CE Expiration Date:
CEU (Continuing Education Unit): Credit(s)
AGD Code:
Educational aims and objectives
This clinical article aims to discuss microsurgical management for correction of a procedure
error in the phase of apical mechanical preparation in endodontics.
Expected outcomes
Endodontic Practice US subscribers can answer the CE questions to earn 2 hours of CE from reading this article. Click here for the quiz. Correctly answering the questions will demonstrate the reader can:
- Realize the importance of cleaning and disinfection of the root canal system.
- Recognize the importance of the role of the mechanical preparation of the root canal system.
- Realize some risks of transportation of the foramen.
- Identify the three categories of transportation of the foramen.
Dr. Leandro A.P. Pereira discusses treatment for one of the most common errors in endodontic treatment
Endodontics is the specialty that treats or prevents pulpal pathologies and apical periodontitis. The main objectives of endodontic treatment are to clean and disinfect the entire length of the root canal system up to a healthy level (Siqueira, et al., 2000). When such objectives are achieved through meticulous treatment, success rates can exceed 94% (Imura, et al., 2007; Lazarski, et al., 2001). Seeking these results during endodontic therapy, the mechanical preparation is carried out with endodontic instruments and chemical preparation with irrigating solutions.
The mechanical preparation of the root canal system is of utmost importance in the process of endodontic disinfection (Al-Sudani, Al-Shahrani, 2006). It is responsible for physically removing the infected dentin and, consequently, bacteria located within the dentinal tubules. In addition, it increases the diameter of the main canals, allowing the delivery of a larger volume of irrigating solutions into the apical third (Shuping, et al., 1999; Siqueira, et al., 2000). It also creates a favorable conical shape for endodontic filling. Therefore, it directly influences the quality of the disinfection process and, consequently, the prognosis of the case. Improper cleaning of canals, especially the apical third, predisposes endodontic failures (Sjogren, et al., 1990; Nair, et al., 1990).
Procedural errors during the mechanical preparation phase may make it impossible to reach the required disinfection levels. Yousuf, et al., 2015, made a digital radiographic evaluation of 1,748 endodontically treated teeth and found procedural errors in 32.8% (574 teeth) of them. Transportation of the apical foramen, which may or may not lead to root perforations, is among the most common errors committed during endodontic treatment, especially in curved canals (Fogarty, Montgomery, 1991; Camara, et al., 2007; Gergi, et al., 2010).
According to the Glossary of Endodontic Terms of the American Association of Endodontics, canal transportation is defined as “Removal of canal wall structure on the outside curve in the apical half of the canal due to the tendency of files to restore themselves to their original shape during canal preparation; may lead to ledge formation and possible perforation.”
The inadvertent use of rigid endodontic files, especially of larger calibers, without previous and meticulous analysis of the individual internal dental anatomy, increases the risk of transposition of the foramen.
Transportation of the foramen may impair the disinfection of the canal system by disabling access to its original trajectory, as well as irritating the periapical tissues by extruding bacteria and their byproducts, and derailing the ideal apical adjustment of a gutta-percha cone. These technical disabilities, imposed by operational error in the cleaning and shaping phase, can negatively influence apical sealing and appropriate bacterial control (Wu, et al., 2002). As a result, they worsen the prognosis of the clinical case involved.
According to Gluskin, et al., 2008, transportation of the foramen can be classified into the following three categories:
- Type I represents a minor movement of the physiologic position of the foramen.
- Type II represents a moderate movement of the physiologic position of the foramen, resulting in a considerable iatrogenic relocation on the external root surface. In this type, a larger communication with the periapical space exists.
- Type III represents a severe movement of the physiologic position of the foramen and the canal, resulting in a significant iatrogenic relocation.
Treatment of apical transportation cases can be made by different clinical approaches. Canals with Type I transposition transportation can usually be cleaned and filled; with Type II may be filled after the application of an apical barrier to control bleeding and to serve as a physical shield to prevent extrusion of the endodontic filling material. In these situations, placing an apical plug of MTA followed by conventional endodontic filling can also be considered.
However, in clinical cases with apical transportation of Type III, it is generally not possible to achieve the desirable cleaning, disinfection, and proper filling. A first attempt should be tried in order to get in to the original trajectory of the root canal. Thus, these steps should be performed as best as possible followed by an apical microsurgery to remove the untreated apical region.
 Clinical case
Clinical case
A female patient, 55 years old, named ASA I, visited the dental office complaining of spontaneous, constant pain, exacerbated while chewing and apical palpation in the region of teeth Nos. 13 and 11 that had been endodontically treated 3 months before. Her measured blood pressure was 128 x 78 mmHg, heart rate 82 bpm, oxygen saturation of 98%, and body temperature of 38.5ºC.
The patient reported that she did not feel pain before the start of the initial endodontic treatments, and they were indicated for oral rehabilitation reasons. After the first endodontic session by another dentist, where teeth Nos. 13 and 11 were treated at the same time, the pain began and exacerbated after the third day. On the fourth day, the patient had to receive intravenous dipyrone and ketoprofen to control the pain. Concurrently to the systemic medication, an occlusal adjustment was performed. After 2 days, the pain returned, and the patient went to another dentist who prescribed dipyrone 500 mg/ml every 4 hours and Nimesulide 100 mg every 12 hours orally for 7 days. The pain decreased but did not cease. Two days after the end of the use of systemic medication, the patient again felt pain. She then went to a third professional who initiated the endodontic reintervention of teeth Nos. 11 and 13. However, the therapy that was being performed was not able to effectively control pain. After 4 days, the patient also began presenting febrile conditions. It was reported that the rubber dam not was used in any of the previously endodontic procedures performed.
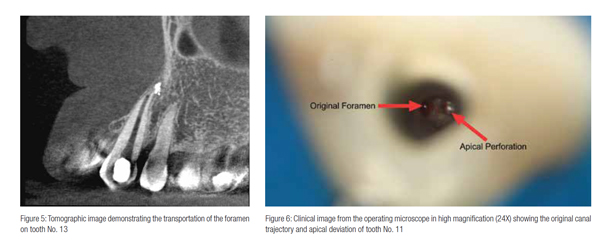
Clinical examination revealed endodontic access on teeth Nos. 13 and 11. Inadequate geometric configuration of endodontic access already suggested problems in chemical-mechanical preparation steps of the root canal system (Figures 1 and 2). Endodontic therapy started in teeth Nos. 13 and 11, and transportation of the foramen Type III was radiographically observed. On tooth No. 12, there were a full crown, metallic post, and an inadequate previously initiated endodontic therapy (Figure 3). Apical periodontitis was diagnosed on teeth Nos. 13, 12, and 11. On the CBCT, it was possible to highlight the transposition of the foramen on tooth No. 11 (Figure 4) and tooth No. 13 (Figure 5).
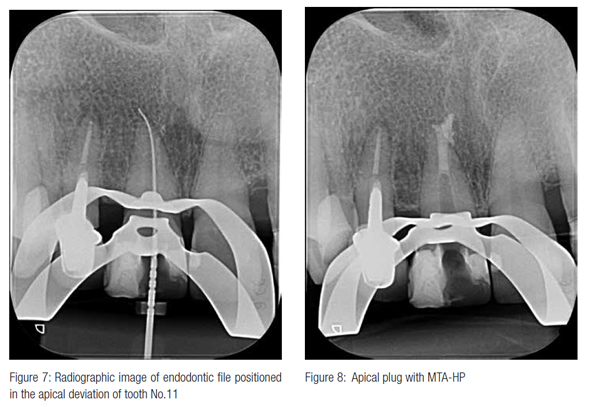
Despite the severity of the apical deviation on teeth Nos. 13 and 11, the first clinical attempt was carry out trying to reach the original root canal pathways. The therapy was initiated with the endodontic retreatment of tooth No. 11 followed by tooth No. 13. The canals were irrigated with sodium hypo-
chlorite 2.5% followed by 17% EDTA, both with PUI and prepared with Reciproc® 50 (VDW®; Munich, Germany). Through the operating microscope and periapical X-rays, it was possible to visualize the apical deviation of tooth No. 11; however, it was not possible to reach the original trajectory of the main root canal (Figures 6 and 7). The same occurred with tooth No. 13. Due to the great irregularity of the root canal walls after the transposition of the foramen, it was not possible to perform the proper fit of gutta-percha master cone. For this reason, the decision was to perform an apical plug of 4 mm with MTA-HP (Angelus®, Londrina, Brazil) (Figure 8). The filling of the rest of the canals was performed using thermoplasticized gutta percha with Fillapex MTA cement. Fillapex MTA cement contains particles of MTA in its composition.
However, this approach was not effective. The proper disinfection control had not been achieved. Due to that, the spontaneous pain, although decreasing, had not ceased. In this way, an additional treatment was required to achieve the desired disinfection. The recommended complementary treatment was the endodontic microsurgery.
In addition, tooth No. 12 also needed a endodontic retreatment due to the apical periodontitis and insufficient previous endodontic treatment. However, as the prosthetic crown of this element was adapted, and microsurgery was already planned for the neighboring teeth, the decision was to perform a retrograde endodontic treatment on tooth No. 12.

 After the conventional endodontic retreatment, the patient underwent apical microsurgery, where the apical area corresponding to the apical iatrogenic region was removed with Piezoelectric ultrasonic tip (W1, CVDentus®; Brazil). A Piezoelectric apicoectomy was performed on tooth No. 12 with the same ultrasonic tip. The canal was retro-prepared to the depth corresponding to the apex of the metal post present. After drying the canal with a Endo Tip 0.014” (Angelus; Londrina, Brazil) coupled to a vacuum pump, the procedure continued with the retro-filling using MTA-HP (Angelus; Londrina, Brazil) (Figures 9-11).
After the conventional endodontic retreatment, the patient underwent apical microsurgery, where the apical area corresponding to the apical iatrogenic region was removed with Piezoelectric ultrasonic tip (W1, CVDentus®; Brazil). A Piezoelectric apicoectomy was performed on tooth No. 12 with the same ultrasonic tip. The canal was retro-prepared to the depth corresponding to the apex of the metal post present. After drying the canal with a Endo Tip 0.014” (Angelus; Londrina, Brazil) coupled to a vacuum pump, the procedure continued with the retro-filling using MTA-HP (Angelus; Londrina, Brazil) (Figures 9-11).
 MTA has been the material of choice for sealing perforations, retrograde preparations, and apices with irregular morphology (not circular). Its superior features of marginal adaptation, biocompatibility, sealing ability in wet environments, induction, and conduction of hard tissue formation, cementogenesis with consequent formation of normal periodontal adhesion, make it the most suitable material for these clinical situations. MTA-HP is also available in powder and liquid form. It preserves all the features of traditional MTA with the addition of easier clinical handling. This characteristic of improved clinical handling is due to a change in the particle size of the MTA powder and the addition of a plasticizer to the liquid.
MTA has been the material of choice for sealing perforations, retrograde preparations, and apices with irregular morphology (not circular). Its superior features of marginal adaptation, biocompatibility, sealing ability in wet environments, induction, and conduction of hard tissue formation, cementogenesis with consequent formation of normal periodontal adhesion, make it the most suitable material for these clinical situations. MTA-HP is also available in powder and liquid form. It preserves all the features of traditional MTA with the addition of easier clinical handling. This characteristic of improved clinical handling is due to a change in the particle size of the MTA powder and the addition of a plasticizer to the liquid.
After 5 months of microsurgery, the patient returned for clinical radiographic control. Clinically, she no longer had any complaints of pain or discomfort. Radiographically, rapid repair of the apical periodontitis was observed in the three teeth involved (Figure 12).
Conclusion
The mechanical chemical preparation phase of the root canal system is of utmost importance for the success of endodontic therapy. Operational errors at this stage, including transportation of the foramen, can dramatically compromise the prognosis of the case. Therefore, it is extremely important to prevent them.
However, depending on the severity of the error, it can be repaired. Postoperative radiographic and clinical control of this clinical case shows that microsurgical complementation can be a safe and predictable clinical option.
References
- Imura N, Pinheiro ET, Gomes BP, Zaia AA, Ferraz CC, Souza-Filho FJ. The outcome of endodontic treatment: a retrospective study of 2000 cases performed by a specialist. J Endod. 2007;33(11):1278–1282.
- Lazarski MP, Walker WA, Flores CM, Schindler WG, Hargreaves KM. Epidemiological evaluation of the outcomes of non-surgical root canal treatment in a large cohort of insured dental patients. J Endod. 2001;27(12):791–796,
- Al-Sudani D, Al-Shahrani S. A comparison of the canal centering ability of ProFile, K3, and RaCe Nickel Titanium rotary systems. J Endod. 2006;32(12):1198-1201.
- Fogarty TJ, Montgomery S. Effect of preflaring on canal transportation: Evaluation of ultrasonic, sonic, and conventional techniques. Oral Surg Oral Med Oral Pathol. 1991; 72(3):345-50.
- Camara AC, Aguiar CM, Poli de Figueiredo JA. Assessment of the deviation after biomechanical preparation of the coronal, middle, and apical thirds of root canals instrumented with three HERO rotary systems. J Endod. 2007;33(12):1460-1463.
- Gergi R, Rjeily JA, Sader J, Naaman A. Comparison of canal transportation and centering ability of twisted files, Pathfile-ProTaper system, and stainless steel hand K-files by using computed tomography. J Endod. 2010;36(5):904-907.
- Shuping GB, Orstavik D, Sigurdsson A, Trope M. Reduction of intracanal bacteria using nickel-titanium rotary instrumentation and various medications. J Endod. 2000;26(12):751–755.
- Siqueira JF, Lima KC, Magalhães FA, Lopes H, de Uzeda M. Mechanical reduction of the bacterial population in the root canal by three instrumentation techniques. J Endod. 1999;25(5):332–335.
- Sjogren U, Hagglund B, Sundqvist G, Wing K. Factors affecting the long-term results of endodontic treatment. J Endod. 1990;16(10):498-504.
- Nair PN, Sjӧgren U, Krey G, Kahnberg KE, Sundqvist E. Intraradicular bacteria and fungi in root-filled, asymptomatic human teeth with therapy-resistant periapical lesions: a long-term light and electron microscopic follow-up study. J Endod. 1990;16(12):580-588.
- Wu M, Fan B, Wesselink PR. Leakage along apical root fillings in curved root canals. Part I: effects of apical transportation on seal of root fillings. J Endod. 2000;26(4):210-216.
- Gluskin AH, Peters CI, Wong RD Ming, Ruddle CJ. Retreatment of non-healing endodontic therapy and management of mishaps. In: Bakland LK, Baumga
Stay Relevant With Endodontic Practice US
Join our email list for CE courses and webinars, articles and more..


 Clinical case
Clinical case
