Editor’s intro: Dr. Brian T. Wells approaches cleaning and disinfecting the root canal system with the GentleWave System for minimal instrumentation in a single appointment. Read about some patients who benefitted from this technique.
Dr. Brian T. Wells discusses a procedure for thoroughly cleaning and disinfecting the root canal system
As endodontists, our job is to be specialists in saving teeth. And making the decision of whether a tooth can be saved is not always black and white. There are essentially three options with previously root canal-treated teeth to consider: orthograde retreatment, surgical retrograde treatment, or extraction. Determining a prognosis with treatment decision should be the first step. Many patients elect to save their tooth despite a guarded or poor prognosis. Particularly when a tooth has had a root canal treatment and is now in need of further assistance, we need to put our diagnostic and treatment skills to the test to properly answer: “Can the patient’s tooth be saved?”
 A retreatment is the least invasive way to save the tooth. My philosophy when it comes to retreatments is to stay conservative, making sure to retain as much structural integrity as possible. Most importantly, it is imperative to ensure adequate cleaning and disinfection of all spaces inside the root canal system where bacteria has reached.
A retreatment is the least invasive way to save the tooth. My philosophy when it comes to retreatments is to stay conservative, making sure to retain as much structural integrity as possible. Most importantly, it is imperative to ensure adequate cleaning and disinfection of all spaces inside the root canal system where bacteria has reached.
All of these aspects of this retreatment philosophy were addressed for me when I integrated the GentleWave® System from Sonendo® into my practice over 3 years ago. In the GentleWave System’s unique mechanism of action, procedure fluids are degassed, and the concentration is adjusted to the optimal level. The fluids are circulated throughout the root canal system and continuously refreshed throughout the procedure. Broad spectrum acoustic energy and vortical flow are induced for maximum debridement and dissolution, which results in unmatched cleaning and disinfection with minimal instrumentation — and in a single visit.
Each of the cases to follow represents a decision point that was not necessarily straightforward — in each case, there was some critical factor to consider, whether it was the amount of bone loss, the size of the post, or amount of dentin initially removed. In each of these cases, retreatment was successful despite a guarded-to-poor prognosis.
Case studies
In the following retreatment case studies, I had to ask myself, What do we do here — extraction, retreatment, or surgery? These cases are just a handful of the 1,000s I have treated using the GentleWave System that have given me a higher level of confidence to pursue retreatments in difficult cases and enable patients to save their natural teeth.
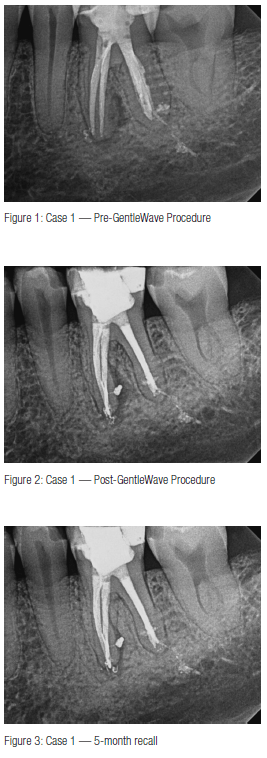
Case 1
45-year-old male
Retreatment on tooth No. 19
This case is not only a retreatment of a retreatment, but also the patient is a periodontist. Tooth No. 19 was retreated by an endodontic colleague 2 years prior. The patient had a persistent draining sinus tract and wanted to save his tooth.
The key challenge in a second retreatment is the degree to which this tooth had been instrumented during its two earlier treatments. Prior treatment appeared to have reached reasonable goals based on radiographic findings. Following prior access, I troughed a fracture on distal wall that did not reach the floor, located the canals, and removed the gutta percha. Upon establishing patency, I realized the importance of cleaning, debriding, and disinfecting the tooth without overinstrumentation any further than it had been previously.
In utilizing the GentleWave® Procedure, I was able to debride and fill a lateral canal on the mesial root, leading to the nidus of the lesion, which gave me a great deal of hope for the future of the tooth. That hope was clearly realized at the 5-month follow-up, where we are able to see near complete bone reformation.



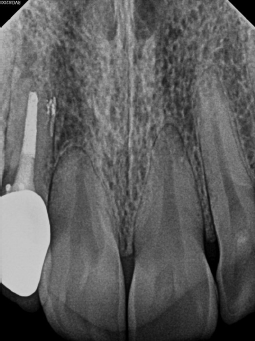
Case 2
59-year-old female
RCT on Tooth No. 7/Retreatment on tooth No. 8
In November 2014, the patient’s dentist noticed a lesion on tooth No. 7 and recommended seeing an endodontist for evaluation. Unfortunately, the patient waited quite a while to follow through on the dentist’s advice. She had undergone RCT on tooth No. 8 2½ years prior and was experiencing intermittent pain. A sinus tract on the palate was drained, and she was given an antibiotic, which relieved her symptoms before coming to see me.
I discussed with her my concern regarding the amount of bone loss, and that extraction or apical surgery may be necessary. The patient, however, was quite eager to save her teeth, so we decided to retreat tooth No. 8 and treat tooth No. 7 — both using the GentleWave System. I also recommended close follow-up to ensure apical healing and determine if apical surgery would still be necessary. Tooth No. 8 was at 2-plus mobility but was not depressible. There was no periodontal communication. Rather than isolate both teeth individually, I isolated the canine and lassoed over to the central. I accessed the tooth, removed the post and all gutta percha from tooth No. 8, utilized the GentleWave Procedure on both teeth, and obturated.
I scheduled follow-up appointments at 1, 3, and 6 months, but she failed to show. She eventually revisited her dentist at 11 months when she began experiencing some discomfort and was referred back to me. As you can see in Figure 6, her pain was not related to any endodontic issues — the alveolar bone had healed remarkably well. I found that the discomfort was related to food impaction, which was easily resolved.




Case 3
46-year-old female
Retreatment on tooth No. 4
This case represents a difficult starting situation with a large post, large apical lesion, and concern of fracture. Surgery does not appear to be a viable option in this case, as a resection would put us right up against the post. For many, extraction would be the most likely course of action.
After removing the post and saving the crown, the GentleWave Procedure was completed. She returned for 3- and 9-month recall, where we can see excellent healing.


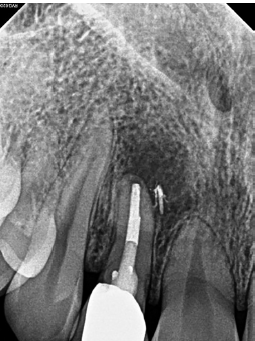

Case 4
23-year-old female
Retreatment on tooth No. 7
There was some additional pressure in this case, as the patient was a dental assistant for one of my referring practices. Prior RCT was completed 8 years prior on tooth No. 7. She started experiencing swelling approximately 6 months before she came to see me. She presented with a buccal draining sinus tract, and probing was at 2 mm-3 mm.
Upon removing the post, the crown fell off, and I saw there was no fracture, but not much tooth structure was left. I discussed extraction, initially, but the patient (and her dentist) wanted to try to save the tooth, so we proceeded to the GentleWave Procedure and finished the case. At the 2-week follow-up, the patient was symptom-free, and the buccal drain was no longer present.
The 9-month follow-up revealed that the lesion had decreased significantly but was still quite prominent. We again discussed the possibility of apical surgery if the tooth did not heal. At 16 months, though, the lesion continued to decrease. At 22 months, we saw a complete bony trabecular pattern — the area had fully healed.
Conclusion
Each of these cases reinforces the need for an effective approach to retreatment, one that preserves the structure of the tooth while still providing thorough cleaning and disinfection. Since integrating the GentleWave System into my practice, I have found that this new technology meets all these criteria.
Prior to using the GentleWave Procedure, all retreatments were treated in two visits. Three years, and thousands of cases into using the GentleWave System, I am no longer surprised when I see rapid and sustained healing, even following complex retreatments, where previously apical surgery or extraction may have been necessary. When we ask: “Can the patient’s tooth be saved?” more often now than before, we are finding that the answer is YES.
Dr. Wells has an interesting practice profile regarding practice philosophy of cleaning and disinfection and other systems he uses. Read about it here.
https://endopracticeus.com/practice-profile/brian-wells-dmd/
Stay Relevant With Endodontic Practice US
Join our email list for CE courses and webinars, articles and more..

 Brian T. Wells, DMD, received his dental degree at Harvard University and completed his clinical training at Tufts University in Boston, where he earned his Endodontic Certificate. Dr. Wells has qualified as a Board Eligible Endodontist with the American Board of Endodontics. He currently maintains a private practice specializing in endodontics in the Tampa, Florida, area.
Brian T. Wells, DMD, received his dental degree at Harvard University and completed his clinical training at Tufts University in Boston, where he earned his Endodontic Certificate. Dr. Wells has qualified as a Board Eligible Endodontist with the American Board of Endodontics. He currently maintains a private practice specializing in endodontics in the Tampa, Florida, area.
