CE Expiration Date:
CEU (Continuing Education Unit): Credit(s)
AGD Code:
Educational aims and objectives
This clinical article aims to discuss the repair of furcal iatrogenic perforation with mineral trioxide aggregate, including a 4-year follow-up
Expected outcomes
Endodontic Practice US subscribers can answer the CE questions to earn 2 hours of CE from reading this article. Take the quiz by clicking here. Correctly answering the questions will demonstrate the reader can:
- Realize the successful endodontic treatment of furcal iatrogenic perforation with reparative materials such as mineral trioxide aggregate.
- Visualize the concept through viewing the case report.
- Realize some properties of MTA and its benefits.
- Realize a possible cause of furcal perforation.
Dr. Claudio Peru presents a case study on the repair of furcal iatrogenic perforation with mineral trioxide aggregate with a 4-year follow-up
Mineral trioxide aggregate (MTA) has been frequently used as material of choice for perforation repair, pulp capping, and apexification since its introduction in 1993 (Lee, Monsef, Torabinejad, 1993; Osorio, et al., 1998; Torabinejad, et al., 1995).
MTA is a mineral powder that consists of hydrophilic particles, which comprises principle components of tricalcium silicate, tricalcium aluminate, tricalcium oxide, and other mineral oxides. It has a pH of 12.5 and sets in the presence of moisture in approximately 4 hours (Torabinejad, Pitt Ford, 1996; Torabinejad, Chivian, 1999). The repair capacity of MTA can be attributed to the antimicrobial properties and high pH (12.5) of MTA. These characteristics of MTA promote growth of the cementum and formation of bone (Roberts, et al., 2008).
Furcal perforation is usually an undesired complication that can occur during preparation of endodontic access cavities or exploring canal orifices of multirooted teeth (Bargholz, 2005). These undesirable situations, such as excess removal of tooth structure or perforation, occur during attempts to locate canals or as a direct result of failing to achieve straight line access to the canals (Frank, 2002; Unal, Maden, Isidan, 2010).
The aim of this long-term follow-up case report is to present a successful treatment of iatrogenic furcal perforation by MTA.
Case Report
A healthy 60-year-old man attended Chiswell Green Specialist Centre for evaluation of his upper right first molar (UR6). He reported having a recent root canal treatment carried out by his general dental practitioner. Since the time the work was completed, he was experiencing “an intense burning sensation in the gums around that tooth.”
Our examination found UR6 sensitive to palpation and tender to percussion. This tooth was restored with a composite filling. The mean probing pocket depth was within normal level. The radiographic examination showed a large extrusion of gutta percha through a perforation in the pulp chamber.
Various treatment options were discussed with the patient. The patient wished to retain his natural tooth and decided to opt to have the UR6 re-root canal treated while accepting its guarded prognosis. A written informed consent was obtained before commencing the treatment.

Figure 1: Preoperative radiograph of UR6 showing a large extrusion of gutta percha (GP) through a perforation in the pulp chamber
Radiographic examination of UR6 revealed an extrusion of gutta percha through a perforation in the pulp chamber and a large periapical radiolucency (Figure 1).
The tooth was anesthetized (4% articaine hydrochloride containing 1:100,000 epinephrine) and isolated with rubber dam. The endodontic treatment was performed using an operative microscope (Global Surgical Corporation).
The restorative material was removed, and a large perforation was detected clinically on the floor of the pulp chamber. It was noticed that only the mesial canal was obturated, and two GP cones extruded through a perforation created on the floor of the pulp chamber (Figure 3). The hemorrhage was controlled with copious irrigation with 2.2% sodium hypochlorite. The extruded GP was carefully removed (Figure 4). The perforation on the floor of the pulp chamber was disinfected using 2.2% sodium hypochlorite and repaired using MTA (Figures 5 and 6). A layer of glass ionomer cement (GC Fuji IX, GC America) was used to seal the pulp chamber (Figure 7).

Figure 2: Preoperative photograph of UR6

Figure 3: Mesiobuccal canal obturated and two GP cones extruded through a perforation on the floor of the pulp chamber

Figure 4: The extruded GP was carefully removed
Four root canals were cleaned using 2.2% sodium hypochlorite and shaped using ProTaper® (Dentsply) (Figure 8). The root canal system was medicated using calcium hydroxide (Figure 9), and the access cavity was temporarily filled with glass ionomer cement (GC Fuji IX, GC America) (Figure 10).

Figure 5: The perforation on the floor of the pulp chamber was disinfected using 2.2% sodium hypochlorite.

Figure 8: Four root canals were cleaned using sodium hypochlorite 2.2% and shaped using ProTaper Universal

Figure 6: The perforation was repaired using mineral trioxide aggregate (MTA)

Figure 9: The root canal system was medicated using calcium hydroxide

Figure 7: A layer of glass ionomer cement (GC Fuji IX) was used to seal the pulp chamber

Figure 10: The access cavity was temporarily filled with glass ionomer cement (GC Fuji IX)
During the second appointment a week later, the root canals were obturated using the warm vertical condensation technique with System B™ (SybronEndo), Obtura™ II (Obtura Spartan) and AH Plus® sealer (Dentsply Maillefer) (Figure 11). The access cavity was permanently restored using composite resin (Figure 12). A composite core was prepared (Figure 13), and the tooth was restored with a temporary crown (Figure 14). The tooth was finally restored with a permanent crown by the patient’s general dental practitioner. At the 3-month recall, the tooth remained asymptomatic (Figure 15). The patient was discharged to the care of his general dentist who was asked to inform us of any signs of symptoms of periapical pathology associated with this tooth.

Figure 11: Second visit — the root canals were filled using the warm vertical condensation technique (System B, Obtura 2, and AH sealer)

Figure 14: Postoperative radiograph
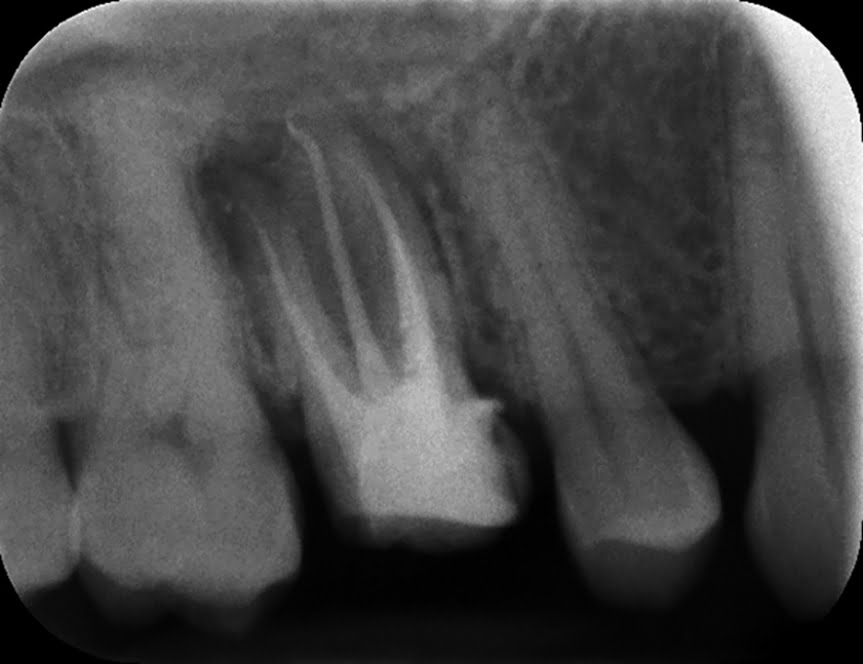
Figure 12: The access cavity was restored using composite resin

Figure 15: Three-month review appointment — tooth restored with a permanent crown following completion of endodontic therapy

Figure 13: A composite core was prepared, and the tooth was restored with a temporary crown

Figure 16: Four-year review
The patient returned to our specialist center 4 years later for the endodontic treatment of another tooth. A re-assessment of UR6 was then carried out. Radiographic examination confirmed periapical healing and the patient was completely asymptomatic (Figures 16 and 17).

Figure 17: Four-year review
Conclusion
It is almost always the patient’s wish to retain his/her natural tooth. In this particular case, all the treatment options were thoroughly evaluated and discussed with the patient before commencing the treatment. The patient fully understood that the prognosis of this tooth was guarded but still decided to try to save his natural tooth.
The developments in the form of reparative materials (MTA), as well the use of the operative microscope, can enhance the positive outcome and promote greater success in endodontic cases that are considered to have a poor prognosis.
References
- Bargholz C. Perforation repair with mineral trioxide aggregate: a modified matrix concept. Int Endod J. 2005;38(1):59-69.
- Frank RJ. Endodontic mishaps: Their detection, correction, and prevention. In: Ingle JI, Bakland LK,
eds. Endodontics. 5th ed. London: BC Decker Inc.; 2002. - Lee SJ, Monsef M, Torabinejad M. Sealing ability of a mineral trioxide aggregate for repair of lateral root perforations. J Endod. 1993;19(11):541-544.
- Osorio RM, Hefti A, Vertucci FJ, Shawley AL. Cytotoxicity of endodontic materials. J Endod.
1998;24(2):91-96. - Roberts HW, Toth JM, Berzins DW, Charlton DG. Mineral trioxide aggregate material use in endodontic
treatment: a review of the literature. Dent Mater. 2008;24(2):149-164. - Torabinejad M, Chivian N. Clinical applications of mineral trioxide aggregate. J Endod. 1999;25(3):197-205.
- Torabinejad M, Hong CU, Lee SJ, Monsef M, Pitt Ford TR. Investigation of mineral trioxide aggregate for root-filling in dogs. J Endod. 1995;21(12):603–608.
- Torabinejad M, Pitt Ford TR. Root-end filling materials: a review. Endod Dent Traumatol. 1996;12(4):161-178 .
- Unal GC, Maden M, Isidan T. Repair of furcal iatrogenic perforation with mineral trioxide aggregate: two years follow-up of two cases. Eur J Dent. 2010;4(4):475-481.
Stay Relevant With Endodontic Practice US
Join our email list for CE courses and webinars, articles and more..


