CE Expiration Date: June 6, 2025
CEU (Continuing Education Unit):2 Credit(s)
AGD Code: 690
Educational aims and objectives
This self-instructional course for dentists aims to provide information on how CBCT can be utilized in making treatment decisions by identifying anatomic structures visible on CBCT imaging and understanding the importance of CBCT in implant therapy.
Expected outcomes
Endodontic Practice US subscribers can answer the CE questions by taking the quiz to earn 2 hours of CE from reading this article. Correctly answering the questions will demonstrate the reader can:
- Recognize the importance that CBCT imaging plays in providing implant therapy.
- Identify the anatomical structures that are necessary to avoid during implant surgery.
- Recognize situations in which only CBCT imaging can identify the proximity of vital anatomic structures to the planned implant position.
Dr. John Pasicznyk offers endodontists some insights into preparing and imaging with CBCT for implant surgery if endodontic options are not appropriate.
Dr. John Pasicznyk discusses implants and how CBCT can help endodontists with treatment planning
Implant dentistry is a rapidly growing aspect of the profession as more clinicians start to provide implant therapy as a routine aspect of treatment. This creates an atmosphere where patients are aware of implants as a treatment option and may even question the recommendation to save a tooth rather than remove and replace it with an implant. What once was a specialist-only procedure in the OMFS or periodontal practice is now performed in many general practices, including a growing number of endodontic practices. Since many GPs utilize their endodontic colleagues as a “last resort” at saving a tooth, it is very reasonable for the endodontist to be equipped to help patients make treatment decisions regarding endodontic therapy versus implant therapy, and even to complete the necessary implant procedures if they so desire. Consider how many times a tooth has a severe periapical abscess, which can only be fully appreciated once treatment is initiated, or cracks in the root, which can only be visualized upon opening the tooth and viewing with a microscope. In these cases, proper planning ahead of time, appropriate informed consent, and an adequate armamentarium can allow the endodontic procedure to seamlessly shift to implant placement. This CE will provide vital information in how CBCT can be utilized in making treatment decisions by identifying anatomic structures visible on CBCT imaging and by understanding the importance of CBCT in implant therapy.
CBCT imaging is a vital part of the initial treatment-planning process for implant cases, allowing clinicians to critically think before a patient is even scheduled for treatment. Effective use of CBCT imaging changes the treatment-planning process, with clinicians having all the information needed to choose cases that are appropriate for the skill set and that inform patients of anticipated complications prior to the surgical appointment.1 By utilizing CBCT imaging, clinicians have a comprehensive view of the anatomic field prior to surgery, and in turn, risk of surgical and prosthetic complications are decreased, thereby improving patient outcomes. Endodontic practitioners have an advantage on most GPs in this regard, as they are quite used to viewing and manipulating CBCT images. The tools and planning software may be slightly different, but the general concepts remain the same: Identify anatomy, make measurements, and look for anything outside the ordinary.
It is important to understand some patient management benefits of using CBCT in implant planning. These are the ways we can help our patients before evaluating their anatomy and bone quantity/quality. Patients are walking into the practice more educated than ever before, doing research on procedures, and getting advice from their peers. In today’s age, many patients have heard of CBCT imaging, and for those who haven’t, once they understand why we use it, they insist on friends and family members getting the same level of care. The confidence it gives the clinician to present a well thought-out and safely planned implant case to the patient is without a doubt the largest benefit of CBCT imaging. In the endodontic practice setting, many cases quickly become non-restorable, and having a “Plan B” prior to starting endodontic therapy would give many patients a boost of confidence prior to treatment. Imagine the case in which a referring dentist asks you to play “hero” by completing a massively compromised endodontic case. When the tooth can’t be saved, it can reflect on the clinician despite their best efforts. By identifying specific challenges in the endodontic treatment and by offering an alternative should endodontics not be in their best interest, we can turn what would ordinarily be a difficult patient management situation into a positive end result for the patient.
Patients largely follow our treatment advice, based on the confidence they have in us, and CBCT gives the doctor and team an added level of confidence in planning. When the clinician is able to clearly articulate why the patient is a good candidate for implant surgery and can reassure the patient that everything possible is being done to ensure the best outcome, it reduces barriers for patients to decline treatment, which allows us to provide more implant dentistry for our patients. Finally, having a full understanding of the patient’s specific situation allows the doctor and team to prepare fair financial arrangements prior to surgery, based on whether grafting or sinus augmentation is needed. Doctor and team can also provide a more realistic timeline of the process from start to finish by disclosing any situations that may lengthen healing or total treatment time.
Safely executing a planned procedure should be the number one priority in any aspect of dentistry. This is especially important in surgery, where tissue is being displaced, incised, removed, and rebuilt with a multitude of important vital structures surrounding the surgical site. Injury to any of these could lead to intraoperative complications that the clinician is unprepared to handle, unable to recognize, or unable to repair. This could lead to significant morbidity or even mortality. CBCT imaging is an imperative aspect of pre-implant treatment planning from a standpoint of safety due to the knowledge it provides the clinician. This information is simply impossible to fully gain from a routine examination consisting of intraoral visual exam, palpation, and two-dimensional radiography.
There are five anatomic structures that should be identified as part of any initial implant treatment plan. They are, in the order of importance: submandibular fossa, inferior alveolar nerve (and anterior loop), buccal plate, nasopalatine nerve, and maxillary sinus. There are structures that will not be a consideration based on the planned case — i.e., for a treatment plan to replace tooth No. 14 — the relative location of the submandibular fossa, inferior alveolar nerve (IAN), and nasopalatine nerve will neither influence the treatment plan nor change the safety margins of the surgery. However, each structure should be identified when appropriate, so clinicians can make the proper clinical decision whether their skill set allows them to move forward with the case.
The submandibular fossa lies within the concavity that occurs inferior to the cortical border of the mandible. Oftentimes, the concavity is quite severe, and the scope of the concavity cannot be identified from palpation, visualization, and two-dimensional radiography (Figures 1-3). This area contains a great number of blood vessels and nerves that, if compromised, could create a significant bleed or paralysis. In many instances, the height from alveolar crest to the fossa is 8 mm to 10 mm, which is, quite inconveniently, the same dimension as very commonly used implant length in the lower molar region.2 It would be disastrous to unknowingly have a severe concavity apical to the planned surgical site and begin preparing an osteotomy to the planned implant length, only to drill directly into the submandibular fossa. The results could range anywhere from excessive intraoperative bleeding to severe hemorrhage. Even if handled appropriately, either of these could, in rare circumstances, lead to a delayed submandibular swelling due to bleeding into fascial spaces. In this situation, CBCT imaging would have identified the anatomic situation, and virtually placing an implant with planning software would allow the clinician to plan for a shorter implant to avoid compromising the submandibular fossa.
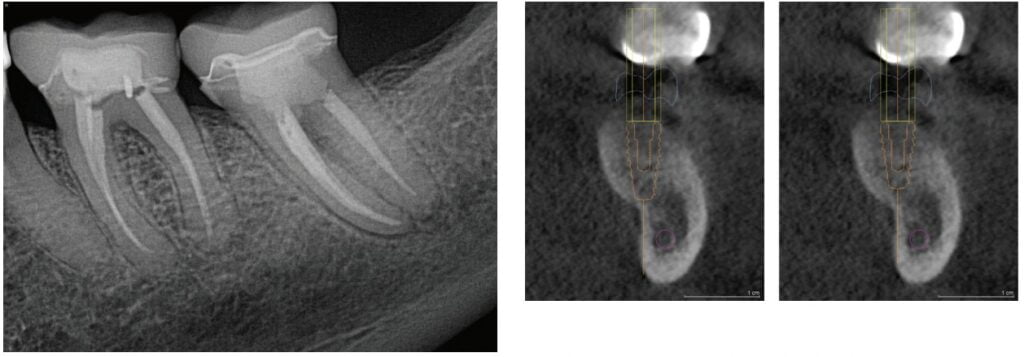
The inferior alveolar nerve (IAN) is a structure housed within a canal made up of cortical bone, which lends it to typically be quite visible on both two- and three-dimensional radiographs. Unlike the submandibular fossa, compromising the IAN or canal will rarely cause a medical emergency. However, damaging the nerve and causing resulting loss of sensation could be a debilitating situation for the patient and create a serious medico-legal event for the clinician.
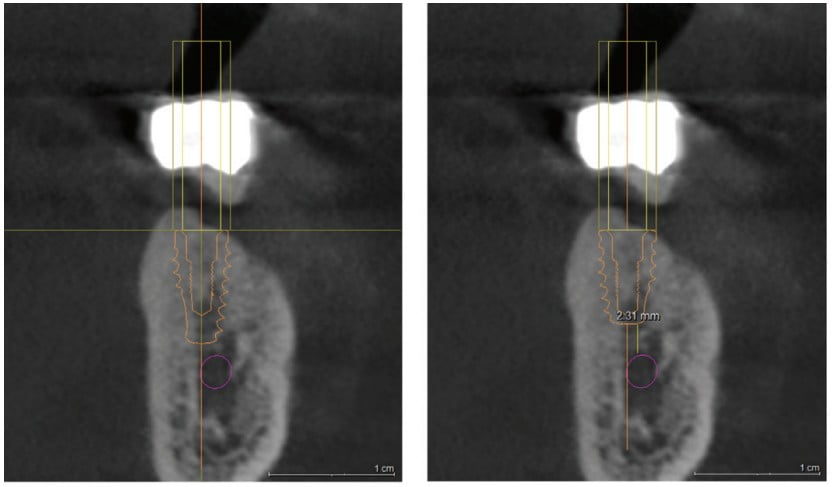
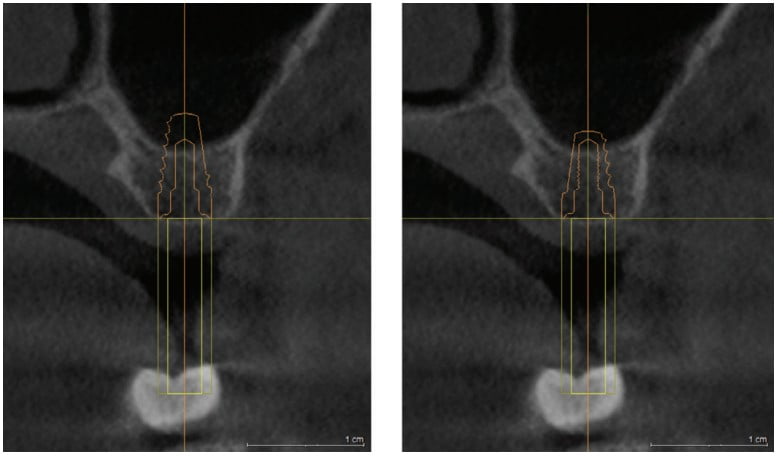
Despite the ability to visualize the nerve canal on two-dimensional radiography, CBCT imaging is the only way to precisely understand the exact height of bone coronal to the nerve. By viewing a CBCT slice, the clinician can determine the appropriate height of implant that can be used without coming near the IAN (Figures 4 and 5). When the nerve position does not allow the use of typical implant length, 8 mm or greater, a short implant can be used with success.3 Short implants are defined as implants less than 7.5 mm in length and are becoming more and more prevalent from manufacturers. In addition to showing the height of bone above the IAN, CBCT slices can also show the relative buccal-lingual position of the IAN. In this case, the nerve was in almost the lingual-most aspect of the inferior border of the mandible, which made the ideal planned implant position greater than 3 mm away from the nerve — an acceptable safety margin. To improve safety even more, a surgical guide fabricated from the CBCT imaging and a digitized dental model would allow precisely placing the implant in the safely planned position.
The buccal plate is a band of cortical bone in both the maxilla and mandible that encapsulates the more cancellous bone within. While violating the buccal plate may not have quite as drastic consequences as injury to the submandibular fossa or IAN, it will have a tremendous impact on the success of the implant surgery. Cortical bone derives most of its blood supply from the periosteum, which means minimizing flap reflection when possible is imperative to preventing bone necrosis. Excessively disrupting the blood supply by denuding bone of its periosteum can cause cortical bone loss.4 This along with the biologic effects of osteotomy preparation, which is known to be a 1.5 mm-2.0 mm band of bone necrosis around the freshly placed implant body, can quickly lead to a dehiscence of bone around the implant body. When this happens, soft tissue can quickly invade the healing implant site, leading to “spinners” or implants that fail to integrate due to soft tissue ingrowth.
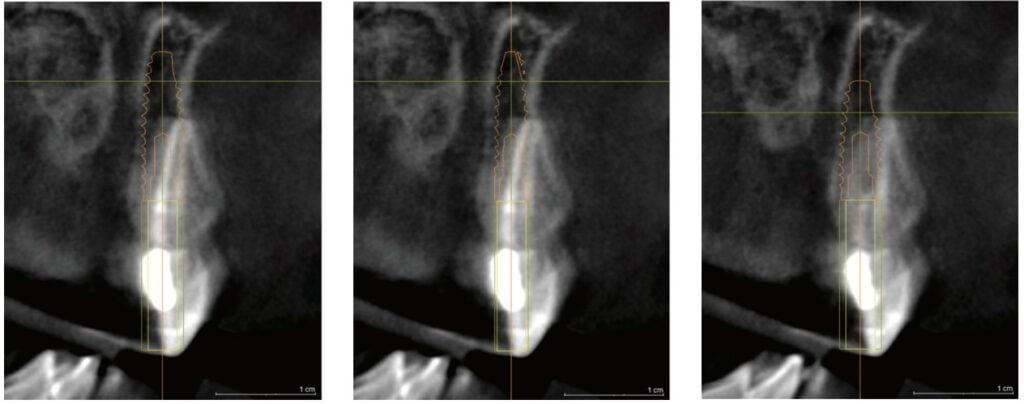
CBCT imaging and implant-planning software with precise digital implant replicas allow the surgeon to visualize an implant within the proposed site and safely determine if the diameter of the implant causes a compromise of the 2.0 mm minimum boundary between implant and buccal plate. If the bone dimension is inadequate, there are three options that can be planned for prior to surgery:
- First, a narrower implant could be selected if appropriate and visualized on CBCT planning software (Figure 6-8).
- Second, by sinking the implant slightly subcrestal, the thin “lip” of buccal plate can be avoided.
- Third, ridge augmentation may be the only way to appropriately increase the volume of bone to adequately secure the implant.
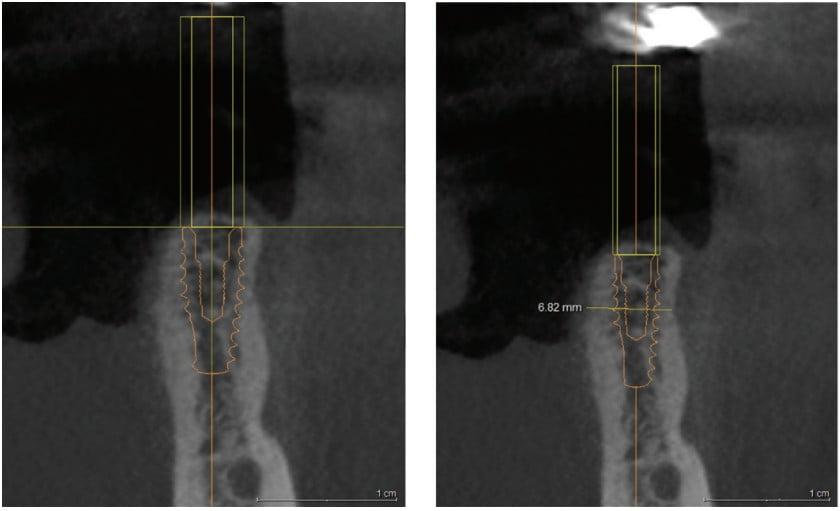
The benefit to both patients and clinicians is that these considerations are being made prior to finalizing the implant treatment plan. The patients receive peace of mind that they are receiving only necessary procedures, and clinicians can rest easy knowing what is coming their way on the day of surgery.
The maxillary sinus is a unique anatomic structure, exhibiting resilience and self-healing capabilities, with a relatively lower risk of serious complications due to damage. Despite this, the sinus is still imperative to manage appropriately, as compromising this structure can significantly increase total time for treatment to be completed. Additionally, being prepared in advance for variation in sinus anatomy allows clinicians to appropriately plan for the procedure prior to the day of surgery.5
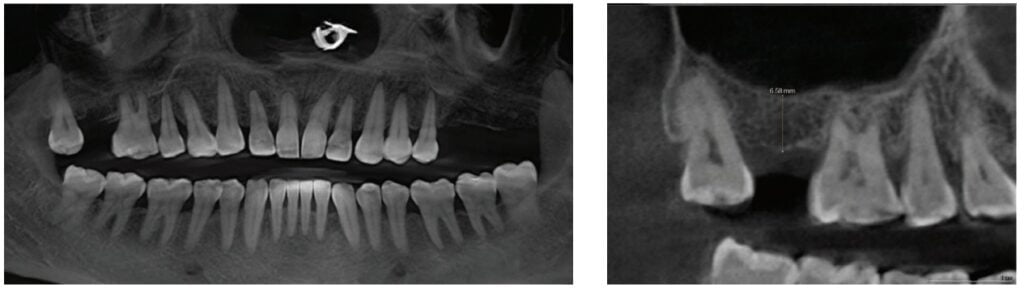
There are many instances where the maxillary sinus has pneumatized, which causes the floor of the sinus to impinge on an otherwise useful implant site. In these cases, a decision can be made whether a shorter implant is appropriate and avoids the sinus entirely, or the sinus can be moved out of the way, building bone in the space between the sinus lining and the maxilla (Figures 9 and 10). In any case, the sinus must be adequately visualized prior to implant surgery. While two-dimensional radiography gives some information as to the extent of the borders of the sinus, it alone is not adequate to fully visualize septa, undulations, and the exact measurement of available bone from crest to sinus (Figures 11 and 12). This measurement of available bone allows clinicians to determine whether the case meets their selection criteria and, ultimately, helps patients understand the extent of treatment required.
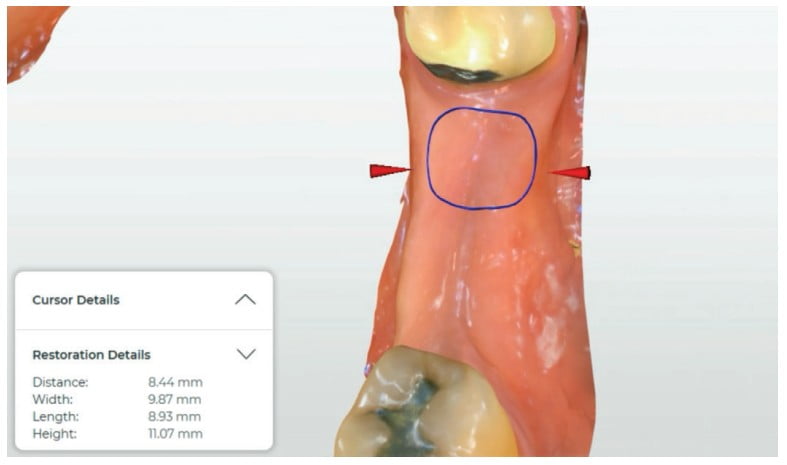
The final anatomic structure to discuss in implant planning is the nasopalatine canal. This structure carries a mixed vascular-neural bundle that exits on the midline palatal to the central incisors. Interestingly, despite being a neurovascular bundle, there is little to no sensory innervation, which reduces the risk of compromising the tissue contained within. In fact, it is the one anatomic structure discussed that can be and, occasionally, is required to be removed entirely.6 Central incisor implants often come close to invading the space of the nasopalatine canal, and care must be given to unintentionally place an implant in the canal. The borders of the canal are made of cortical bone, and will react and atrophy in a similar fashion to the buccal plate if the implant is placed in too close proximity. By utilizing CBCT slices, clinicians can visualize the proximity of the canal to the planned implant position, and adjust the proposed size or the position of the implant in order to avoid the canal (Figures 13 and 14). In cases with such limited space, the implant is placed in the ideal position, even if that means compromising the canal. During implant surgery, the canal will be intentionally exposed and the contents within obliterated entirely to allow for bone grafting material to fill the canal and stabilize the implant (Figure 15).
Implant dentistry is one of the most rapidly growing clinical aspects of dentistry, and this is driven by many barriers of entry being lowered or eliminated. CBCT imaging is arguably the most useful piece of technology to an implant practice, and its routine use in treatment planning will provide the doctor and team many advantages in patient communication and surgical execution. Effective use of CBCT in presurgical treatment planning leads to decreased risk of complications and increased patient safety, which will help implant practices and clinicians no matter how far along they are in their implant journey.
Dr. Albert (Ace) Goerig discusses the benefits of CBCT to the endodontic practice in his article: https://endopracticeus.com/the-value-of-the-cbct-in-the-endodontic-practice/
References
- Karthik K, Sivaraj S, Thangaswamy V. Evaluation of implant success: A review of past and present concepts. J Pharm Bioallied Sci. 2013;5(suppl 1): S117–S119.
- Parnia F, Fard EM, Mahboub F, Hafezeqoran A, Gavgani FE. Tomographic volume evaluation of submandibular fossa in patients requiring dental implants. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 2010;109(1):e32-e36.
- Karthikeyan I, Desai SR, Singh R. Short implants: A systematic review. J Indian Soc Periodontol. 2012;16(3):302-312.
- Mehta H, Shah S. Management of Buccal Gap and Resorption of Buccal Plate in Immediate Implant Placement: A Clinical Case Report. J Int Oral Health. 2015;7(suppl 1):72-75.
- Kim, GS., Lee, JW., Chong, JH. et al.Evaluation of clinical outcomes of implants placed into the maxillary sinus with a perforated sinus membrane: a retrospective study. Maxillofac Plast Reconstr Surg. 2016;38(1):50.
- Verardi S, Pastagia J. Obliteration of the nasopalatine canal in conjunction with horizontal ridge augmentation. Compend Contin Educ Dent. 2012;33(2):116-20, 122.
Stay Relevant With Endodontic Practice US
Join our email list for CE courses and webinars, articles and more..

 Dr. John Pasicznyk practices at Britely Implant Studios in Naples, Florida. A 2010 graduate from Indiana University School of Dentistry, he built a group of technology-focused general dental practices before transitioning into owning his implant-only practice. A leader in digital implant dentistry, his mission is to provide the highest quality of care to his patients using the latest technology and innovative techniques. As a faculty member at 3D Dentists and mentor at Implant Pathways, Dr. Pasicznyk has devoted himself to improving dentists’ lives through education and mentoring on all things implants.
Dr. John Pasicznyk practices at Britely Implant Studios in Naples, Florida. A 2010 graduate from Indiana University School of Dentistry, he built a group of technology-focused general dental practices before transitioning into owning his implant-only practice. A leader in digital implant dentistry, his mission is to provide the highest quality of care to his patients using the latest technology and innovative techniques. As a faculty member at 3D Dentists and mentor at Implant Pathways, Dr. Pasicznyk has devoted himself to improving dentists’ lives through education and mentoring on all things implants.