CE Expiration Date:
CEU (Continuing Education Unit): Credit(s)
AGD Code:
Educational aims and objectives
This clinical article aims to discuss the examination, treatment planning, and endodontic management of a maxillary first molar presenting several complicating features.
Expected outcomes
Endodontic Practice US subscribers can answer the CE questions to earn 2 hours of CE from reading this article. Take the quiz by clicking here. Correctly answering the questions will demonstrate the reader can:
- Describe the examination and assessments used in the patient case.
- Recognize the prognosis and treatment plan of the patient case.
- Understand the treatment protocols followed during the patient’s first and second appointments.
- Realize the strategy used to manage the complications in this case and the value of using the literature to overcome challenges and develop clinical skills.
- Realize that the definition of success or failure in a case may not be representative of the dynamic healing process that is occurring.
Dr. Satnam Singh Virdee discusses the endodontic retreatment of a maxillary first molar in this award-winning case
DS, a 36-year-old photographer, was referred from his general dental practitioner (GDP) to the local restorative department for endodontic retreatment of a previously root-filled maxillary first molar. This report aims to discuss the examination, treatment planning, and endodontic management of this tooth, which present several complicating features.
History
Presenting complaint
Patient DS presented with persistent dull pain arising from the upper right area of the mouth.
History of complaint
Patient DS complained of a well-localized, moderate but constant dull ache arising from the right maxillary first molar (UR6). This started 9 months prior following an acute episode that was managed by his general dentist with antibiotics and is exacerbated only by masticatory forces with no sensitivity to thermal stimuli. The pain, which fortunately does not disturb his sleep, was being managed by over-the-counter analgesics.
He recalls that the tooth in question had previously undergone root canal therapy approximately 9 years ago as a result of extensive caries. This was allegedly completed over a single visit with no recollection of rubber dam use and, upon completion, was coronally restored with a direct restoration.
Relevant dental and social history
DS regularly attends his general dentist and has adopted an excellent oral hygiene regime, a low cariogenic diet, has never smoked, and presents little to no anxiety or parafunction.
Relevant medical history
No relevant medical history or known drug allergies reported.
Examination
Extraoral assessment
An extraoral assessment concluded a right submandibular lymphadenopathy.
Intraoral assessment
- Soft tissues — nothing abnormal detected
- Hard tissues — a moderately restored dentition with no evidence of caries (Figure 1)
- Periodontal — BPE all 0s with very good oral hygiene and no mobility, recession, or furcations
- Occlusal — Class I incisors and group function on lateral excursions with no interferences

Figure 1: Dental charting
Right maxillary first-molar assessment
- Visual — a moderately sized mesio-occlusal amalgam restoration with an intact mesial contact, but marginal ditching on the occlusal aspects. There was no evidence of caries, cracks, periodontal pocketing, or mobility; and approximately 60% of natural tooth structure remained. (Figure 2)
- Pulpal — repeated negative readings to electrical and thermal sensibility testing
- Periodontal — no pocketing, mobility, recession, or furcation involvement
- Apical — moderate tenderness to apical percussion, particularly on the mesiobuccal cusp tip. Although there was no apical swelling or sinus tract, on palpation there was tenderness on the attached buccal mucosa adjacent to the UR6.
- Radiographic — an intraoral periapical radiograph taken using a long cone paralleling technique revealed a well-corticated apical radiolucency greater than 5 mm, associated with a significantly curved mesiobuccal root (>40º) and no evidence of MB2 instrumentation. Additionally, the coronal restoration extends to the floor of the pulp chamber. Assessing against the quality guidelines, the previous root filling could be improved as it was poorly condensed and not extended to the appropriate length (European Society of Endodontology, 2006). Furthermore, there was a close anatomical relationship between the root apices and maxillary sinus (Figure 3).

Figure 2: Clinical photograph of UR6
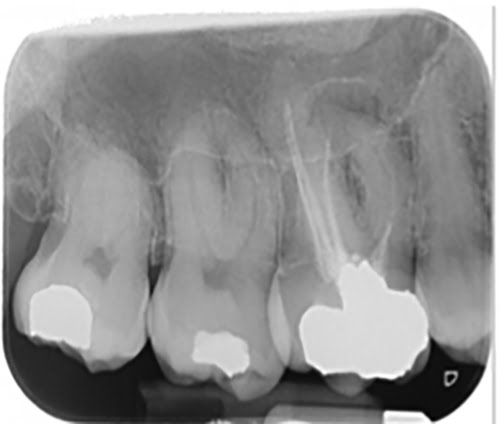
Figure 3: Preoperative long-cone periapical radiograph of UR6

Figure 4: Single tooth isolation of UR6
Diagnosis
Using the classification system set out by Abbott and Yu (2007), the diagnosis was chronic apical periodontitis with a previous but infected root canal filling (Abbott,
Yu, 2007).
Prognosis and treatment plan
Ng, et al., 2011, reported the presence of a preoperative periapical lesion, considerably reduced periapical healing, and this is a significant prognostic factor, which is consistent with landmark Toronto studies (Ng, Mann, Gulabivala, 2011; Farzaneh, Abithol, Friedman, 2004). Additionally, it was found that the size of the apical lesion also had a statistical significance on treatment outcomes, with those less than 5 mm healing more favorably as opposed to those that were larger (Ng, Mann, Gulabivala, 2011).
Unfortunately, these features were all present in this case, reducing overall prognosis. However, the tooth also possessed several features that have been shown to improve treatment outcomes, such as the presence of a technically inadequate root filling, substantial natural tooth structure, and adequate periodontal health with the absence of any perforations, sinus tracts, or apically extruded root-filling material (Ng, Mann, Gulabivala, 2011; Farzaneh, Abithol, Friedman, 2004).
The preoperative prognosis, therefore, was deemed slightly more favorably as “guarded” and conveyed to the patient, as well as all relevant options, which included:
- Leave
- Orthograde retreatment
- Referral to specialist endodontist
- Extract and accept space
- Extract and fill space
DS still wished to retain the tooth and agreed upon the following treatment plan:
- UR6 orthograde endodontic retreatment
- Direct composite core and coronal restoration
- Clinical and radiographic 12 monthly reviews
Treatment protocol: first appointment
Isolation and endodontic access
Upon achieving profound anesthesia, single tooth isolation was achieved using a winged molar clamp, rubber dam, floss, and a caulking agent (Figure 4). The absence of any leaks into the oral cavity on water application from the triple air syringe confirmed a hermetic seal. Prior to access, the preoperative radiograph was studied closely to estimate the depth of the amalgam core restoration (Figure 3). A basic outline of an orthodox access cavity was then scribed into the amalgam surface, and the predetermined depth was used to orientate a round-ended, tapered, cooled diamond bur during access to prevent causing iatrogenic injury. At the floor of the pulp chamber, a safe-ended tungsten carbide bur was used to remove the roof the pulp chamber, ensuring the minimally invasive access cavity permitted good visibility, was a reservoir for irrigants, and straight-line access to all canal orifices.
Identifying canals
Once access was gained, the pulpal floor was inspected for existing injuries and uninstrumented canals. Four canals were identified, three had been previously obturated, and the MB2 was left uninstrumented. Estimated working lengths for each canal were established using the preoperative radiograph, and then a glide path was established in the MB2 using ISO size 8-20 K-files and a ProTaper Universal Sx file (Dentsply) with lubricant (Figure 5, Table 1).
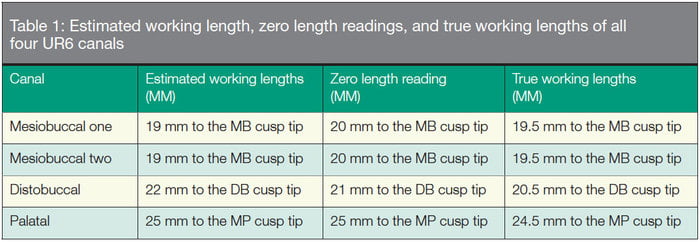

Figure 5: Endodontic access

Figure 6: True working-length radiograph
Gutta-percha removal
The estimated length of gutta percha (GP) was established from the preoperative radiograph. Gross GP was initially removed by a combination of Gates Glidden burs and Hedstrom files set to the length of GP. Fine remnants were then retrieved by introducing solvents into each orifice and using large paper points in a “wicking” motion until all canals were patent and no further GP residue was visible on the terminal third of the paper points. Using an Electronic Apex Locator (EAL) and an ISO size 10 K-file, zero length readings for each canal were established. For each reading, 0.5 mm was subtracted to establish the true working length and then confirmed with a true working length long cone periapical radiograph (Table 1, Figure 6).
Chemomechanical debridement
All canals were shaped to length using the ProTaper Universal Rotary system (Dentsply) with the mesiobuccal one, mesiobuccal two, and the distobuccal canals shaped to an ISO 25 F2, and the palatal shaped to an ISO 30 F3. The varying taper of these files allowed the author to monitor shaping technique throughout the procedure. If carried out correctly, the shaper files should present with dentinal debris in the coronal aspect of the instrument, whereas this should be located in the apical region of finisher files (Figure 7). All shaping was conducted in the presence of copious irrigation (sodium hypochlorite 5.5%) to aid removal of debris from the canal, to lubricate files to prevent separation, and to chemically disinfect the root canal system, which is the critical component to a successful outcome. Following shaping, the tooth was temporized with non-setting calcium hydroxide paste and a distinctly colored glass ionomer temporary restoration.
Treatment protocol: second appointment
Trial cone radiograph
After regaining access and single tooth isolation, canals were dried using paper points, and the respective GP cones were inserted to assess for tug back at the measured true working lengths. A trial cone periapical radiograph was then taken to confirm the shaping was completed to a satisfactory standard and to the correct length prior to obturation (Figure 8).
Irrigation activation
Regardless of its many favorable properties, sodium hypochlorite is still unable to dissolve the inorganic component of the smear layer (American Association of Endodontists, 2011). This mineral film, which covers instrumented walls, can harbor residual microorganisms and impede the ability of sodium hypochlorite to penetrate deep into the dentine tubules, reducing its overall antimicrobial effect (Violich, Chandler, 2010). Therefore, to achieve a more thorough disinfection, a 1-minute penultimate rinse of 17% EDTA was carried out upon completion of all mechanical instrumentation. This combination is a recognized technique and has shown to significantly improve the treatment outcomes of teeth undergoing endodontic retreatment (Ng, Mann, Gulabivala, 2011).
With the smear layer now effectively removed, a final rinse of 5.25% sodium hypochlorite was administered. For each canal, a corresponding GP cone was inserted for manual dynamic activation of the irrigant before the canals were thoroughly dried and then finally obturated. Throughout the procedure, any change in solution was preceded by a saline flush to neutralize the effects of the former irrigant.
Obturation
A warm vertical condensation technique was used to obturate the canals after the canals were thoroughly dried. Initially, the GP was coated with a calcium hydroxide based sealer (AH Plus®, Dentsply). When it was then inserted into the canal to length, the System B™ Tip (Kerr Dental) was activated to 5 mm short of the true working length. At this length, the tip was deactivated and the excess coronal GP removed on withdrawal. The remainder of the canal was then obturated with thermoplastic GP in 2 mm increments using the Obtura™ system (Kerr Dental) (Figure 9).
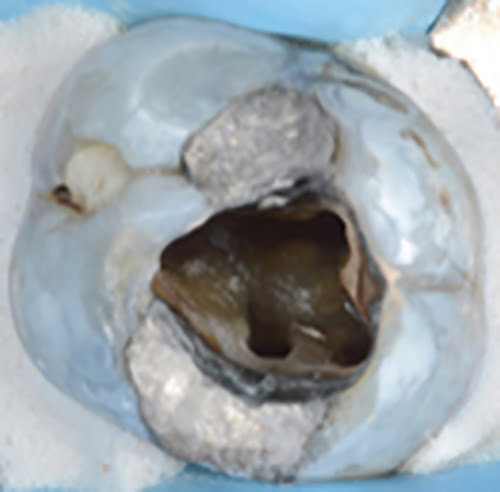
Figure 7: Gutta percha removed, and all canals shaped
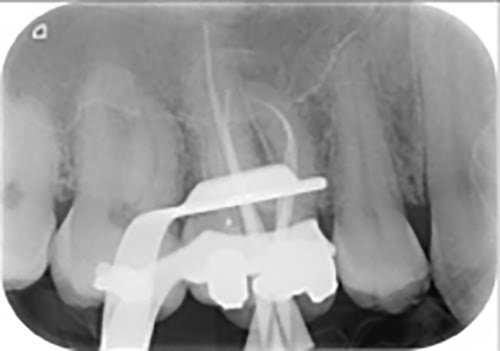
Figure 8: Trial gutta-percha radiograph
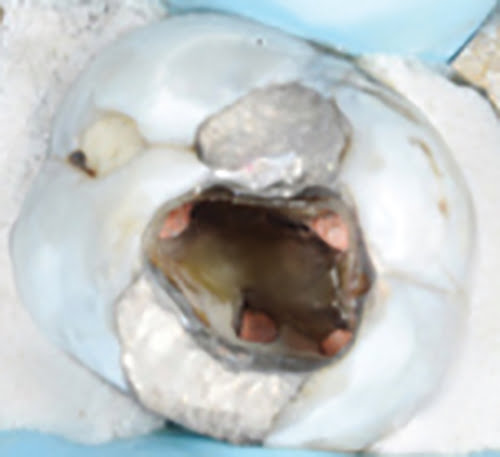
Figure 9: Obturated canals
Coronal seal
A definitive restoration was immediately placed after obturation, as Chugal, et al., 2007, reported those of a temporary nature result in higher failure rates. Initially, 3 mm of flowable composite was used to seal the orifices of the canals, and then a direct hybrid composite restoration was used to restore the lost tooth substance (Figure 10). Although there was no mesial marginal ridge, a substantial amount of natural tooth structure was preserved, and the remaining cusps retained a critical thickness of 2.5 mm. Additionally, the tooth was not at the terminus of the arch and was occlusally protected against excessive axial forces during excursive movements. These are all features that have been shown to improve the healing and long-term survival of the tooth, and so a conservative direct composite coronal restoration was deemed appropriate (Polesel, 2011; Ng, Mann, Gulabivala, 2011). Following this, a postoperative periapical radiograph was taken to assess the quality of the endodontic root filling (Figure 11). This showed that the GP was obturated to the correct length; there were no voids, extrusions or overfills. Additionally, the radiolucency does not appear to have increased in size.

Figure 10: Direct composite coronal restoration
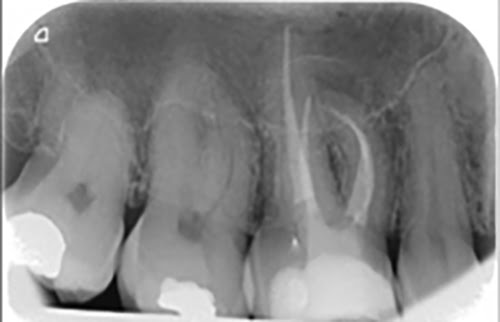
Figure 11: Postoperative radiograph

Figure 12: Twelve-month postoperative radiograph
Review
At 6 and 12 months, DS presented with no symptoms and had stated that there had not been any postoperative acute episodes. The tooth was now functional as he was able to eat on this side without feeling any pain. Clinically, the coronal restoration was intact, and there was no evidence of active infection. Radiographic examination revealed the apical lesion had significantly reduced in size (Figure 12). Due to the absence of any symptoms and radiographic evidence of healing, the case was deemed as successful, and DS was discharged back to his general dentist and advised to be re-referred should any issues occur.
Discussion
If the aim of root canal therapy is to resolve infection, then it could be assumed that the strict definition of endodontic success is to achieve complete resolution of apical periodontitis. This would mean that even in the absence of clinical symptoms and the presence of a comparatively reduced radiographic apical lesion, this case would still be considered a failure. However, it is well recognized that healing is a dynamic process that can take between 2 to 5 years to occur, and an appropriate follow-up period is required to truly determine if success has been achieved (Eriksen, Ørstavik, Kerekes, 1988; Byström, et al., 1987; Ørstavik, 1996). This is echoed in the quality guidelines, which recommend an annual follow-up period for up to 4 years at which only then can failure be determined (European Society of Endodontology, 2006). Therefore, at this stage, describing outcomes dichotomously as a success or failure may not be representative of the dynamic healing process that is occurring.
However, one such classification system that does take this into account is the one set out by Friedman and Mor (2004) where endodontic outcomes are described as being either “healed,” “healing,” or “diseased.” The most appropriate term for this case would be “healing” due to the absence of clinical symptoms and the significant reduction in the mesiobuccal periapical radiolucency at the 12-month review. This restoration of function would translate to an overall “good” outcome and will require further review to assess if the well-corticated apical lesion has completely healed, which would then become an “excellent” outcome. Technically, the outcome meets all of the desirable criteria outlined in the quality guidelines and would be considered an “excellent” outcome in this context (European Society of Endodontology, 2006).
Conclusion
Overall, this case encompassed a combination of several complicating factors that challenged the author’s endodontic clinical skills and knowledge. The author has learned to be insightful and critical of his own work, to employ a systematic strategy to manage complications, and the value of using the literature to overcome challenges and develop as a clinician.
Award-winning case: Dr. Satnam Singh Virdee won the Young Dentist Endodontic Award 2016 for this case. Find out more at bit.ly/2jiuSLd.
References
- Abbott PV, Yu C. A clinical classification of the status of the pulp and the root canal system. Aust Dent J. 2007;52(suppl 1):17-31.
- American Association of Endodontists. AAE Endodontic Case Difficulty Assessment Form and Guidelines . https://www.aae.org/caseassessment. Accessed June 6, 2016.
- American Association of Endodontists. Winter 2011 ENDODONTICS: Colleagues for Excellence newsletter: Root canal irrigants and disinfectants. https://www.aae.org/publications-and-research/endodontics-colleagues-for-excellence-newsletter/root-canal-irrigants-and-disinfectants.aspx. Accessed June 6, 2016.
- Byström A, Happonen RP, Sjögren U, Sundqvist G. Healing of periapical lesions of pulpless teeth after endodontic treatment with controlled asepsis. Endod Dent Traumatol. 1987;3(2):58-63.
- Chugal NM, Clive JM, Spångberg LS. Endodontic treatment outcome: effect of the permanent restoration. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 2007;104(4):576-582.
- Eriksen HM, Ørstavik D, Kerekes K. Healing of apical periodontitis after endodontic treatment using three different root canal sealers. Endod Dent Traumatol. 1988;4(3):114-117.
- European Society of Endodontology. Quality guidelines for endodontic treatment: consensus report of the European Society of Endodontology. Int Endod J. 2006;39(12):921-930.
- Falcon HC, Richardson P, Shaw MJ, Bulman JS, Smith BG. Developing an index of restorative dental treatment need. Br Dent J. 2001;190(9):479-486.
- Farzaneh M, Abitbol S, Friedman S. Treatment outcome in endodontics: the Toronto study. Phases I and II: orthograde retreatment. J Endod. 2004;30(9):627-33.
- Friedman S, Mor C. The success of endodontic therapy — healing and functionality. J Calif Dent Assoc. 2004;32:493-503.
- Ng YL, Mann V, Gulabivala K. A prospective study of the factors affecting outcomes of nonsurgical root canal treatment: part 1: periapical health. Int Endod J. 2011;44(7):583-609.
- Ng YL, Mann V, Gulabivala K. A prospective study of the factors affecting outcomes of non-surgical root canal treatment: part 2: tooth survival. Int Endod J. 2011;44(7):610-625.
- Ørstavik D. Time-course and risk analyses of the development and healing of chronic apical periodontitis in man. Int Endod J. 1996;29(3):150-155.
- Polesel A. The conservative restoration of single posterior endodontically treated teeth. Ital J Endod. 2011;25:3-21.
- Violich DR, Chandler NP. The smear layer in endodontics — a review. Int Endod J. 2010;43(1):2-15.
Stay Relevant With Endodontic Practice US
Join our email list for CE courses and webinars, articles and more..


