CE Expiration Date:
CEU (Continuing Education Unit): Credit(s)
AGD Code:
Educational aims and objectives
This clinical article aims to:
- Inform the reader of the etiology of dens invaginatus (DI) dental malformation.
- Demonstrate how to treat this condition through case studies.
Expected outcomes
Endodontic Practice US subscribers can answer the CE questions by taking this quiz to earn 2 hours of CE from reading this article. Correctly answering the questions will demonstrate the reader can:
- See a report showing the truthful diagnosis and conservative treatment of dens invaginatus using current endodontic methods.
- Recognize that dens invaginatus can be treated nonsurgically with the aid of the dental operating microscope, ultrasonic, and hand endodontic instruments.
- Recognize some of the reasons that RCT of teeth with DI can be demanding.
- See why a meticulous radiographic inspection plays a key role in the identification of
- Realize the role that canal morphologies, microbes, irregular dimensions of the root canal system, and elimination of the invaginated form of hard tissue play in the challenging treatment of DI.
Drs. Adrian Espinoza Muñoz, Jorge Paredes Vieyra, Fabian Ocampo Acosta, Francisco Javier Jiménez Enriquez, Daniel Cerrillo Lara, and Ceceña Gonzalez Flor Vianey review dens invaginatus in root canals and measure how best to approach the condition
Dens invaginatus (DI) is a growth-related malformation resulting from invagination of the crown before calcification has developed (Hüllsmann, 1997). As the hard tissues are created, the invaginated enamel organ creates a small tooth inside the forthcoming pulp chamber. In the severe type of dens invaginatus, there is a folding of Hertwig’s epithelial sheath into the developing root (Bhaskar, 1986).
The etiology of this dental malformation remains controversial, and although many hypotheses have been proposed, none have been supported or widely accepted. Numerous issues have been suggested to explain this uncommon dental formation, including trauma, infection, inhibition of the growth of specific cells, disruption of factors that regulate the formation of the enamel organ, and links to genetic factors (Hüllsmann, 1997; Alani and Bishop, 2008; Hosey and Bedi, 1996).
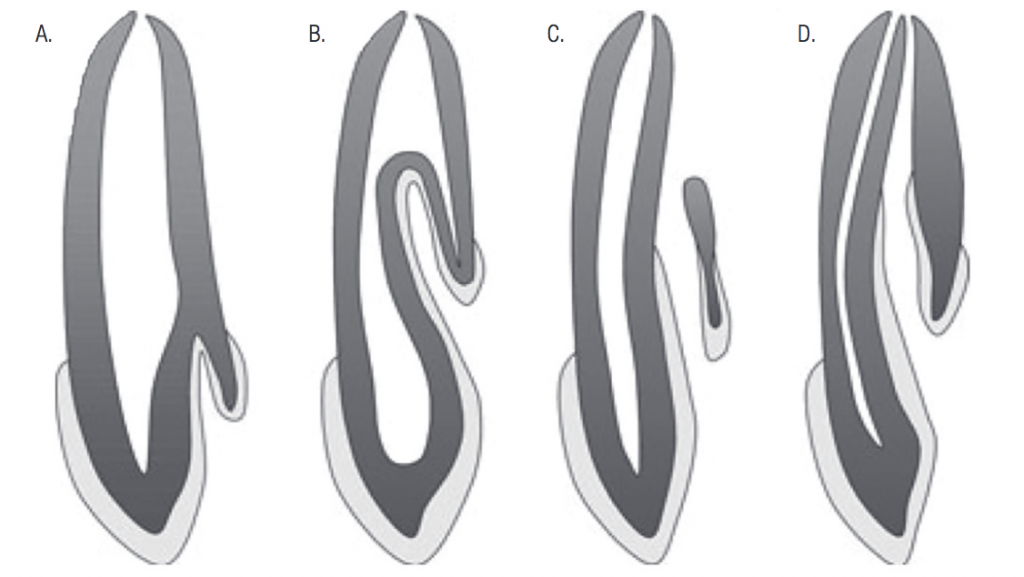
Salter (1855) described a radiographic image that seems to be “a tooth within tooth.” DI can be catalogued according to its complexity, with the well documented classification of Oehlers (1957) describing three forms according to the complexity of the invagination into the root: Type I is limited to the crown, whereas type II invagination extended inside the root, ending as a blind pod. Type III invagination invades the entire root and exits apically or laterally (Figure 1). Its occurrence varies from 0.3% to 10% (Hovland and Block, 1977), with the upper lateral incisor the most frequently affected tooth followed by the upper central incisor.
Teeth with DI pose a problem for root canal therapy because of their complex anatomy. Numerous clinical procedures have been proposed such as nonsurgical root canal treatment (Hovland and Block, 1977); combined root canal and surgical treatment (Benenati, 1994); planned replantation (Lindner, et al., 1995); and extraction (Rotstein, et al., 1987). However, planned replantation and extraction are often the last decision. Outcome studies for the management of teeth with DI are, however, unavailable due to the rarity of the condition.
The following clinical condition describes the combined orthodontic-endodontic treatment of a maxillary central incisor diagnosed with infected dens invaginatus (Oehlers’ type III) and associated apical periodontitis. A surgical operating microscope was used as an aid for both diagnosis and the planning of treatment.
Case report
An 11-year-old female patient presented at the Orthodontic Graduate School in Tijuana, México, with a complaint of pain and tenderness in the maxillary left anterior area. The principal condition was the unerupted left maxillary central incisor (UL1). The child was healthy and had no record of disease. The patient had a normal facial pattern, with a Class I skeletal relationship. Intraoral inspection exposed acceptable oral hygiene and early mixed dentition with a dental Class II correlation on the left side only (Figures 2A, 2B, and 2C).



The partial eruption of UL1 followed in an insufficient space distribution with midline deviance. The tooth had belated root maturity related with its homologue. After initial examination, the patient was referred to the endodontic department for consultation and further management. The patient reported mild pain and swelling about a week before, but at the day of examination, there were no clinical manifestations.
Diagnosis and treatment planning
Orthodontic view
Clinical examination revealed an 11-year-old female requiring orthodontic therapy due to uncompleted eruption and a lack of normal alignment in the maxillary left central incisor (Figures 3A, 3B, and 3C).
Endodontic diagnosis
Clinical inspection showed immature crown eruption on the maxillary left central incisor UL1. There was no sign of sinus tract; nonetheless, the tooth was vaguely tender to tapping. The labial mucosa related to the maxillary left central incisor was sore. UL1 was non-responsive to cold stimulation (Endo-Ice®; Coltene), while the adjacent teeth responded normally. Periodontal examining was within standard limits.
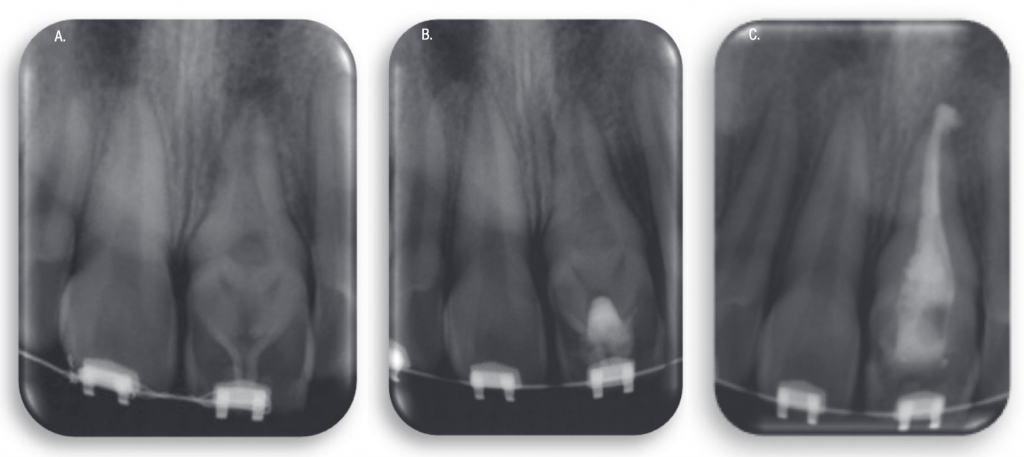
Radiographic inspection showed immature root development, apical radiolucency of about 4 mm in diameter, and an abnormal internal structure corresponding with Class III DI.
A diagnosis of pulp necrosis with apical periodontitis was made. The contralateral central incisor was also tested for clinical and radiographic signs of the same malformation, but there were none.
The patient’s general dentist had suggested antibiotics (amoxicillin 250 mg, 3 times a day for 7 days) and an analgesic (ibuprofen 400 mg, 3 times a day for 7 days).
Treatment procedure
Orthodontic treatment






Figures 3A-3F: The nonsurgical treatment images 3A to 3F. 3A. Labial aspect of UL1 with dens invaginatus; 3B. Lateral view of UL1; 3C, 3D, 3E. Partial eruption of UL1 followed in an insuf-ficient space distribution with midline deviance; 3F. Complete orthodontic treatment
Early management used an asymmetrical Klöehn-type headgear to repair the left side Class II and obtain some area. Concurrently, brackets (Edgewise, 0.022 0.025-inch slot; Monrovia, California, Glendora California) were positioned on teeth UR2 UR1 UL2, and a 3 x 2 segmented alignment with open coil spring (Ormco™, Glendora, California) was performed to redistribute space in the arch, with special emphasis to the left central incisor region. Orthodontic movement was programmed (Figures 3D, 3E, and 3F).
Orthodontic movement started 10 days later. The aim was to take the tooth into the appropriate position by an adjustment in its eruption direction. Biomechanical control was achieved with the help of trans-palatal arch. An extrusion force of approximately 50 gm–60 gm was applied using an elastic band (1/8 inch) attached with the alignment wire.
As the tooth moved downwards, a mandibular occlusal splint was suggested to diminish occlusal contact, allowing for the succeeding alignment of the tooth with a complete orthodontic appliance.
Nonsurgical endodontic treatment
A clinical strategy was developed that included nonsurgical root canal treatment (RCT) of the dens tract over some appointments, comprising use of a calcium hydroxide dressing. The treatment plan was presented to and accepted by her parents, and the plan was to perform removal of the DI and the infected necrotic pulp tissue, followed by the complete RCT. Written consent was obtained before initiation of RCT and notably addressed all the available treatment options and their associated risks, benefits, and challenges (Figures 4A, 4B, and 4C).


Figures 4A-4F
A surgical operating microscope (Carl Zeiss Surgical) was used in all the treatment. After anesthesia with 2% lidocaine, 1: 100,000 epinephrine (Xylocaine, Dentsply Sirona), rubber dam was placed and stabilized with dental dam cord (Wedjets®, Coltene). Access was prepared with a 331-carbide bur in the lingual side of the tooth. Entrance into the large pulp chamber of the invagination via an occlusal access revealed a necrotic pulp tissue.
The infected pulp tissue was removed, and the irregular invaginated tissue was cautiously eliminated by chemomechanical preparation using ultrasonic endodontic tips sizes 2-4 (ProUltra® Endo Coated instrument; Dentsply Sirona) at power setting four of the ultrasonic unit (Acteon Satelec P5; Dentsply Sirona) in a brushing movement starting from an apical to coronal direction.
The root canal was prepared primarily with a long-tapered diamond bur to improve access to the apical defect. Working length of the dens tract was estimated with an apex locator (Root ZX, QED UK, JMorita USA) and was verified radiographically. The root canal was initially debrided with large K-file instruments up to size 60. The master apical size of 110 was achieved using K-files (Sybron-Endo, Kerr Endodontics). The remaining root canal was molded as far as possible with Gates Glidden drills (Dentsply Sirona) size 2-4.
To maximize proper disinfection, irrigation was performed with 5.25% sodium hypochlorite (NaOCl) in the pulp chamber and 2.5% NaOCl the apical part of the canal system with the regard to the incomplete apical closure of the root. Some 2ml of 17% EDTA was used to remove the smear layer. The final irrigation of the canal with NaOCl was achieved using the Piezon Master 400 ultrasonic unit (EMS, Optident UK). Sodium hypochlorite was delivered into the canal by syringe, and ultrasonic passive irrigation was performed for one minute.
The root canal was desiccated with sterile absorbent paper cones size No. 100, and dressed with Ca(OH)2 paste (PULPDENT™ Corp, Watertown, Massachusetts). The entrance of pulp chamber was temporarily sealed with Cavit® (3M Oral Care) and Fuji IX (GC UK) to avoid infection of root canal system. The patient returned after 2 weeks, having remained free of any symptoms. At this second appointment, the tooth was not sensitive to percussion, and the soft tissues in the area were not tender to palpation. The tooth was anesthetized as earlier defined, and rubber dam was placed. The invagination was opened and flooded with 1% NaOCl followed by a final rinse with 17% EDTA for 1 minute and passive ultrasonic irrigation (ProUltra® tips 1 and 2; Dentsply Sirona) with 1% sodium hypochlorite for 1 minute after elimination of calcium hydroxide paste.
After additional irrigation, the canal was desiccated with sterile absorbent paper cones, and further Ca(OH)2 was placed in the canal. The tooth was temporarily sealed with Cavit and Fuji IX as previously described. The patient was requested to return 3 weeks later for completion of nonsurgical RCT.
At the third visit, the tooth was anesthetized as described before and isolated with a rubber dam. The tooth was accessed, Ca(OH)2 was eliminated from the root canal with passive ultrasonic irrigation, and the canal was desiccated with sterile absorbent paper cones size No. 100.
The prepared root canal was filled with a master apical gutta percha cone size No. 110 and warm gutta percha using an Obtura® Gun (Obtura II, Fenton, Missouri) and AH 26 sealer (Dentsply Sirona). A bolus of thermoplasticized injectable gutta percha heated to 150ºF was delivered and carefully positioned around the master apical gutta percha with use of Schilder pluggers size No. 10 (Dentsply Sirona). Serial radiographs were exposed to visualize and check its acceptable adaptation, and to take the absence of extrusion outside the apical foramen (Figures 3D, 3E, and 3F). The root canal system was then filled with thermoplasticized gutta percha warmed to 150º F.
The access was filled with a light-cured composite, and a control radiograph was taken. The patient was advised to take 400 mg ibuprofen (every 6 hours as needed for pain); antibiotics were not deemed necessary because of the absence of signs/symptoms. The patient was then referred to the attending dentist. The patient was asked to return in 48 hours and was seen at 1-month, 3-month (Figure 3E), 6-month, and 1-year recall periods. Cone beam technology was used to see completed filling (Figures 3F and 3G).
Discussion
RCT of teeth with DI can be demanding because of the capricious form of the internal anatomy and the fact that the dens tract is covered with enamel (Hüllsmann, 1997). Additionally, pulp necrosis in such teeth usually develops before complete apical closure, leaving the root canal with a wide apical opening.
Opportune diagnosis and proper treatment of such cases (orthodontic-endodontic treatment) can help to prevent physiological, esthetic and functional problems associated with DI.
The clinical protocol includes an effective treatment plan based on the knowledge of signs, symptoms, and radiographs. A meticulous radiographic inspection plays a key role in the identification of DI. Nevertheless, standard or digital periapical radiographs may not show the features and size of the invagination (Vier-Pelisser, et al., 2012). CBCT imaging has been shown to be useful in the diagnosis of teeth with unusual anatomy. The introduction of cone beam computed tomography (CBCT) brought about a revolution in dentistry that has contributed to the planning, diagnosis, therapy, and prognosis of several dental procedures (Kaneko, et al., 2011).
Teeth with DI present physical defects that are predisposed to caries because of the deep pits that act as locations of plaque retention. Microbes and their products may exacerbate infection and lead to necrosis of the pulp, frequently before final maturation of the root (Cingiz, 2006). Therefore, DI requires early diagnosis and treatment. A major condition for effective RCT is the entire elimination of irritants from the infected root canal system.
A tooth with DI shows a diversity of canal morphologies such as concavities, intracanal communications, apical difficulties, and other areas that mechanical devices cannot reach. The complicated structure in DI affects the prognosis of the tooth. The case of DI presented here demonstrates one clinical handling approach, which may not necessarily be appropriate in all such clinical scenarios.
The irregular dimensions of the root canal system make proper shaping and cleaning complicated. A large amount of dentin has to be removed to ensure adequate cleaning. Regrettably, this may end in increased predisposition to fracture the thin root-end walls.
Elimination of the invaginated form of hard tissue in the root canal is tough and challenging. Thus, the clinician should select a suitable way to eliminate the hard tissue, the necrotic material, and the microorganisms. In this case, the use of an operating surgical microscope and ultrasonic instruments facilitated the clinical procedures. In some clinical situations, the abnormal structure of DI is internal and an independent unit from the rest of the tooth. In these occurrences, the complete elimination of the central-anomalous structure and total elimination of pulp tissue can be followed with this valuable clinical aid.
An ideal endodontic repair material should seal the paths of interaction between the root canal and its neighboring tissues. It should be harmless, non-carcinogenic, bio-tolerable, insoluble in tissue fluids, and physically stable (Bogen and Kuttler, 2009). Calcium hydroxide as interappointment treatment, ultrasonic instrumentation, and passive irrigation are necessary and suggested (Bishop and Alani, 2008). Obturation techniques using thermoplasticized injection of gutta percha are correct for such teeth because they allow flow of softened gutta percha into unreachable areas better than other techniques, but they have a risk of extrusion in teeth with an open apex (de Sousa and Bramante,1998).
Several methods have been proposed to strengthen the root (Katebzadeh, et al., 1998; Lertchirakarn, et al., 2002). Materials like MTA can be considered an option in RCT of immature permanent teeth with DI with the benefit of shorter treatment time, good sealing ability, and great biocompatibility (Kumar, et al., 2014).
The procedural difficulty encountered is controlling the overfill or under fill of MTA. Most of these include bonding a material to the root dentin inside the root canals. However, it has been shown that such a bond can break down over time (Kitasako, 2002). Hence, long-term decrease of fracture exposure employing bonding techniques must be debatable. In this case, the dentin wall seemed to be sufficiently thick, so fracture was not a primary concern (Brooks and Ribera, 2014; Narayana, et al., 2012; Zoya, et al., 2015; Zhang and Wei, 2017).
Conclusions
This report shows the correct diagnosis and conservative treatment of dens invaginatus using current endodontic methods. This case report demonstrates that Class III dens invaginatus can be treated nonsurgically with the aid of the dental operating microscope, ultrasonic, and hand endodontic instruments.
Acknowledgments
The authors thank Professor Michael Hülsmann for his valuable assistance in reviewing this manuscript.
References
- Alani A, Bishop K. Dens invaginatus: part 1: classification, prevalence and aetiology. Int Endod J. 2008;41(2):1123-1136.
- Benenati FW. Complex treatment of a maxillary lateral incisor with dens invaginatus and associated aberrant morphology. J Endod. 1994;20(4):180-182.
- Bhaskar SN. Synopsis of Oral Pathology. 7th ed. CV Mosby: St. Louis, MO; 1986.
- Bishop K, Alani A. Dens invaginatus. Part 2: clinical, radiographic features and management options. Int Endod J. 2008;41(12):1137-1154.
- Bogen G, Kuttler S. Mineral trioxide aggregate obturation: a review and case series. J Endod. 2009;35(6):777-790.
- Brooks JK, Ribera MJ. Successful nonsurgical endodontic outcome of a severely affected permanent maxillary canine with dens invaginatus Oehlers type 3. J Endod. 2014;40(10):1702-1707.
- Cengiz SB, Korasli D, Ziraman F, Orhan K. Non-surgical root canal treatment of dens invaginatus: reports of three cases. Int Dent J. 2006;56(1):17-21.
- de Sousa SM, Bramante CM. Dens invaginatus: treatment choices. Endod Dent Traumatol. 1998;14(4):152-158.
- Hosey MT, Bedi R. Multiple dens invaginatus in two brothers. Endod Dent Traumatol. 1996;12(1):44-47.
- Hüllsmann M. Dens invaginatus: aetiology, classification, prevalence, diagnosis, and treatment considerations. Int Endod J. 1997;30(2):79-90.
- Hovland EJ, Block RM. Nonrecognition and subsequent endodontic treatment of dens invaginatus. J Endod. 1977;3:360-362.
- Lindner C, Messer HH, Tyas MJ. A complex treatment of dens invaginatus. Endod Dent Traumatol. 1995;11(3):153-155.
- Katebzadeh N, Dalton BC, Trope M. Strengthening immature teeth during and after apexification. J Endod. 1998;24(4):256-259.
- Kaneko T, Sakaue H, Okiji T, Suda H. Clinical management of dens invaginatus in a maxillary lateral incisor with the aid of cone-beam computed tomography: a case report. Dent Traumatol. 2011;27(6):478-483.
- Kitasako Y, Burrow MF, Nikaido T, Tagami J. Long-term tensile bond durability of two different 4-META containing resin cements to dentin. Dent Mater. 2002;18(3):276-280.
- Kumar A, Yadav A, Shetty N. One-step apexification using platelet rich fibrin matrix and mineral trioxide aggregate apical barrier. Indian J Dent Res. 2014;25(6):809-812.
- Lertchirakarn V, Timyam A, Messer HH. Effects of root canal sealers on vertical root fracture resistance of endodontically treated teeth. J Endod. 2002;28(3):217-219.
- Narayana P, Hartwell Wallace R, Nair UP. Endodontic Clinical Management of a Dens Invaginatus Case by Using a Unique Treatment Approach: A Case Report. J Endod. 2012;38(6):1145-1148.
- Oehlers FA Dens invaginatus (dilated composite odontome). I. Variations of the invagination process and associated anterior crown forms. Oral Surg Oral Med Oral Pathol. 1957;10(11):1204-1218.
- Rotstein I, Stabholz A, Heling I, Friedman S. Clinical considerations in the treatment of dens invaginatus. Dent Traumatol. 1987;3:249-254.
- Salter S. Warty tooth. Trans Pathol Soc Lond. 1855;6:173-177.
- Vier-Pelisser FV, Pelisser A, Recuero LC, et al. Use of cone beam computed tomography in the diagnosis, planning and follow up of a type III dens invaginatus case. Int Endod J. 2012;45(2):198-208.
- Mandibular Central Incisor with a Periapical Lesion: A Case Report. J Endod. 8:1378-1382.<unrevised>
- Zhang P, Wei X. Combined Therapy for a Rare Case of Type III Dens Invaginatus in a Mandibular Central Incisor with a Periapical Lesion: A Case Report. J Endod. 2017;43(8):1378-1382.
- Zoya A, Ali S, Alam S, et al. Double Dens Invaginatus with Multiple Canals in a Maxillary Central Incisor: Retreatment and Managing Complications. Int Endod J. 2015;14(11):1927-1932.
Stay Relevant With Endodontic Practice US
Join our email list for CE courses and webinars, articles and more..


