endodontic predictability rather than the basics of training and replicating the process of biologic, structural, and esthetic endodontic success. Two often overlooked ingredients for increasing the probability of predictably for successful endodontic outcomes are (1) precisely and intentionally planning for endodontic restorability and (2) starting with the answer. Endodontic success probabilities and tooth retention have the possibility to approach 100%. While success reports may have varied over the past 60 years within a range of 60% to 98%, the rationale and capacity for endodontic success remains at 100%. The rationale of and for predictably successful endodontics has always been that any endodontically diseased tooth can be predictably treated if the root canal system is eliminated (shaped, cleaned, and filled), the periodontal condition is healthy or can be made so, and the tooth is restorable. But everyone knows the real percentage of endodontic success is not 100%. It is 100% minus some number. Let’s call that number X. So, 100 − X. What is the X factor? I have identified 3 X factors: (1) The clinician’s knowledge of what to do, (2) the clinician’s ability to do what is required, and (3) The clinician’s willingness to do so.
Anything can work some of the time. In fact, that same thing might work more often than not. Endodontic predictability mandates something different. What is available to you, the dentist reading this, is for you to transform the expectations and experience of your endodontics. My personal Why for writing this article is to ultimately challenge the reader’s status quo, regardless of how presently predictable you may be with endodontic procedures. “If we keep doing the same thing over and over again expecting different results, we become insane” (Rita Mae Brown). Who wants to be an insane endodontic clinician?
The key takeaway from the heart of this article is for each of us not only to improve our endodontic predictabilities, but also to identify how we want to experience ourselves before treatment, during treatment, and as we reflect back after the treatment. For most of us, the words and phrases used to describe our preferred experiences might include these examples: competent, masterful, in control, I can handle this; I am handling this; I got this; I am agile; I am resilient. You might even ask the ultimate critical question: Would I refer myself to me if I needed endo? Think about that for a second. I suggest you write down your own lists of “How I Want to Experience Myself Doing Endo” and “How Do I Want My Patients to Experience Me When I Am Doing Endo?” This little exercise can be vastly revealing. It may sound trite, but honestly, I feel I have done this exercise many times and discovered I have never really worked a day in my life. Our office is a playground. It is this way of thinking and being that is an essential, yet often missed, critical piece of the Think Box.
When you think about any successful organization or domain such as endodontic predictability, four essential features are always present: (1) vision (intended out-come), (2) structure (a plan to get there), (3) by when (deadline), and (4) measurable milestones along the roadmap (accountability). Endodontic predictability has the same four distinctions, and The Set Up sets this up. Beginning to follow our roadmap is the context for the next successful step. Context is decisive!
The Think Box
The Think Box is our brain, and this is the first essential part of The Set Up. The brain is made up of approximately 100 billion neurons. These nerve cells transmit electrochemical signals in what can be thought of like the gates and wires of a computer. The trick to mastering exceptional endodontic predictability is to harness our neurons to engender the endodontic experience and get the results that we want.
The Olympic Gold Medal Mind is a perfect example. The gold medal is always on the Olympian’s mind. For example, when a female swimmer sets her sights on the Olympic gold medal, she visualizes herself on the Olympic podium receiving the gold medal around her neck with her country’s flag being raised, her anthem playing and tears of joy, and accomplishment streaming down her face. A little dramatic for endodontics? Well, let’s look a little deeper into this intentional imagery process and how it affects endodontic predictability.
We all already do subconscious imagery in everything we do, whether we know it or not. It is the automatic pilot — the autonomic system working as its best. The trick is learning to recognize the made-up stories in our minds about the endodontic patient cases in front of us (bringing them into our consciousness) and then intentionally seeing the stories or outcomes that we want in our minds. Presto — magic! The outcomes we want and see become real. When this happens, we have applied our minds to produce intended outcomes. Now all we have to do is practice this until the practice itself, e.g., for the Olympic gold medalist, becomes second nature. Keep in mind that the vast majority of people have no idea that they are creating memories of the future (and their future goals) all the time. The trick is to intentionally fashion or guide the future desired memory into the present time. How do we do this using the concept of endodontic predictability as a perfect starting point? It’s time to take action! Once you decide that improving your endodontic predictability truly matters to you, you, like everyone else, will have your own penchants to unlearn. How can we remember to remember to nurture our newfound skills in order to immediately implement them in our practice of endodontics? The trick! Too often, dentists sabotage their intended successes by failure to take a few moments before, and frequently during treatment, to intentionally see, feel, and think (SFT) the desired endodontic outcomes: vividly seeing themselves overcoming what may first be perceived as obstacles, challenges, or temporary setbacks and instead producing perfect results with absolute imperturbability — feeling the desired outcomes in their guts and then thinking, “I am enough. I am able” (briandesroches.com). Sometimes endodontic mistakes occur because the mental set up in The Think Box — namely, the pretreatment imaging of the posttreatment result — is insufficient or has not been practiced enough or at all (Figure 1).
In order to understand the role of the brain in producing replicable endodontic predictability, a brief review about understanding how the brain works can be the difference that makes the difference.
Three essential brain facts
- Hebb’s axiom
“Neurons that fire together, wire together.”4 This clever phrase was first used in 1949 by Donald Hebb, a Canadian neuropsychologist known for his work in the field of associative learning. When a group of nerve cells are stimulated (fire together), a potential “neural network” of information and energy is formed (wired together). Firings happen with an emotion as the catalyst. Hebb’s axiom reminds us that every experience, thought, feeling, and physical sensation triggers millions of neurons, which form a neural network. When you repeat an experience over and over, the brain learns to trigger the same neurons each time: endodontic predictability.
- Attention density
Neural networks are created when nerve cells are fired enough for them to “wire” together. “Enough” is a function of focus, frequency, and intensity. Attention density is concerned with thoughts and emotions that accompany any action or intended result. If my thoughts about outcomes are embedded in a positive or negative state, and if I keep focusing on those thoughts and/or emotions, I will create a dense neural network with positive or negative contents (i.e., a memory). Along with love, this is perhaps our most powerful gift as humans: choice. Neuroscience and quantum physics research tell us if you focus long enough, hard enough, and often enough, you can change your neural pathways and brain circuitry to rewire your brain. Attention density is how we make learning stick: endodontic predictability.
- Neuroplasticity
The brain can change, and we are the actual changers.5,6 You can change your brain by changing what you are focusing on. By managing my focus and using my mind to direct my focus on the outcomes and experiences I want, I can change my brain and strengthen the wiring of the SFT networks: the desired memories of the future brought into the present time, the now: endodontic predictability.
The endodontic practice-changing magic of SFT
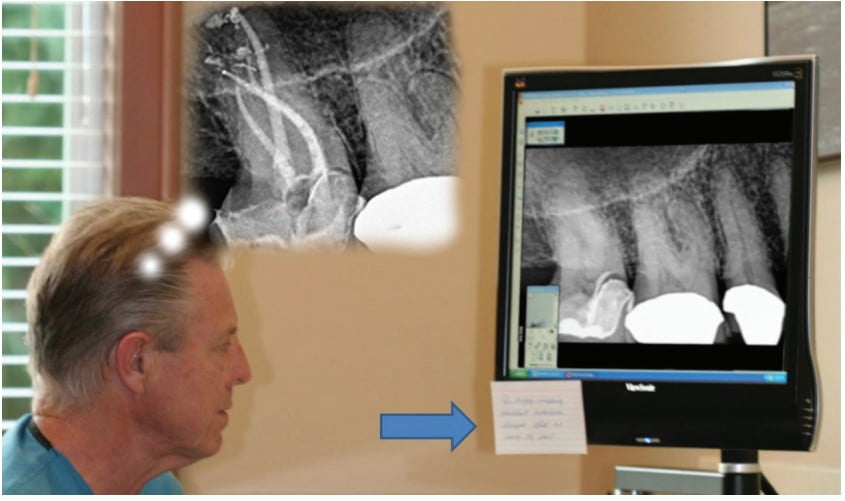
How does the endodontic clinician apply the above three basic brain facts, as mysterious and complicated as they are, to produce purposeful endodontic outcomes? The secret is SFT. The “see” part of SFT is the external-outcome component that is embedded within the neural network. The content of the SFT way of creating new neural networks are that it first enables us to first see what the root canal system is through multiview radiographs and ask: Is there a chamber? Where are the canals? How many canals are there? What are their sizes and shapes? Take a 3D CBCT scan to better see the anatomy, and/or take a bitewing and perpendicular, mesial, and distal periapical images (Figure 2). SFT is not hope, visualization, affirmation, positive thinking, kumbaya, or an endodontic cult. It is seeing (visualizing) the desired endodontic outcome as the point of focus or the North Star principles that guide you during the procedure.

The “see” and “feel” have been wired into us since the beginning evolution of the survival of the fittest. Changing our neural networks does not happen overnight. Change requires attention density. The SFT skill has been used since our birth, and the good news is that we can harness this skill to produce our desired endodontic future now — right now — when treating your patient’s endodontic root canal system!
The “feel” part of SFT is how I am experiencing myself doing the procedure and that I am “seeing” what I want in the theater of my mind: my mind’s eye; for example, “I am present, focused, and confident during my endo procedures, and I trust my skills and experience.” Hold this feeling for 10 seconds to fire and wire your new neurons. Do this every chance you get. The SFT practice will fire and wire your neurons to create the network of endodontic predictability. The principle of attention density reminds us that the more frequently we focus on the desired neural network for 10 seconds at a time, the stronger and more sustainable the wiring becomes.
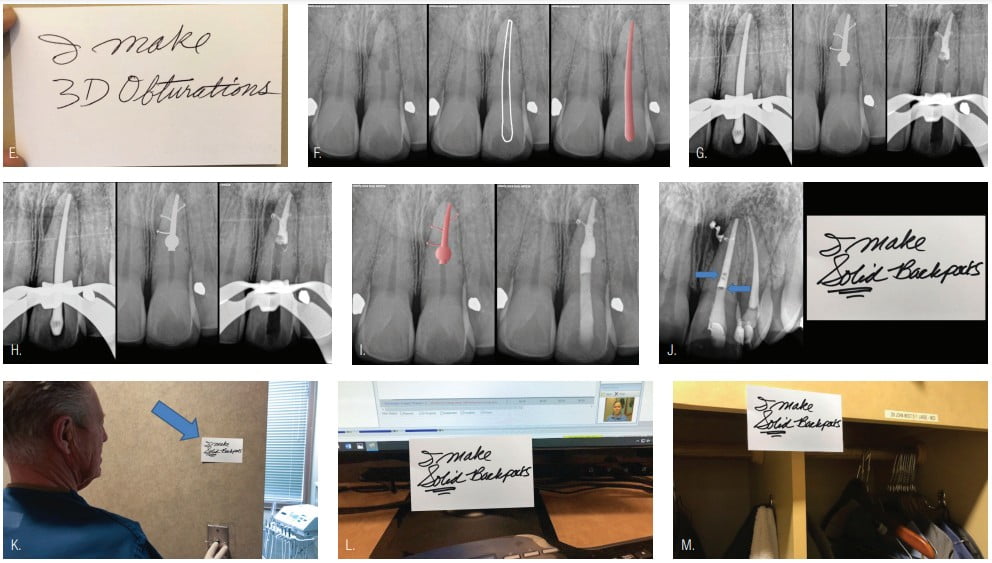
The “think” part of SFT is the moment of realization when we give ourselves permission to believe that we are enough, even more than enough, to do the job. To think finds its origin from the Old English, referring to “causing to appear to one’s self; to conceive in the mind.” We are worthy of the endodontic accomplishment before us. Endodontic predictability is a state of mind. It is a state of thinking. It is a state of being. And we can evoke it on demand (Figure 3).
Application to an endodontic procedure
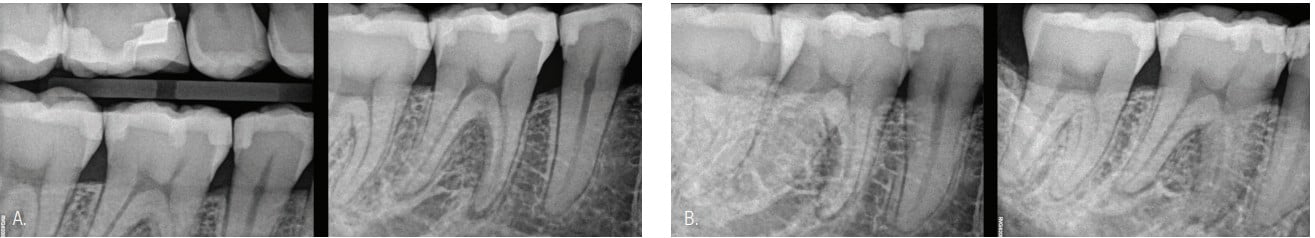
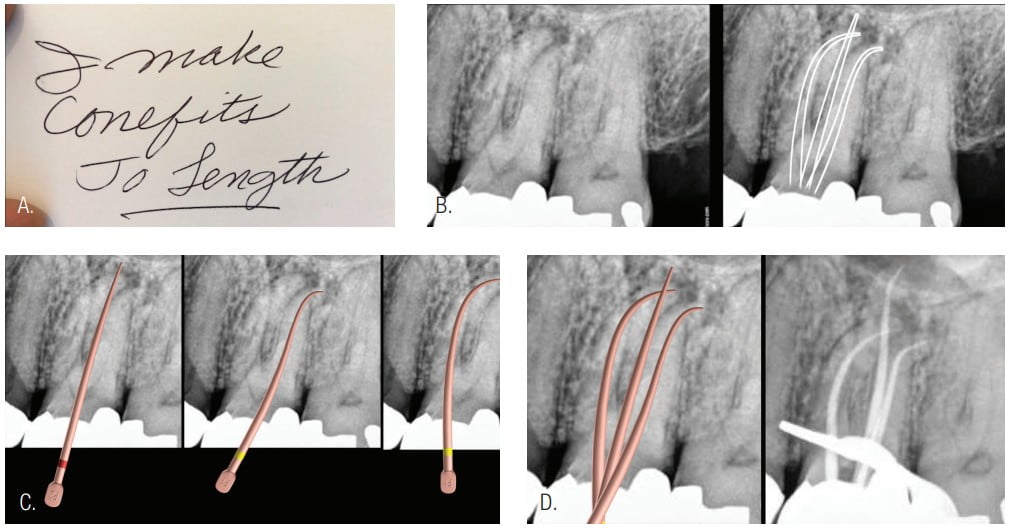
Here’s my 3” x 5” index card trick. Back to how do we “remember to remember?” It is so easy to go out of the moment and listen instead to that constant voice in one’s head that is all about the past or future. This is the practiced skill difference that makes the difference. The index cards are placed in prominent locations where they cannot be avoided before, during, or after the endodontic treatment. The best way to train our neurons for what we want is to write what we want — for example, “I make conefits to length”— on an index card (Figure 4). While the external conditions of the endodontic challenge will vary from patient to patient, creating endodontic predictability through exceptional endodontic outcomes is the same. This is the SFT Gold Medal Mind. This “thinking” invites us to think differently: for example, “There are no problems in endodontics, only situations requiring smart thinking.”
The Play Box
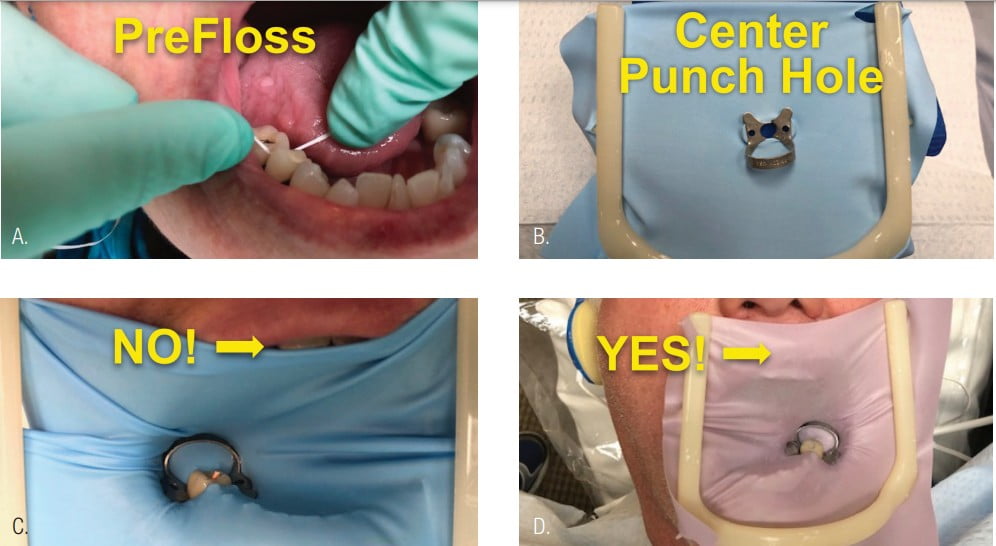
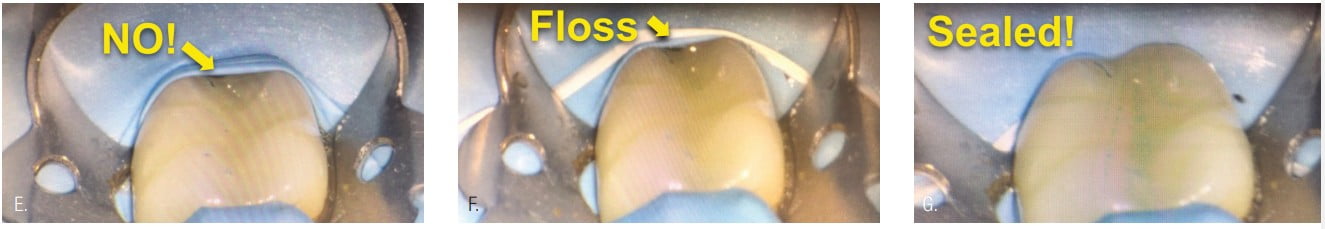
The Play Box is the physical component of The Set Up that is often overlooked or underperformed. In short, the three parts of the Play Box are (1) a rubber dam, (2) rubber dam clamps, and (3) an access bur selection. The importance of this 1, 2, 3 checklist can be underestimated. While every dentist reading this article has a different operatory design and infrastructure delivery system, there should be a consistent protocol for simple rubber dam placement, clamp choice, and bur selection.

Rubber dam clamps: You only need two: 2A for posterior teeth and 9A for anterior teeth. They should be almost universal, but they are not (Figure 5)!
Rubber dam: The name of the game with the rubber dam is security! The rubber dam should be punched so that the tooth punch hole is in near the center of the rubber dam, allowing equal access from all angles. The rubber dam prevents the unintended swallowing of an instrument, such as a manual file. The rubber dam also thoroughly seals the tooth from saliva leaking into the access and root canal system irrigants from leaking under the rubber dam and into the mouth. Rubber dam quality seems almost too basic to write about, but if proper attention is not given here, then our 1, 2, 3 Play Box checklist for endodontic predictability is already in jeopardy (Figure 6).
Burs: Everyone has a favorite bur. In my practice, I have identified nine of my favorite burs and their uses. If I include long shank burs, which are often needed, you can double the number of burs that I use! My point is that most dentists cutting an access cavity adapt to the bur. For more control, consider instead adapting to the access and using the bur that is needed. While some dentists may choose only one or two burs due to price sensitivity or perceived efficiency, I do not use all nine every time (Figure 7). The “less is more” concept applies here. The key part of the Play Box physical Set Up is a new bur. New-bur efficiency can be the subject of an entire article, but for now, here is a simple test to prove new bur versus used bur. I call this the new-bur challenge.

For your next 10 endodontic accesses, use your favorite burs, but use new ones. After each of the first 10 patients, clean and sterilize each bur used, and then place them in a cup labeled “Used Burs.” When patient No. 11’s endodontic tooth is treated, use the burs from the “Used Burs” cup. Observe the difficulty of access with the used burs compared to the previous new-bur experience. Notice the loss of confidence. Dull burs show up when it is too late. It might not be the second time but maybe the third or fourth time. You never know exactly when; dullness is gradual and insidious. You now have to invest your time to first discover the dull bur, then you waste your time taking the bur out of the handpiece and placing a new bur into the handpiece and then returning to where you were in the procedure after having been distracted for perhaps up to a minute. Time is the most important factor in your overhead. Now honestly, as dentistry is crawling out of the world’s pandemic shock, efficiency may not be your current priority, but someday that will change back to normal with the desire to be as efficient as possible.
The next step of the Play Box is designing a “maximally appropriate” access, followed by maintaining your mental game all the way to the treatment finish line: endodontic predictability.7
Closing comments
You now know the “intellectual knowledge” for producing endodontic predictability is “on demand.” You have your 3″ × 5″ remember-to-remember memory cards to provide frequent, significant visual support for experiencing sensory knowledge and for training your new endodontic predictability neural networks. It’s time to take action! Use this information when preparing for your next endodontic treatment and, even more importantly, during your next endodontic treatment.
Remember, we are free to be (present in this nanosecond of a moment) and free to act. Whenever you are stuck — for example, on your way to the apex — rather than do more or less of the same, ask yourself, “What do I need to do differently?” Then, with your goal firmly in your mind, just get out of the way and observe as your hands do their magic!
Along your endodontic treatment journey, you will want to minimize the variables, so always remember that simple is better. It doesn’t mean easy. Stay focused on what is under your control. Learn to manage the variability of endodontics, and keep having fun while realizing and experiencing your full endodontic potential!
This article was reprinted with permission from Dentistry Today.
- West JD. Anatomy matters only when it matters. Endodontic Practice US. 2013;6(5):14-16.
- West JD. Endodontic predictability: “What matters?” Dent Today. 2013;32:108-113.
- Brousseau C. Realize Your Golfing Potential. Sea Script Company; 2017.
- Hebb DO. The Organization of Behavior: A Neuropsychological Theory. John Wiley & Sons: New York; 1949.
- Doidge N. The Brain’s Way of Healing: Remarkable Discoveries and Recoveries from the Frontiers of Neuroplasticity. Viking: New York; 2015.
- Nuwer R. The right stuff: the Olympic edge. Sci Am Mind. 2016.
- West JD. The pendulum swings: “minimally invasive” vs “maximally appropriate.” Dent Today. 2019;38:8-10.
- West JD. The endodontic Glidepath: “secret to rotary safety.” Dent Today. 2010;29:86-93.
- West JD. Manual versus mechanical endodontic Glidepath. Dent Today. 2011;30:136-140.
- West JD. Glidepath implementation: “return to the beginning.” Dent Today. 2011;30:90-97.
Stay Relevant With Endodontic Practice US
Join our email list for CE courses and webinars, articles and more..

 John West, DDS, MSD, received his DDS degree from the University of Washington, where he is an affiliate professor. He is the founder and director of the Center for Endodontics in Tacoma, Washington and a clinical instructor at Boston University, where he earned his MSD degree and was honored with the Distinguished Alumni Award. Dr. West and his two sons, Drs. Jason and Jordan West, are in private endodontic practice in Tacoma. He can be reached via email at johnwest@centerforendodontics.com.
John West, DDS, MSD, received his DDS degree from the University of Washington, where he is an affiliate professor. He is the founder and director of the Center for Endodontics in Tacoma, Washington and a clinical instructor at Boston University, where he earned his MSD degree and was honored with the Distinguished Alumni Award. Dr. West and his two sons, Drs. Jason and Jordan West, are in private endodontic practice in Tacoma. He can be reached via email at johnwest@centerforendodontics.com.