Dr. Rick Schwartz performed endodontic retreatment and used GentleWave irrigation on five patients who still had symptoms after their initial treatment.
Dr. Rick Schwartz discusses retreatment of five cases with varying outcomes
Abstract
Introduction: The GentleWave® device is claimed to provide more complete irrigation of the root canal system than traditional irrigation methods, potentially resulting in better treatment outcomes. One way to measure the efficacy of a clinical technique or device is to use it to retreat teeth that did not respond to conventional retreatment protocols.
Materials and methods: Retreatment was performed on five patients. In each case, the patients remained symptomatic after initial instrumentation, placement of calcium hydroxide paste in the canals for a month, followed by replacement of Ledermix® paste for approximately 2 months. At that point, the teeth were re-accessed, a GentleWave® (Sonendo®) cycle was run, and the teeth were obturated and restored. The patients were contacted by phone 1 day and 1 week later, and four of the patients attended recall appointments at 6-8 months. The fifth patient was contacted and questioned by phone at 6 months, but declined to attend a recall appointment.
Results: At the 6-month recall, one patient was unchanged, two were improved but not 100%, and two were symptom-free. The results suggest that the GentleWave system may improve the outcome for some patients who remain symptomatic after traditional retreatment methods.
Introduction
Irrigation is considered an important contributor to successful root canal treatment. Traditional endodontic treatment utilizes needle irrigation by hand as the primary method. Many products and devices have been developed in an effort to make the irrigation more effective. One such device is the GentleWave (GW) system (Sonendo).
Many claims have been made by users about the benefits of GW, some of which are supported by published studies. The claims include more thorough cleaning of the root canal system than other methods, high success rates, less postoperative pain than other methods, obturation of more “accessory anatomy” than other methods, and that single-visit treatment is possible for most teeth. Several in vitro studies reported more thorough cleaning of the root canal system in initial treatment.1-6 One study showed no difference.7 Minimal canal preparation is recommended by Sonendo to maintain as much of the tooth’s structural integrity as possible, and GW was shown to effectively clean canals prepared to size 15.04.8 Several case reports demonstrated an abundance of accessory anatomy obturated after irrigation with GW.9,10 GW was shown to be comparable to other methods (although not very effective) at removing remnants of gutta percha and sealer during retreatment.11,12 One in vitro study reported no apical extrusion of irrigant, as opposed to the findings with hand irrigation.13
Studies reported GW sometimes removes obstructions in the canals14,15 including separated instrument segments.16 Several case series report high short-term success rates;17-19 however, there were no control teeth treated for comparison. Two of the case series articles reported minimal18 or no19 postoperative pain, but a prospective, randomized study reported no difference between GW and hand irrigation.20 A common criticism of the GW literature is that the majority of the published studies to date were supported by Sonendo.
There are many obstacles to performing outcome studies in endodontics that are prospective, randomized, and with adequate power to determine the efficacy of treatments, including studies on new irrigation technologies. One method to evaluate potential benefit is to retreat teeth with previous root canal treatment, which has been refractory to traditional methods. The purpose of this case series is to report the findings of five patients who remained symptomatic after initial treatment followed by conventional multi-visit retreatment of at least three appointments. A GW cycle was added at the last appointment, and the teeth were obturated and restored. Follow-ups of at least 6 months were obtained, and the results are reported.
Materials and methods
The five patients in this case series have several things in common. They had received initial treatment within the previous 2 years, and were referred for evaluation because the teeth remained at least mildly symptomatic. Clinical testing was performed on the teeth in the quadrant and opposing quadrant, included biting pressure, percussion, cold, and periodontal probing as well as periapical and bitewing radiographs. Each patient had preoperative CBCT imaging performed as part of the evaluation.
Retreatment was initiated, the obturating material was removed with a combination of rotary instruments and chloroform, patency was obtained, and when the canals were considered to be adequately prepared, calcium hydroxide paste was placed with a Lentulo spiral. The process was essentially the same for each patient. An effort was made to minimize the enlargement of the canals during retreatment. Irrigants included 6% sodium hypochlorite (Clorox®), which was used throughout instrumentation plus 17% EDTA (Pulpdent®) for the last minute. Both irrigants were activated. At the second appointment, about a month later, all five patients remained symptomatic to some degree. The canals received additional instrumentation and irrigation and Ledermix paste (Reimser Pharma Gmbh) was placed. At the third appointment, about 2 months later, they remained at least mildly symptomatic. At this point, they were considered to be “refractory” to traditional treatment. The teeth were re-accessed, and an 8-minute GentleWave cycle was run. The canals were obturated with gutta percha and a bioceramic cement (Brasseler USA®), and the access was restored immediately with a bonded composite restoration.
The patients were called the next day and at 1 week to ask about their symptoms. They were asked if their tooth was completely better (100%), better but not 100%, worse, or the same as before treatment. With one exception, in which the patient declined to return for recall, they were seen again at least 6 months after completion of treatment for evaluation and radiographs. That patient was contacted by telephone.
Case series
Patient 1
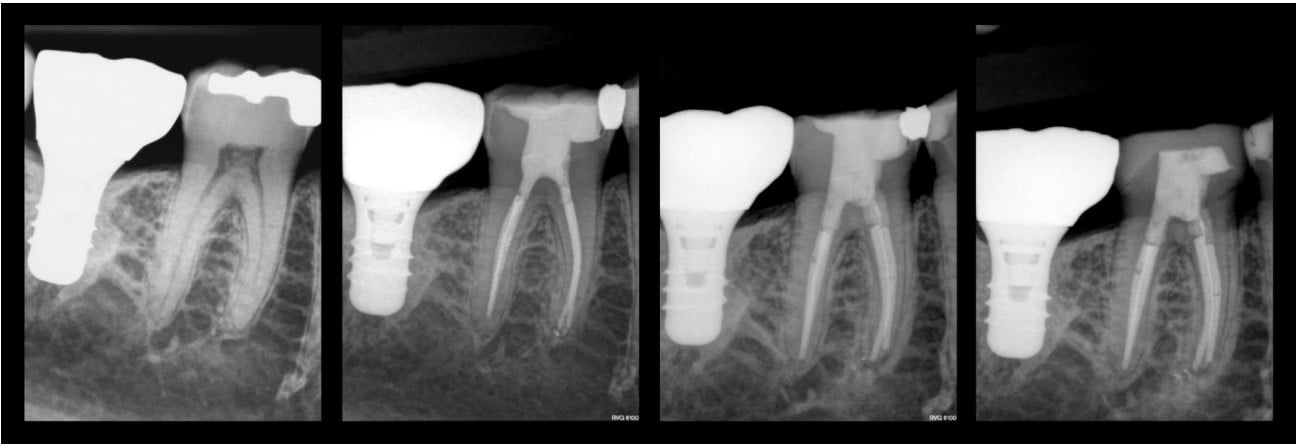
This patient was a 65-year-old white female (Figure 1). She reported allergy to penicillin and had been taking Fosomax® for 2 years, but recently discontinued. She was also taking Premarin®, estradiol, and progesterone for postmenopausal symptoms. She originally presented to the author’s practice for evaluation with spontaneous pain, tenderness, and temperature sensitivity in the right mandible. Testing localized the tenderness to tooth No. 30. It was tender to pressure and percussion, and was hyper-responsive to cold compared to the adjacent teeth, but with minimal lingering. There were no cracks evident with transillumination and no significant periodontal probing. The provisional diagnosis was symptomatic irreversible pulpitis with acute apical periodontitis of unknown etiology. A crack was suspected, even though not visualized externally, based on the shallow restoration.
Root canal treatment of four canals was completed by the author over two appointments with calcium hydroxide dressing for 30 days. The pulp was hyperemic on entry. No cracks were evident internally with the microscope. She was asymptomatic at the second appointment when the tooth was obturated and restored with a bonded composite resin. The tooth was taken out of occlusion at the first appointment in anticipation of a cuspal coverage restoration.
She returned 2 days later with spontaneous pain and tenderness from tooth No. 30. The occlusion was adjusted further, and she was prescribed a Medrol® Dose Pack (Pfizer), which relieved her symptoms.
She was back again 5 months later with spontaneous pain and tenderness. Because of periodic symptoms, she had not had any further restorative treatment on tooth No. 30. Testing confirmed tooth No. 30 was the source of her tenderness. A second CBCT scan indicated there were no untreated canals. The following options were discussed: retreatment, surgery, extraction, or no treatment and live with the symptoms. She opted for no further treatment at that point.
Six months later, she decided she was tired of “living with it.” Four canals were retreated. Calcium hydroxide was placed initially for a month, followed by 2 months of Ledermix. At each appointment, her symptoms had not improved. At the third appointment, a GentleWave cycle was run, the canals were obturated with gutta percha and a bioceramic cement, and the tooth was restored with a bonded composite resin. Once again, no cracks were visible internally. The author spoke to her several times over the succeeding months. She reported she improved after the last appointment, but “not 100%.” She said she chews on the tooth comfortably, but is still “aware of it” when she brushes or pushes on it with her tongue. She had a cuspal coverage restoration placed, and no further treatment is planned.
Patient 2
This 37-year-old white female (Figure 2) had no significant medical issues. She reported her only prescription drug was for birth control and penicillin-caused hives. She presented with spontaneous pain, tenderness, and temperature sensitivity in the left mandible. Testing localized the tenderness to tooth No. 19. The cold sensitivity was localized to tooth No. 18, which was otherwise normal. The crown and RCT No. 19 were completed 2 months earlier by her general dentist. The diagnosis was previous root canal treatment and acute apical periodontitis. CBCT imaging suggested there were no untreated canals. We discussed the options: no treatment, extraction, or retreatment with the possibility of a cracked root. Surgery was not considered. She was younger than usual for a cracked tooth, but had excessive tooth wear for her age. She opted for retreatment. As an initial step, the heavy occlusion on the zirconia crown was adjusted, but after 3 weeks, there was no improvement in her symptoms. It was noted that the mesial and distal contacts were less than ideal.

Retreatment was initiated. No cracks were evident internally. The canals were fully prepared, and calcium hydroxide paste was placed. At 1 month, there was only slight improvement of her symptoms. The tooth was taken completely out of occlusion, the canals received additional instrumentation and irrigation, and were refilled with calcium hydroxide paste. A Medrol Dose Pack was prescribed. The next day the patient reported her tooth felt better, but the steroids made her feel “hot and mean.”
After 2 additional months, she was improved, but some chewing tenderness remained. The canals were further instrumented and irrigated, and Ledermix paste was placed in the canals. After 2 additional months, she noted no additional improvement. The tooth was accessed, a GentleWave cycle was run, the canals were obturated with gutta percha and bio-ceramic cement, and the access opening was restored with bonded composite. The next day she reported she was pain-free, but at 1 week she reported minor symptoms had returned.
At 6-month recall she reported she could chew comfortably on that side, but tooth No. 19 “felt different” than her other teeth. She said she was having no problem living with the minor symptoms. The zirconia crown was not replaced.
Patient 3
This 53-year-old white female (Figure 3) reported a history of hypertension and hyperlipidemia. She was currently taking metoprolol and enalapril.

She presented with asymptomatic chronic apical periodontitis on tooth No. 30. She reported the original RCTs were done about 20 years earlier and had been retreated about 2 years ago. She reported a history of spontaneous pain and tenderness associated with tooth No. 30, but was asymptomatic on the day of her evaluation appointment. The diagnosis was previous root canal treatment and chronic apical periodontitis. CBCT imaging showed the distolingual canal appeared to be untreated. Options presented to the patient were no treatment, extraction, and retreatment. After some discussion, we decided to attempt retreatment.
Retreatment was initiated, and no cracks were observed internally. Three plastic carriers were removed, four canals were instrumented to full length, and calcium hydroxide paste was placed.
At 1 month, she reported periodic mild spontaneous pain, and tooth No. 30 was mildly tender to pressure and percussion. The canals were further instrumented and irrigated, and Ledermix paste was placed.
Two months later, she reported similar symptoms as the previous appointment, although it appeared some regeneration of the bone had occurred based on the periapical radiographs. Access was made, a GentleWave cycle was run, the canals were obturated with gutta percha and bio-ceramic sealer, and the access was restored with bonded composite. She reported no symptoms after a follow-up 1 day later and 1 week later. At 6-month recall, she reported no further symptoms, and there appeared to be additional evidence of healing on the periapical radiographs.
Patient 4
This 73-year-old white female (Figure 4) had knee replacement surgery a year before and was premedicated with amoxicillin per her physician’s instructions. She was taking Prozac® for depression and a “baby aspirin” each day. She presented with biting tenderness in the right mandible. Testing localized the pain to tooth No. 30. The diagnosis was previous root canal treatment and chronic apical periodontitis. The existing RCT was about 2 years old, and she reported periodic pain since it was completed. A scan suggested no untreated canals, but a radiolucency in the apical area of the mesial root was evident. We discussed the options: no treatment, retreatment, extraction, or apical surgery. She opted for retreatment, which was performed over three appointments as described with the previous patients. Her symptoms never improved. Her pain was largely unchanged the day after retreatment was completed, at 1 week and 6 months. She said she was able to chew soft foods on that side, but crunchy foods were a problem. She declined CBCT imaging at the recall appointment, and subsequently had the tooth extracted.

Patient 5
This 71-year-old male (Figure 5) presented with controlled hypertension and hyperlipidemia, and was diagnosed as prediabetic, controlled with diet. The original RCT was performed 6 months earlier by a local endodontist. The canal preparations appeared to be somewhat underprepared and “short,” and the patient had persistent biting pain. Testing indicated tooth No. 30 was the source. The diagnosis was previous root canal treatment and acute apical periodontitis. CBCT imaging indicated no untreated canals. Three options were discussed: no treatment, retreatment, and extraction. He opted for retreatment, which was performed as described with the previous patients over a 3-month period. He remained symptomatic when he presented at the third appointment. As with the others, A GW cycle was run, the canals were obturated, and the tooth was immediately restored. He was pain-free the day after obturation and at 1 week and 6 months. He declined to come in for a 6-month recall, so there is not a recall radiograph available, but he said over the phone he was having no issues, and tooth No. 30 felt the same as his other teeth.

Discussion
This case series provides a low level of evidence because of the small sample size and lack of controls, among other things. Like most case series, it is a starting point that suggests there might be value in performing larger, controlled, randomized studies.
Historically, the author has primarily performed multi-visit root canal treatment, with calcium hydroxide paste placed in the canals for about a month between the first and second appointment. In most cases, teeth were not obturated until all the signs and symptoms were resolved. About twice a month, patients would return for the second appointment with an ongoing problem. They received additional instrumentation and irrigation, and in most cases, Ledermix was placed. Ledermix is a paste containing the antibiotic demeclocycline hydrochloride and a steroid, triamcinolone acetonide. It is currently not sold in the U.S. Most of the time the patients’ symptoms would resolve within a day or two after the Ledermix was placed. The five cases in this series were exceptions, seen over about a 6-month period in 2020.
The author prescribes a Medrol Dose Pack on occasion for patients with severe or persistent pain. It consists of 4 mg methyl prednisolone tablets, which the patient takes in a decreasing dose over 6 days. It generally relieves spontaneous pain and tenderness within a few hours of the first dose. In most cases, in a well-treated tooth, the symptoms don’t return.
The GentleWave system utilizes 3% sodium hypochlorite for the majority of the irrigation cycle followed by a shorter cycle with 8% EDTA. Wang21 showed less erosion of the canal walls when the irrigants were used in this order compared to the reverse order. According to the company, it works best in small canals with minimal preparation (personal communication).
It is interesting to note that all five teeth were mandibular first molars, the most common failures in the author’s practice. Four of the five patients were females.
Of the five teeth in this case series, one patient had no improvement of symptoms after the GW cycle, two patients reported improvement; but their symptoms were not completely resolved at recall, and two resolved completely, to the point that the treated teeth were indistinguishable from their surrounding teeth. It is not certain the improvement was due to the GW cycle, of course. Factors such as time, additional instrumentation, and irrigation may have contributed. Nonetheless, the results suggest that some “refractory” teeth, which don’t respond to conventional retreatment protocols and 3 months of an intracanal dressing, may benefit from the addition of GW irrigation.
Dr. Brian Wells also used GentleWave for endodontic retreatment. Read about how some of his patients benefitted from this technique: https://endopracticeus.com/effective-retreatments-with-the-gentlewave-system/
- Haapasalo M, Wang Z, Shen Y, et al. Tissue dissolution by a novel multisonic ultracleaning system and sodium hypochlorite. J Endod. 2014;40(8):1178-1181
- Ma, Y Shen, Y Yang, Y Gao, et al. In Vitro Study of Calcium Hydroxide Removal from Mandibular Molar Root Canals. J Endod. 2015; 41:553-558.
- Molina B, Glickman G, Vandrangi P, Khakpour M. Evaluation of Root Canal Debridement of Human Molars Using the GentleWave System. J Endod. 2015;41(10):1701-1705.
- Wang Z, Shen Y, Haapasalo M. Root Canal Wall Dentin Structure in Uninstrumented but Cleaned Human Premolars: A Scanning Electron Microscopic Study. J Endod. 2018; 44(5):842-848.
- Choi HW, Park SY, Kang MK, Shon WJ. Comparative Analysis of Biofilm Removal Efficacy by Multisonic Ultracleaning System and Passive Ultrasonic Activation. Materials (Basel). 2019;12(21):3492.
- Zhang D, Shen Y, de la Fuente-Nunez C, Haapasalo M. In Vitro Evaluation by Quantitative Real-Time PCR and Culturing of the Effectiveness of Disinfection of Multispecies Biofilms in Root Canals by Two Irrigation Systems. Clinical Oral Investigation. 2019;23(2):913-920.
- Park SY, Kang MK, Choi HW, Shon WJ. Comparative Analysis of Root Canal Filling Debris and Smear Layer Removal Efficacy Using Various Root Canal Activation Systems during Endodontic Retreatment. Medicina (Kaunas). 20201;56(11):615.
- Zhong X, Shen Y, Jingzhi M, Chen W, Haapasalo M. Quality of Root Filling After Obturation with Gutta-Percha and Three Different Sealers of Minimally Instrumented Root Canals of the Maxillary First Molar. J Endod. 2019;45(8):1030-1035.
- Ford MW. Complex Apical Anatomy Revealed Following Endodontic Treatment of a Maxillary Molar Using the GentleWave System: A Case Report. 2017;7(8):446.
- Pullen RV. Root Canal Treatment of a Maxillary First Molar with an Uninstrumented Fifth Canal: A Clinical Case Report. Int J Dent Hyg. 2017;5(1):219.
- Wright C, Glickman G, Jalali P, Umorin M. Effectiveness of Gutta-Percha/Sealer Removal During Retreatment of Extracted Human Molars Using the GentleWave System. J Endod. 2019;45(6):808-812.
- Crozeta BM, Chaves de Souza L, Silva-Sousa YTC, et al. Evaluation of Passive Ultrasonic Irrigation and GentleWave system as adjuvants in endodontic retreatment. J Endod. 2020;46(9):1279-1285.
- Charara K, Friedman S, Sherman A, et al. Assessment of Apical Extrusion During Root Canal Irrigation with the Novel GentleWave System in a Simulated Apical Environment. Endod. 2016;42(1):135-139.
- Chan R, Versiani M, Friedman S, Malkhassian G, Sousa-Neto M, Leoni G, Silva-Sousa Y Basrani B. Efficacy of Three Supplementary Irrigation Protocols in the Removal of Hard Tissue Debris from the Mesial Root Canal System of Mandibular Molars. J Endod. 2019;45(7):923-929.
- Chen B, Szabo D, Shen Y, et al. Removal of Calcifications From Distal Canals of Mandibular Molars by a Non-Instrumentation Cleaning System: A Micro-CT Study. Endod J. 2020; 46(1):11-16.
- Wohlgemuth P, Cuocolo D, Vandrangi P, Sigurdsson A. Effectiveness of the GentleWave System in Removing Separated Instruments. J Endod. 2015;41(11):1895-1898.
- Sigurdsson A, Le KT, Woo SM, et al. Six-Month Healing Success Rates After Endodontic Treatment Using the Novel GentleWave System: The PURE Prospective Multicenter Clinical Study. J Clin Exp Dent. 2016;8(3):290-298.
- Sigurdsson A, Garland RW, Le KT, Woo SM. 12-Month Healing Rates After Endodontic Therapy Using the Novel GentleWave System: A Prospective Multicenter Clinical Study. J Endod. 2016;42(7):1040-1048.
- Sigurdsson A, Garland RW, Le KT, Rassoulian SA. Healing of Periapical Lesions After Endodontic Treatment with the GentleWave Procedure: A Prospective Multicenter Clinical Study. J Endod. 2018;44(3):510-517.
- Grigsby D Jr, Ordinola-Zapata R, McClanahan SB, Fok A. Postoperative Pain after Treatment Using the GentleWave System: A Randomized Controlled Trial. J Endod. 2020;46(8):1017-1022.
- Wang Z, Maezono H, Shen Y, Haapasalo M. Evaluation of Root Canal Dentin Erosion After Different Irrigation Methods Using Energy-Dispersive X-ray Spectroscopy. J Endod. 2016;42(12):1834-1839.
Stay Relevant With Endodontic Practice US
Join our email list for CE courses and webinars, articles and more..

 Rick Schwartz, DDS, graduated from the University of Minnesota School of Dentistry in 1977 and completed a 2-year general dentistry residency. He did a combination of private practice, teaching, and dental materials research before entering endodontic training in 1996. He has authored over 100 publications and was a cover author on three editions of Fundamentals of Operative Dentistry by Quintessence Publishing Co. He is first author of the book Best Practices in Endodontics, also from Quintessence, and is a cover author of Advanced CBCT for Endodontics. For the past 24 years, he has been in full-time private practice limited to endodontics in San Antonio, Texas. He has lectured extensively in the United States and in 17 other countries.
Rick Schwartz, DDS, graduated from the University of Minnesota School of Dentistry in 1977 and completed a 2-year general dentistry residency. He did a combination of private practice, teaching, and dental materials research before entering endodontic training in 1996. He has authored over 100 publications and was a cover author on three editions of Fundamentals of Operative Dentistry by Quintessence Publishing Co. He is first author of the book Best Practices in Endodontics, also from Quintessence, and is a cover author of Advanced CBCT for Endodontics. For the past 24 years, he has been in full-time private practice limited to endodontics in San Antonio, Texas. He has lectured extensively in the United States and in 17 other countries.
