CE Expiration Date: September 1, 2026
CEU (Continuing Education Unit):2 Credit(s)
AGD Code: 070
Educational aims and objectives
This self-instructional course for dentists aims to focus on some challenges of irrigating anatomic complexities.
Expected outcomes
Endodontic Practice US subscribers can answer the CE questions by taking the quiz to earn 2 hours of CE from reading this article. Correctly answering the questions will demonstrate the reader can:
- Distinguish between the mechanism of action, benefits, drawbacks and safety issues of Positive Pressure Irrigation (PPI), Negative Pressure Irrigation (NPI), Closed System Negative Pressure Irrigation (CSNPI), and Multisonic Ultracleaning Systems (MUS).
- Realize some statistics about the causes of root canal
- Identify some more recent root canal technologies.
- Identify what could happen if the direction of vacuum is reversed.
- Realize the concept and advantages of “The Forward Effect” caused by the vacuum on multi-cannular drawn NaOCl- irrigation in MIE preparations.
Drs. L. Stephen Buchanan and Christophe Verbanck explore systems for irrigation of root canals and the advantages of closed-system negative pressure irrigation.
Drs. L. Stephen Buchanan and Christophe Verbanck explore irrigation of root canal systems
Irrigation of root canal systems is the most important aspect of RCT,1,2,3 yet it may also be the least understood action we do inside these complex spaces.4 Evidence for that statement is the fact that, to this day, very few endodontists understand how the introduction of rotary shaping files caused an increase in our irrigation failures,5 including the fact that a large proportion of endodontists instrument with NaOCl6,7 and still think we clean canals with files.5,8
Does this lack of understanding about irrigation fundamentals translate into RCT failures? The answer is yes, although these cases are seldom correctly diagnosed after the fact.
A randomized multi-center study done by Nixdorf, et al.,9 showed that 11% of patients in pain and seen by endodontists were not pain-free 6 months later! Half of these patients were misdiagnosed myofascial pain cases — they didn’t need RCT. The other half did need RCT, but 40% of this group received RCT on an adjacent tooth — so much for pulp testing — leaving the remaining cases that did need RCT, had the correct tooth treated, but remained symptomatic.
Virtually all of these cases had a history of severe pulpitis or partial necrosis before RCT, indicating to the authors that the most likely etiology for those teeth to continue to be symptomatic was due to pulp remnants left by the irrigation procedure; said irrigation failure rate being 3.3% of the patients presenting in pain.
Of the eleven percent of those still in pain 6 months later, half of those — 5.5% didn’t need RCT, and 40% of the other half had the wrong tooth treated, leaving 60% of 5.5% which calculates at 3.3 of our cases. That’s not a small issue if you consider the fact that 25 million RCTs10 are done in the U.S. alone every year, revealing approximately 825,000 RCT irrigation failures per year — a number that closely relates to the findings in a previous study by Nixdorf, et al., on persistent tooth pain after RCT.11

The challenge of irrigating anatomic complexities
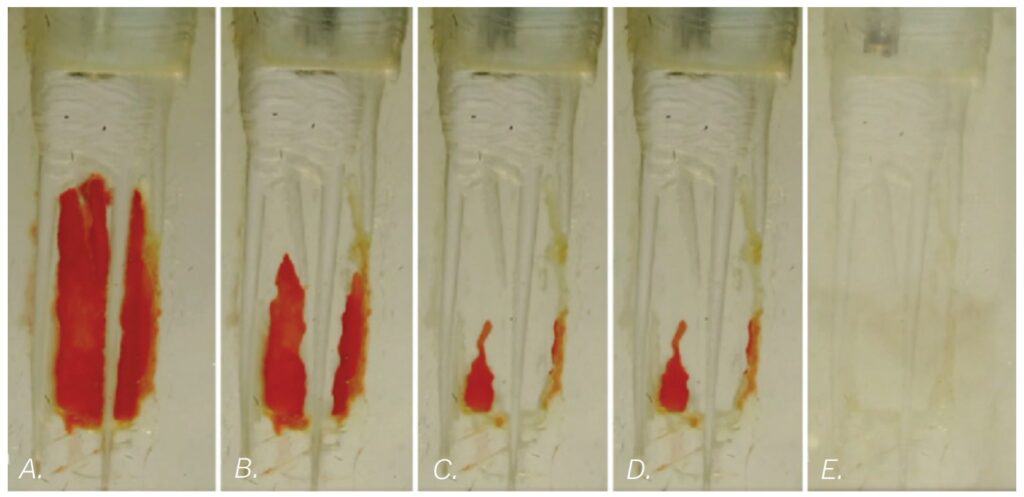
Complete removal of pulp tissue during RCT is not a simple job due to the anatomic complexity of root canal systems and the fact that NaOCl dissolves pulp tissue in a linear fashion, not as a catalytic reaction (Figure 2).7,8 While a broached pulp can be completely dissolved in a minute or two when dropped into a dappen dish of bleach, it can take 40 minutes of passive positive pressure irrigation to digest the same volume of pulp tissue out of an MB canal system contained inside an upper molar. Fortunately, irrigation technology is rapidly improving our ability to eliminate lateral pulp remnants in spite of the current trend toward minimally invasive instrumentation.

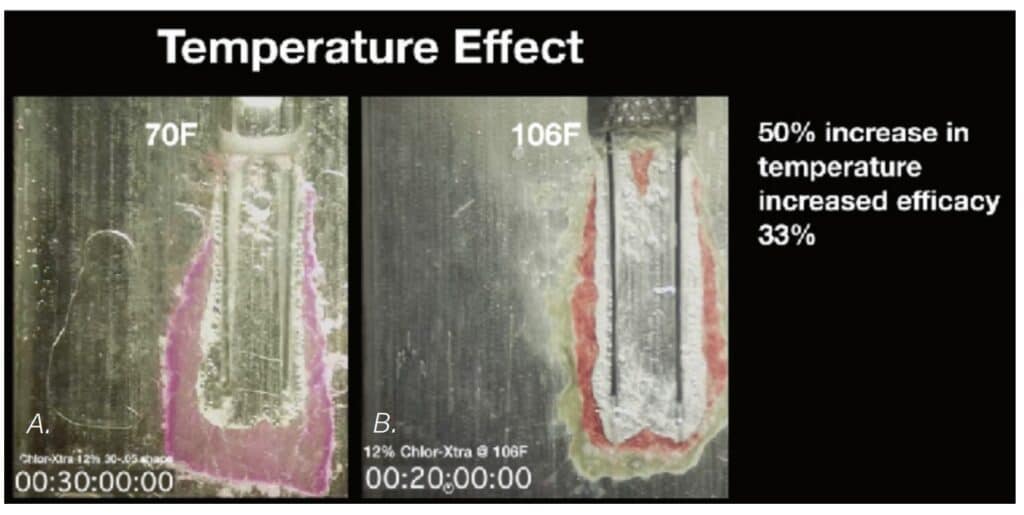
Stojicic, et al., in 2010, looked at the effects of concentration, temperature, and agitation on NaOCl efficacy and found that dissolution efficacy increased almost linearly with the concentration of NaOCl. Higher temperatures and agitation considerably enhanced the efficacy of NaOCl, although agitation had a greater effect than temperature, and continuous agitation resulted in the fastest tissue dissolution. Their comment that “Optimizing the concentration, temperature, flow, and surface tension can improve the tissue dissolving effectiveness of NaOCl even 50-fold” seemed a bit far-fetched when first read;12 however, our own research (unpublished data) on the rates of pulp dissolution from isthmus spaces have confirmed that this is possible.

New irrigation technologies
There are many ways to intermittently agitate (cavitate) NaOCl in root canal systems — sonic, ultrasonic, and laser activation, but GentleWave® irrigation (GW), developed by Sonendo® (Sonendo Inc., Laguna Hills, California), is one of the few irrigation methods that delivers continuous agitation to all canals simultaneously. They pump the irrigating fluids up to 9000 psi, and blast them into and out of the access cavity, creating a negative pressure Bernoulli effect in the RCS to prevent NaOCl from escaping into peri-radicular tissues. Much is made of the sonic energy GW imparts to the solutions, but the greatest mechanism of action is more likely the 250 ml of NaOCl shot through the tooth during the 5-minute NaOCl cycle, allowing accelerated dissolution of pulp tissue in canals (Figure 4).13

After 40 to 50 RCT procedures successfully done with GW, the senior author had his first case failure in a red-hot C-shaped lower molar that remained symptomatic after RCT was completed (Figure 5). The case looked pretty nice when finished — several filled lateral aberrations were seen postoperatively, but the patient complained about pain that continued to be referred to his right endo zone (below the malar eminence, above the lower border of the mandible). This being a C-shaped molar, the best hypothesis for the etiology of this failure was incomplete debridement of pulp tissue in the large isthmus spaces (Figure 6).


A novel isthmus replica
To test this hypothesis, a research device was designed to replicate the isthmus morphology seen in these molars. This was 3D-printed in two halves so a pulp replica (porcine muscle tissue) could be inserted into the isthmus form before they were assembled with light-cure adhesive (Figure 7). This novel in vitro device was capable of displaying how pulp dissolution occurs in isthmus spaces when a number of variables are compared, said variables being NaOCl concentration, temperature, fluid flow, and agitation.

The first irrigation method tested in the isthmus block was of course GW, and it confirmed my hypothesis about the cause of my C-shaped molar failure — at the end of the 5-minute NaOCl cycle, significant amounts of pulp replica remained. Also confirmed by this test was the fact that EDTA — even when activated by multi-sonic energy — has zero ability to digest organic tissue, so it could be said that GW’s primary mechanism of action (MOA) for pulp dissolution is hosing root canal systems with enormous volumes of NaOCl (Figure 8).
Negative pressure irrigation (NPI) versus positive pressure irrigation (PPI)
The isthmus research blocks were then used to investigate NPI because the literature shows excellent cleaning of isthmus spaces with EndoVac™ (EV) by Kerr Endodontics.14,15,16 Is it the direction the solutions are moving through the canal? Is it because EV eliminates “vapor lock” — the gas bubbles liberated during pulp saponification?17 Isthmus block studies showed the only difference between PPI and NPI was that the latter requires constant replenishing of solutions, whereas dentists using PPI tend to irrigate and let the solutions soak in the patient’s tooth — radically decreasing the volume of solutions run through root canals. When constant irrigation was used for both NPI and PPI, the results were identical (Figure 9).

Therefore, while EV is 100% safe from irrigation accidents,18,19 it was poorly designed and was pedantic to use because of the constant attention needed and because of its propensity to clog up every 5 minutes of use. Worse than that, EV is uni-canular, meaning it only irrigates a single canal at a time so a four-canal molar requires 20 minutes of intensive hands-on work.

unclogging the cannula every 5 minutes. 10C. The ultimate objective for this irrigating system was to have manifolds and cannulae for each canal so multicanalar irrigation can happen. Originally the vacuum was connected to the cannula, and the irrigants inlet was placed just inside the access cavity
Investigating closed-system negative pressure irrigation (CSNPI)
Eliminating intensive hands-on requirements was simple in a closed system as the solutions could then be pulled into the pulp chamber by the vacuum coming through the micro-cannulas from the chairside evac system (Figure 10). The results from the extracted tooth experiment (Figure 11) as seen in SEM imaging were exceptional, but it took 30 minutes due to the repeated clogging of the microcannula.

The reversal
The senior author then had the epiphany that clogging would never be an issue if the direction of vacuum were reversed, so that change was made, and another isthmus block study was kicked off. Shortly after beginning, it became apparent that not only was the cannula blockage issue solved, but that the vacuum-drawn outflow of NaOCl through the end of the blunt-cut cannula was dissolving pulp replica at a remarkable rate (Figure 12), most likely due to the constant, rapid fluid flow of sodium hypochlorite exiting the cannula ends.

There was initial concern about the inherent safety of NaOCl flowing out of an open-ended cannula, until it was realized that vacuum-drawn irrigation immediately ceased the moment an open-ended needle was locked in a canal, rendering it impossible to cause a hypochlorite accident with this MOA (Figure 13).

The Forward Effect
Then, as the studies continued, it became apparent that drawing the NaOCl out the end of the cannula with vacuum pressure was having its effect at least 5 mm forward of the cannula end. This was very providential as it meant that irrigating cannulae had only to be placed to mid-root in most canals, a definite advantage when dealing with severely curved canals, especially when cutting minimally-invasive canal preparations.20 EV, by comparison, requires a .35 mm 4 % apical preparation diameter,21 a shaping objective that invites apical damage in curved canals.5
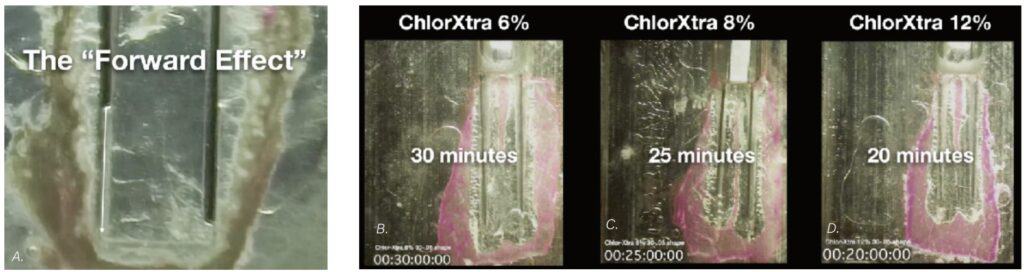
Over the following months, the isthmus research block was used to compare the effects of different irrigation variables. Simply choosing a higher NaOCl concentration has significant effect on the speed of dissolution (Figure 14). Raising the irrigant’s temperature from 70ºF (21.1C) to 100ºF (37.7C) increasinged the speed of dissolution by 33% (Figure 15), and the shear forces of agitation — provided in this case by aerating the solution to cause gas bubble cavitation — doubled the speed of dissolution (Figure 16), confirming Stojicic, et al.’s findings12 that agitation brought more effect than temperature. All irrigation tests were done with a constant flow of solutions — another variable critical to GW’s MOA.

Finally, a study was done with 12% NaOCl irrigant that was aerated and heated to 120° F (48,9°C), and the isthmus pulp replica was gone in just over 7 minutes (Figure 17).

Case outcomes



In conclusion: features, advantages, and benefits of CSNPI
Closed-system negative pressure irrigation (CSNPI) has several advantages over conventional open-system irrigation (PPI or NPI):
- CSNPI can be multi-cannular. Multi-cannular means that it can clean all of the canals in a given tooth at the same time. Only laser-driven PIPS (photo-induced photo-acoustic streaming), GentleWave, and PulpSucker irrigation can do this. Why is this important? Because endodontists treat mostly multi-cannular molars, so any irrigation method that is uni-cannular is non-optimal and time consuming.
- CSNPI is more effective than open-system irrigation. Open-system NPI can have constant irrigation flow but only in a single canal at a time, so even though EV ads say they can reduce a 40 minute irrigation time to 5 minutes, clinicians have to hang onto an EV syringe for 20 minutes in a 4-canal molar. That is just untenable for specialists doing 4 to 8 cases a day.
- CSNPI can be hands-free. CSNPI can do its work without dentist or assistant in the operatory. GentleWave irrigation is fast, but operators must hold onto the GW procedure instrument in a very focused manner for 8 minutes after the preparatory 3-5 minutes of hands-on PulpSucker irrigation can be staged in less than 5 minutes, after which it is entirely hands-off.
- CSNPI decreases immediate post-op symptoms. All pain of endodontic origin is a pressure phenomena. “Hot teeth” are exquisitely tender to touch because of the peri-radicular tissue pressure induced by severe inflam Closed-system irrigation applies vacuum pressures to the RCS but also to PA tissues beyond the root, and although evidenced-based clinical trials have not been completed yet, clinical experiences indicate that patients who had RCT with CSNPI experience much less post-op pain when the anesthesia wears off than patients who had RCT in teeth irrigated conventionally.

After reading about irrigation of root canal systems, see what Drs. Buchanan and Verbanck have to say about rotary negotiation as first file to length here: https://endopracticeus.com/rotary-negotiation-as-first-file-to-length/
References
- Gu LS, Kim JR, Ling J, Choi KK, Pashley DH, Tay FR. Review of contemporary irrigant agitation techniques and devices. J Endod. 2009 Jun;35(6):791-804.
- Liu H, Shen Y, Haapasalo M. Effectiveness of Six Irrigation Techniques With Sodium Hypochlorite in Tissue Dissolution. 2023 May 18;15(5):e39208.
- Gulabivala K, Ng YL, Gilbertson M, Eames I. The fluid mechanics of root canal irrigation. Physiol Meas. 2010 Dec;31(12):R49-84.
- Boutsioukis C, Arias-Moliz MT. Present status and future directions – irrigants and irrigation methods. Int Endod J. 2022 May;55 Suppl 3(Suppl 3):588-612.
- Buchanan LS, Verbanck CLM. Root canal shaping in the age of minimally invasive endodontics (MIE). Endod Practice US. 2023; 16(1): 20-24.
- McComb D, Smith DC. A preliminary scanning electron microscopic study of root canals after endodontic procedures. J Endod. 1975 Jul;1(7):238-242.
- Zehnder M. Root canal irrigants. J Endod. 2006 May;32(5):389-398.
- Peters OA. Current challenges and concepts in the preparation of root canal systems: a review. J Endod. 2004 Aug;30(8):559-567.
- Nixdorf DR, Law AS, John MT, Sobieh RM, Kohli R, Nguyen RH; National Dental PBRN Collaborative Group. Differential diagnoses for persistent pain after root canal treatment: a study in the National Dental Practice-based Research Network. J Endod. 2015 Apr;41(4):457-463.
- American Association of Endodontists. AAE Root canal safety talking points. https://www.aae.org/specialty/wp-content/uploads/sites/2/2017/06/rootcanalsafetytalkingpoints.pdf. Accessed August 10, 2023.
- Nixdorf DR, Moana-Filho EJ, Law AS, McGuire LA, Hodges JS, John MT. Frequency of persistent tooth pain after root canal therapy: a systematic review and meta-analysis. J Endod. 2010 Feb;36(2):224-230.
- Stojicic S, Zivkovic S, Qian W, Zhang H, Haapasalo M. Tissue dissolution by sodium hypochlorite: effect of concentration, temperature, agitation, and surfactant. J Endod. 2010 Sep;36(9):1558-1562.
- Haapasalo M, Wang Z, Shen Y, Curtis A, Patel P, Khakpour M. Tissue dissolution by a novel multisonic ultracleaning system and sodium hypochlorite. J Endod. 2014 Aug;40(8):1178-1181.
- Versiani MA, Alves FR, Andrade-Junior CV, Marceliano-Alves MF, Provenzano JC, Rôças IN, Sousa-Neto MD, Siqueira JF Jr. Micro-CT evaluation of the efficacy of hard-tissue removal from the root canal and isthmus area by positive and negative pressure irrigation systems. Int Endod J. 2016 Nov;49(11):1079-1087.
- Yoo YJ, Lee W, Kim HC, Shon WJ, Baek SH. Multivariate analysis of the cleaning efficacy of different final irrigation techniques in the canal and isthmus of mandibular posterior teeth. Restor Dent Endod. 2013 Aug;38(3):154-159.
- Siu C, Baumgartner JC. Comparison of the debridement efficacy of the EndoVac irrigation system and conventional needle root canal irrigation in vivo. J Endod. 2010 Nov;36(11):1782-1785.
- Estrela C, Estrela CR, Barbin EL, Spanó JC, Marchesan MA, Pécora JD. Mechanism of action of sodium hypochlorite. Braz Dent J. 2002;13(2):113-117.
- Desai P, Himel V. Comparative safety of various intracanal irrigation systems. J Endod. 2009 Apr;35(4):545-549.
- Azim AA, Aksel H, Margaret Jefferson M, Huang GT. Comparison of sodium hypochlorite extrusion by five irrigation systems using an artificial root socket model and a quantitative chemical method. Clin Oral Investig. 2018 Mar;22(2):1055-1061.
- Buchanan LS. Closed-system negative pressure irrigation: A serious inflection point in root canal cleaning. Dentistry Today. April 2020 [Online]. https://www.dentistrytoday.com/closed-system-negative-pressure-irrigation-a-serious-inflection-point-in-root-canal-cleaning/. Accessed August 10, 2023.
- Kerr Endodontics. EndoVac Apical Negative Pressure Irrigation System Instructions for use. Download for instructions can be found at: https://www.kerrdental.com/download-centre?f%5B0%5D=field_resource_document_type%3A633. Accessed August 10, 2023.
Stay Relevant With Endodontic Practice US
Join our email list for CE courses and webinars, articles and more..


