Drs. Romina Chaintiou Piorno, Maribel Rocío Mamani Flores, Eugenia Pilar Consoli Lizzi, Paula Leticia Corominola, and Pablo Alejandro Rodríguez delve into new materials that make treatment of pulp necrosis easier and more successful.
Drs. Romina Chaintiou Piorno, Maribel Rocío Mamani Flores, Eugenia Pilar Consoli Lizzi, Paula Leticia Corominola, and Pablo Alejandro Rodríguez discuss how to treat immature permanent teeth with pulp necrosis
Abstract
Aim
Immature permanent teeth with pulp necrosis pose a challenge for endodontic treatment performance. Calcium hydroxide paste and mineral trioxide aggregate have been used in the apexification treatment of teeth with open apex for a long time. At present, they are replaced by new, biocompatible materials with improved characteristics such as the new generation of hydraulic silicate cements.
Case report
The objective of this paper is to present a case report in which the apical closure of the palatal root in the upper left maxillary first premolar, with an open apex and pulp necrosis, was regenerated by a bioceramic material (Biodentine®). After a 2-year follow-up, the tooth was found to be asymptomatic, and radiographic and computed tomographic studies revealed bone repair and root closure.
Clinical implications
Promotion of apical closure is sought in the treatment of immature permanent teeth that require endodontic treatment. A reasonable and predictive apexification technique with Biodentine can be employed to elicit an apical barrier or a plug promoting tissue regeneration.
Introduction
In several clinical studies, caries and dental trauma have been reported to be the most common cause when assessing the etiology of pulp necrosis.1-3 When pathosis progresses, natural root development of the permanent teeth can be affected, resulting in arrested apical root development and an open apex.4 The complete root development and apical closure of a tooth is estimated to occur 3 years after its eruption;5,6 therefore, it is important to consider the moment the tooth is involved. Several clinical challenges are posed by the endodontic treatment of nonvital immature teeth, with or without periradicular lesion, when the chemomechanical debridement and obturation techniques are performed, due to the thin walls and the presence of an open apex.
In order to maintain these teeth, an intervention focused on the biological or artificial sealing of the delicate apical portion is needed. This treatment is known as apexification7 — “a method to induce a calcified barrier in a root with an open apex or the continued apical development of an incompletely formed root in teeth with necrotic pulps.”8 The apexification with a calcium hydroxide (CH) paste in multiple visits and the single-visit apexification procedure with mineral trioxide aggregate (MTA) are two technically different therapeutic options, being the treatment of necrotic permanent teeth with immature apices their common goal. Today other materials that can be employed to elicit an apical barrier or a plug in a single clinical appointment are available such as hydraulic silicate cements.9 Moreover, revascularization aimed at controlling the infection and promoting continued root development is considered an effective regenerative treatment option for necrotic immature teeth.10,6
Biodentine® (Septodont, Lancaster, Pennsylvania) is a bioceramic material exhibiting adequate handling characteristics with acceptable mechanical and bioactivity properties.11 The single-visit apexification procedure with a bioceramic material is a useful tool to treat teeth in which the apical anatomy is complex due to its amplitude.12 The aim of this paper is to display the clinical management of a first maxillary premolar with a diagnosis of pulp necrosis and an open apex, treated by a single-visit apexification procedure with Biodentine.
Case report
A 10-year-old male patient was referred for endodontic treatment of the maxillary left first premolar. Accompanied by his mother, the patient presented at the Department of Endodontics, School of Dentistry, University of Buenos Aires. Leakage in the composite coronal restoration was noted, and pain on percussion with pain on palpation was revealed during the clinical examination. A sensitivity test to cold was performed with a negative pulpal response. A radiological examination consisted of a preoperative radiograph (Figure 1A). A preoperatory CBCT scan was requested (Figure 1B), which revealed incomplete apex formation and a periradicular radiolucent lesion. The clinical diagnosis of the tooth was pulpal necrosis with a chronic alveolar abscess, and the clinicians decided to perform a single-visit apexification procedure with Biodentine.

Local anesthesia (carticaine hydrochloride 4% L-Adrenaline 1: 100,000, Totalcaína Forte, Bernabó Laboratory, CABA, Argentina) was administered into the buccal vestibule and by palatine before rubber dam application. The coronal restoration of the isolated tooth was removed with a carbide bur in a high-speed handpiece, an access cavity was created, and the canal orifices identified. After scouting, the access was prepared with ProTaper Gold® system SX file (Dentsply Sirona, Tulsa, Oklahoma). Working length was determined with a hand K-File (Dentsply Maillefer, Ballaigues, Switzerland), and an apex locator was utilized and verified with a periapical radiograph (Figure 2A). The canals were chemo-mechanically debrided with further instrumentation with ProTaper Gold S1, S2, F1, F2, and F3 in the buccal canal, while in the palatal canal, the F4 and F5 files were used as well as hand instrumentation with K-Files Nos. 55 and 60. A 2.5% sodium hypochlorite irrigation throughout the entire treatment was used, followed by irrigation with 17% EDTA and then final irrigation with saline. Placement of a rubber stopper 2 mm short of the apical foramen on the files was carefully done during the irrigation process to prevent the solution extrusion and a hypochlorite accident.
After the root canal was dried with sterile absorbent paper points, Biodentine was prepared according to the manufacturer’s instructions and carried into the palatal root canal to be finally condensed with hand pluggers to form an apical plug.

A master cone radiograph was taken (Figure 2B), and condensation of the bioceramic material was verified. A lateral condensation technique with gutta-percha cones and AH-26 sealer (Dentsply Sirona) was performed to finish the obturation. An immediate postoperative radiograph was taken (Figure 2C) in which the obturation quality was observed without extrusion of obturation material periapically.
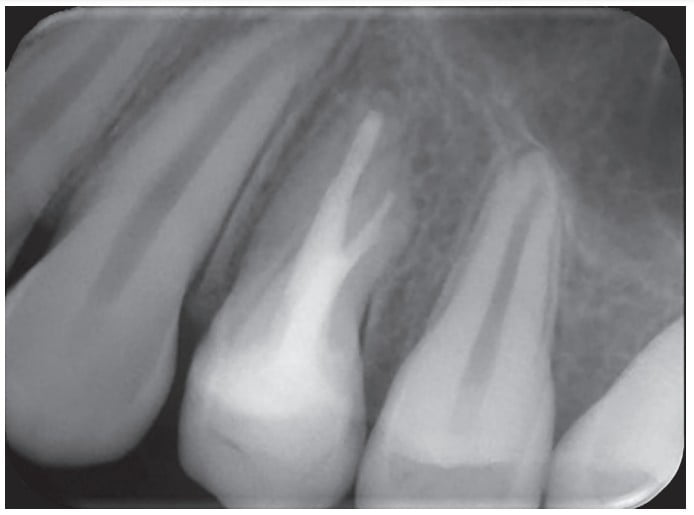
After 12 months (Figure 3), the patient was recalled for a follow-up, and the resolution of the lesion was noted. The treated tooth was also clinically reviewed after 24 months, a periapical radiograph was taken, and the patient presented with a CBCT scan requested by his orthodontist. The tooth remained asymptomatic, and the continuity in the periodontal ligament space with absence of periapical radiolucency was observed (Figures 4A, 4B, and 4C).

Discussion
The objective of endodontics is apical periodontitis prevention and/or elimination,13 and the promotion of apical closure is also sought in the treatment of immature permanent teeth9,14 as has been achieved in the present case report.
It is of utmost importance to seal and prevent bacterial reinfection in the majority of apexification protocols for human immature permanent teeth with apical periodontitis by placing an apical plug.
It is of utmost importance to seal and prevent bacterial reinfection in the majority of apexification protocols for human immature permanent teeth with apical periodontitis15 by placing an apical plug. For many years, calcium hydroxide apexification has been the treatment of choice, although this technique requires many visits, and the weakening of the tooth walls due to long-term use was reported.16 The time between the first visit and the end of treatment varies because multiple visits are needed — a difficult issue to overcome if there is no continuous patient follow-up, along with the presence of a provisional coronal restoration capable of eliciting a root canal reinfection.17,18 Because of these complications, the calcium hydroxide apexification procedure has been replaced by MTA apexification.19 The antibacterial effects of MTA are given by its high pH and the fact that it is biocompatible, induces hard tissue formation, and is slightly more radiopaque than the dentine.20,21
Torabinejad and Chivian22 suggested an alternative apexification to the calcium hydroxide technique. It consisted of cleaning the root canal system and sealing the open apex with MTA in one or two visits to minimize the risk of overfilling and to promote apical repair. The outcomes of a one-step procedure in teeth with open apices and periradicular lesions were assessed by Lin, et al.,23 who concluded that it may be a reasonable and predictable treatment alternative. However, the prolonged setting time, the difficult handling, and possible coronal discoloration associated with MTA20 had led to the search of other materials such as the new generation of hydraulic calcium silicate cements.
Biodentine is a bioactive cement with excellent biological properties as well as good color stability.24 The absence of genotoxicity25 and its low cytotoxicity26 make it an ideal material to be used in endodontic practice. The possible shortcoming of Biodentine is its low radiopacity.27,28
The use of Biodentine as well as MTA in contact with mesenchymal stem cells was suggested by Lee, et al.,28 to induce osteoblast differentiation. The importance of a combination between a specific local biological microenvironment and the circulation of soluble calcium and levels of inorganic calcium to obtain bone regeneration was shown by several studies.29,30 This microenvironment in the presence of calcium-silicate cements is able to induce the apical papilla stem cell and the signaling factors cell differentiation31,32,33 to enhance the apical closure. Just as shown by other case reports with successful long-term resolution,34,9,14 herein the remission of the associated lesion in the radiographic follow-up was observed 1 year after the completion of treatment. Likewise, tissue regeneration and a continuity of the periodontal ligament space, the absence of periradicular radiolucency and the presence of a fine layer of calcified tissue apical to the Biodentine plug were seen in the 24-month follow-up CBCT.
The possible achievement of treatment success by different apexification procedures, even without promoting continued root development leaving thin dentinary walls prone to fracture, is demonstrated by the literature.6,9 Therefore, the development of a therapeutic alternative such as pulp revascularization to enhance continued root formation can be an option.35 However, the decision to perform an apexification procedure in the present case report was sustained on the root development (Nolla 9 stage)5 of the involved tooth.
Biodentine was chosen as a material able to produce apical closure due to its favorable characteristics — namely, a 12-minute initial setting time that enables the completion of the root canal treatment in a single visit and precludes possible root canal system reinfection. Other advantages were its easy handling and working time reduction. Although its radiopacity is low, making radiograph visualization difficult, the adequate seal obtained through the favorable evolution and the achievement of predictable medium-term outcomes are emphasized.
Conclusion
The one-step apexification procedure performed with Biodentine proved to be a versatile option for a tooth with a very wide apex, promoting tissue regeneration.
Drs. Ricardo Machado, Emanuely da Silva Chrun, Luiz Fernando Tomazinho, and Lucas da Fonseca Roberti Garcia wrote about their treatment for pulp necrosis. Read the CE here, and pass the quiz to obtain 2 CE credits! https://endopracticeus.com/ce-articles/endodontic-treatment-of-a-tooth-with-pulp-necrosis-and-severe-inflammatory-external-apical-root-resorption-in-a-single-session-is-it-possible-a-case-report/
- Bender IB. Pulpal pain diagnosis–a review. J Endod. 2000;26(3):175-179.
- Chen MY, Chen KL, Chen CA, et al. Responses of immature permanent teeth with infected necrotic pulp tissue and apical periodontitis/abscess to revascularization procedures. Int Endod J. 2012;45(3):294-305.
- Koç S, Del Fabbro M. Does the Etiology of Pulp Necrosis Affect Regenerative Endodontic Treatment Outcomes? A Systematic Review and Meta-analyses. J Evid Based Dent Pract. 2020;20(1):101400.
- Lauridsen E, Hermann NV, Gerds TA, Kreiborg S, Andreasen JO. Pattern of traumatic dental injuries in the permanent dentition among children, adolescents, and adults. Dent Traumatol. 2012;28(5):358-363.
- Nolla C. The development of the permanent teeth. J Dent Child 1960;27:254-66.
- Flanagan TA. What can cause the pulps of immature, permanent teeth with open apices to become necrotic and what treatment options are available for these teeth. Aust Endod J. 2014;40(3):95-100.
- Timmerman A, Parashos P. Delayed Root Development by Displaced Mineral Trioxide Aggregate after Regenerative Endodontics: A Case Report. J Endod. 2017;43(2):252-256.
- Glossary of Endodontic Terms. Ninth Edition. 2015.
- Vidal K, Martin G, Lozano O, et al. Apical Closure in Apexification: A Review and Case Report of Apexification Treatment of an Immature Permanent Tooth with Biodentine. J Endod. 2016;42(5):730-734.
- Clinical Considerations for a Regenerative Procedure. 2018.
- Domingos Pires M, Cordeiro J, Vasconcelos I, et al. Effect of different manipulations on the physical, chemical and microstructural characteristics of Biodentine. Dent Mater. 2021;37(7):e399-e406..
- Bajwa NK, Jingarwar MM, Pathak A. Single Visit Apexification Procedure of a Traumatically Injured Tooth with a Novel Bioinductive Material (Biodentine). Int J Clin Pediatr Dent. 2015;8(1):58-61.
- Chugal N, Mallya SM, Kahler B, Lin LM. Endodontic Treatment Outcomes. Dent Clin North Am. 2017;61(1):59-80.
- Sharma S, Sharma V, Passi D, et al. Large Periapical or Cystic Lesions in Association with Roots Having Open Apices Managed Nonsurgically Using 1-step Apexification Based on Platelet-rich Fibrin Matrix and Biodentine Apical Barrier: A Case Series. J Endod. 2018;44(1):179-185.
- Holland GR. Periapical response to apical plugs of dentin and calcium hydroxide in ferret canines. J Endod. 1984;10(2):71-4. doi: 10.1016/S0099-2399(84)80040-0.
- Shabahang S. Treatment options: apexogenesis and apexification. Pediatr Dent. 2013 Mar-Apr;35(2):125-8. PMID: 23635980.
- Abbott PV. Apexification with calcium hydroxide–when should the dressing be changed? The case for regular dressing changes. Aust Endod J. 1998;24(1):27-32.
- Rafter M. Apexification: a review. Dent Traumatol. 2005;21(1):1-8.
- Guerrero F, Mendoza A, Ribas D, Aspiazu K. Apexification: A systematic review. J Conserv Dent. 2018;21(5):462-465.
- Parirokh M, Torabinejad M. Mineral trioxide aggregate: a comprehensive literature review — Part III: Clinical applications, drawbacks, and mechanism of action. J Endod. 2010;36(3):400-443.
- Duarte MAH, Marciano MA, Vivan RR, et al. Tricalcium silicate-based cements: properties and modifications. Braz Oral Res. 2018;18;32(suppl 1):e70.
- Torabinejad M, Chivian N. Clinical applications of mineral trioxide aggregate. J Endod. 1999;25(3):197-205.
- Lin J, Zeng Q, Wei X,et al. Regenerative Endodontics Versus Apexification in Immature Permanent Teeth with Apical Periodontitis: A Prospective Randomized Controlled Study. J Endod. 2017;43(11):1821-1827.
- Rajasekharan S, Martens LC, Cauwels RGEC, Anthonappa RP. Biodentine™ material characteristics and clinical applications: a 3-year literature review and update. Eur Arch Paediatr Dent. 2018;19(1):1-22. Erratum in: Eur Arch Paediatr Dent. 2018;15; Erratum in: Eur Arch Paediatr Dent. 2021;22(2):307.
- Vallés M, Mercadé M, Duran-Sindreu F, Bourdelande JL, Roig M. Influence of light and oxygen on the color stability of five calcium silicate-based materials. J Endod. 2013;39(4):525-528.
- Opacic-Galic V, Petrovic V, Zivkovic S, et al. New nanostructural biomaterials based on active silicate systems and hydroxyapatite: characterization and genotoxicity in human peripheral blood lymphocytes. Int Endod J. 2013;46(6):506-16. doi: 10.1111/iej.12017.
- Kaur M, Singh H, Dhillon JS, Batra M, Saini M. MTA versus Biodentine: Review of Literature with a Comparative Analysis. J Clin Diagn Res. 2017;11(8):ZG01-ZG05.
- Lee BN, Lee KN, Koh JT, et al. Effects of 3 endodontic bioactive cements on osteogenic differentiation in mesenchymal stem cells. J Endod. 2014;40(8):1217–1222.
- Tziafas D, Pantelidou O, Alvanou A, Belibasakis G, Papadimitriou S. The dentinogenic effect of mineral trioxide aggregate (MTA) in short-term capping experiments. Int Endod J. 2002;35(3):245-254.
- Gandolfi MG, Shah SN, Feng R, Prati C, Akintoye SO. Biomimetic calcium-silicate cements support differentiation of human orofacial mesenchymal stem cells. J Endod. 2011;37(8):1102-1108.
- Lin NH, Gronthos S, Bartold PM. Stem cells and future periodontal regeneration. Periodontol 2000. 2009;51:239-251.
- Gandolfi MG, Ciapetti G, Taddei P, et al. Apatite formation on bioactive calcium-silicate cements for dentistry affects surface topography and human marrow stromal cells proliferation. Dent Mater. 2010;26(10):974-992.
- Sanz JL, Forner L, Almudéver A, Guerrero-Gironés J, Llena C. Viability and Stimulation of Human Stem Cells from the Apical Papilla (hSCAPs) Induced by Silicate-Based Materials for Their Potential Use in Regenerative Endodontics: A Systematic Review. Materials (Basel). 2020;13(4):974.
- Khetarpal A, Chaudhary S, Talwar S, Verma M. Endodontic management of open apex using Biodentine as a novel apical matrix. Indian J Dent Res. 2014;25(4):513-516.
- Diogenes A, Ruparel NB. Regenerative Endodontic Procedures: Clinical Outcomes. Dent Clin North Am. 2017;61(1):111-125.
Stay Relevant With Endodontic Practice US
Join our email list for CE courses and webinars, articles and more..

 Romina Chaintiou Piorno, DDS, graduated from the School of Dentistry of the University of Buenos Aires in 2012. She then specialized in endodontics at the University of Buenos Aires in 2014. Currently, she serves as Assistant Professor in the Department of Endodontics, School of Dentistry, University of Buenos Aires, Argentine Republic.
Romina Chaintiou Piorno, DDS, graduated from the School of Dentistry of the University of Buenos Aires in 2012. She then specialized in endodontics at the University of Buenos Aires in 2014. Currently, she serves as Assistant Professor in the Department of Endodontics, School of Dentistry, University of Buenos Aires, Argentine Republic. Maribel Rocío Mamani Flores, DDS, graduated from the School of Dentistry of the Cosmos Private Technical University Cochabamba in Bolivia in 2011. She then specialized in endodontics at the University of Buenos Aires in 2021. Now she serves as Assistant Professor in the Department of Endodontics, School of Dentistry, University of Buenos Aires, Argentine Republic.
Maribel Rocío Mamani Flores, DDS, graduated from the School of Dentistry of the Cosmos Private Technical University Cochabamba in Bolivia in 2011. She then specialized in endodontics at the University of Buenos Aires in 2021. Now she serves as Assistant Professor in the Department of Endodontics, School of Dentistry, University of Buenos Aires, Argentine Republic. Eugenia Pilar Consoli Lizzi, DDS, specialized in endodontics and graduated from the University of Buenos Aires in 2017. Currently, she serves as Assistant Professor in the Department of Endodontics, School of Dentistry, University of Buenos Aires, Argentine Republic.
Eugenia Pilar Consoli Lizzi, DDS, specialized in endodontics and graduated from the University of Buenos Aires in 2017. Currently, she serves as Assistant Professor in the Department of Endodontics, School of Dentistry, University of Buenos Aires, Argentine Republic. Paula Leticia Corominola, DDS, graduated from the School of Dentistry at the University of Buenos Aires in 2007. She then specialized in endodontics at the University of Buenos Aires in 2012. She now serves as Associate Professor in the Department of Endodontics, School of Dentistry, University of Buenos Aires, Argentine Republic.
Paula Leticia Corominola, DDS, graduated from the School of Dentistry at the University of Buenos Aires in 2007. She then specialized in endodontics at the University of Buenos Aires in 2012. She now serves as Associate Professor in the Department of Endodontics, School of Dentistry, University of Buenos Aires, Argentine Republic. Pablo Alejandro Rodríguez, DDS, PhD, earned his degree in dentistry from the University of Buenos Aires in 1991. He graduated with the Specialization in Endodontics and the Specialization in Prosthodontics in 2007; he finished his PhD in 2016. Currently, he serves as the Head Professor of the Department of Endodontics and is the Director of the Specialization in Endodontics. Dr. Rodriguez is also Professor of Prosthodontics in the School of Dentistry of the University of Buenos Aires. Dr. Rodríguez is the actual Dean of the School of Dentistry of the University of Buenos Aires in the Argentine Republic.
Pablo Alejandro Rodríguez, DDS, PhD, earned his degree in dentistry from the University of Buenos Aires in 1991. He graduated with the Specialization in Endodontics and the Specialization in Prosthodontics in 2007; he finished his PhD in 2016. Currently, he serves as the Head Professor of the Department of Endodontics and is the Director of the Specialization in Endodontics. Dr. Rodriguez is also Professor of Prosthodontics in the School of Dentistry of the University of Buenos Aires. Dr. Rodríguez is the actual Dean of the School of Dentistry of the University of Buenos Aires in the Argentine Republic.