Drs. Cassandra Wieczerza, Susan Paurazas, and Mazin Askar take a look at endodontic infections and implants and how pathologies can impact treatment planning.
Drs. Cassandra Wieczerza, Susan Paurazas, and Mazin Askar explore the effects of specific periapical pathologies on dental implants
Introduction
The goal of dental implants is to restore the patient’s masticatory function as well as esthetics. To achieve this goal, it is vital to obtain proper osseointegration of the implant and maintain health of surrounding tissues. With a prevalence rate of 19.53%,1 the development of either apical peri-implantitis or retrograde peri-implantitis (RPI) is a concern with long-term success of the dental implant. RPI and apical peri-implantitis are diagnosed by radiographic or cone-beam computed tomography (CBCT) evidence of bone loss in the apical region of an implant, with or without clinical signs. The etiology of these pathologies is an inflammatory response leading to progressive loss of the bone supporting the implant.2 In cases of implant failure related to endodontic infection, two possible etiologies of peri-implantitis are the presence of periradicular lesions of an adjacent tooth and implant placement into a previously infected site.3,4,5,6 A 2016 literature review by Sarmast, et al., found that the most common etiology of RPI was the presence of periradicular periodontitis of an adjacent tooth.7 This discussion and case presentation aims to address the possible effects of adjacent and/or previous periapical pathology on dental implants.
Can endodontic lesions affect adjacent implants?
When treatment planning a dental implant, it is vital to evaluate the pulpal and periapical status of teeth adjacent to the edentulous site. Previous reports have shown cases in which periapical pathology of an adjacent tooth spreads to an otherwise healthy and osseointegrated implant.3,4,8 Whether the periradicular pathology was present at the time of implant placement or developed following placement, one thought is that adjacent pathology can contaminate the implant fixture. If contamination occurs shortly after implant placement, then proper healing and thus osseointegration cannot occur, leading to a failed implant.8 Consequently, the health status of the pulp should always be assessed on teeth adjacent to the implant site. Periapical radiographs alone are insufficient to detect periradicular periodontitis, since 30%-50% of mineral content of bone must be destroyed prior to detection with 2-dimensional imaging.9 Thus, if pulp necrosis or periapical periodontitis is found during clinical or radiographic exam, CBCT should be considered to evaluate the presence and extent of pathology. An integrative review by Costa, et al., provides evidence supporting the superiority in sensitivity and specificity of CBCT over radiographs in evaluating the presence of bone defects around implants. Measurements of detected lesions using CBCT are accurate to a degree of 1 mm when compared to the actual defect.10 Necessary root canal treatment or extraction should be completed prior to implant placement to prevent possible cross-contamination.4
Two important factors when considering adjacent periradicular pathology are the time between the resolution of infection and implant placement and the distance between the infected tooth and implant. Zhou, et al., studied the stability of 128 implants placed adjacent to endodontically treated teeth. Their evidence shows that less than 2 mm between the implant and adjacent tooth increases risk of the RPI. A correlation was also seen between increased success and extending the time between endodontic treatment and implant placement.3
While periradicular lesions of untreated or root canal treated teeth can negatively affect the adjacent implant, this does not mean failure of the implant is imminent. If the infected adjacent natural tooth develops a lesion after implant placement or was not resolved prior to implant placement, efforts must be made to resolve any periradicular pathology as soon as it is detected. A 2019 case series by Sarmast, et al., shows that performing adequate non-surgical root canal treatment of an infected tooth adjacent to an infected implant will allow the complete healing of both.11 Thus, the interdisciplinary relationship between implant surgeons and endodontists is vital to maintain the health of natural teeth as well as dental implants.
Does placing an implant in the site of previous periapical periodontitis affect outcome?
One proposed reason for infections around the implant apex is the placement of said implant in the site of persistent apical periodontitis following endodontic treatment. To investigate this etiology, Saleh, et., al studied the incidence of retrograde peri-implantitis when implants replaced teeth with failed apicoectomy. While not statistically significant, this study showed increased incidence of RPI when implants were placed in sites of persistent apical periodontitis.5 Another study comparing success of implants placed in sites with periapical pathology and those placed in pristine sites found a 98.1% and 98.2% success rate respectfully. They concluded that the difference in survival was not affected by the presence of previous periapical pathology.6
A systematic review by Chrcanovic, et al., also concluded that implants may be immediately placed after extraction of an endodontically or periodontally infected tooth with adequate healing and osseointegration.12 When evaluating implants placed in sites with chronic periapical lesions, one randomized prospective trial showed a 92% success rate with immediate placement. In cases where a 3-month waiting period between tooth extraction and implant placement was observed, the implant success rate increased to 100%; however, this increase was not of significant difference.13
While evidence shows implants are successful when placed in previously infected sites, suggested treatment guidelines should be followed to achieve success. These include thorough debridement of the implant site prior to placement, guided bone regeneration between the bone and implant, and prescribing systemic antibiotics.12,14
Case report
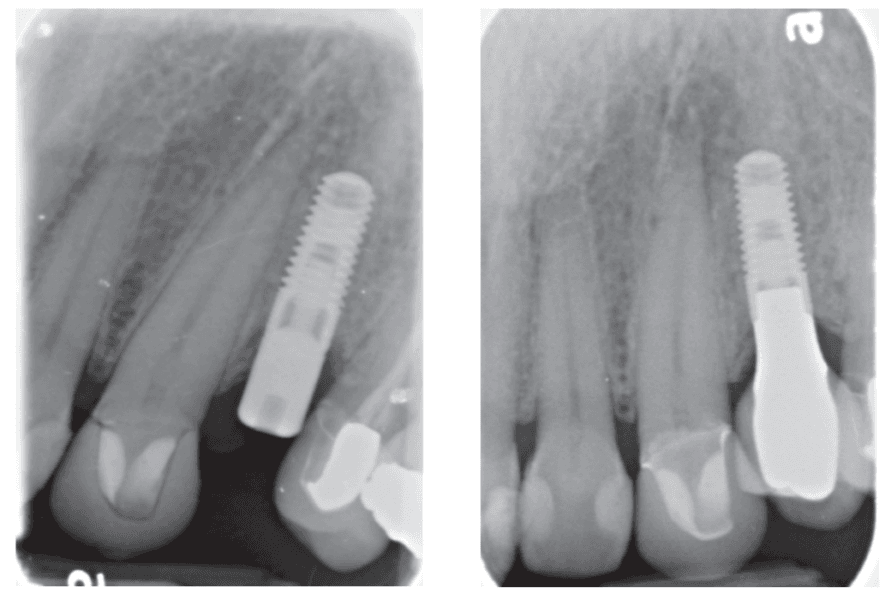
A 48-year-old female patient presented to the graduate endodontic clinic with a referral to evaluate and treat tooth No. 11 through the existing crown. The patient’s chief complaint was, “I was told a year ago I had an infection, but it hasn’t bothered me. They told me I needed a root canal to get rid of the infection.” The patient had no significant health history or any known drug allergies. Dental history for tooth No.11 included multiple restorations followed by a final core and crown in 2019. The adjacent tooth, No. 12, was replaced with an implant in 2018 and restored in 2019, 6 months following final crown of tooth No. 11. Upon examination of records, a periapical radiolucency on tooth No. 11 was visible on the day of crown fabrication and delivery (Figure 1). There was no note of this lesion in the patient’s record. An updated radiograph was taken during a periodic oral exam in September of 2023 showing clear delineation of the periapical radiolucency on tooth No.11 (Figure 2).

Upon presentation to the endodontic clinic, the patient was asymptomatic. Extraoral exam revealed no signs of acute infection and no lymphadenopathy. Intraoral exam showed no signs of acute infection and no sinus tracts. The crown on tooth No. 11 had adequate margins, contacts, and no recurrent decay was detected. Endodontic testing revealed negative responses to cold, percussion, and palpation. Probing depths of tooth No.11 and adjacent implant No. 12 were equal to or less than 3 mm, and no mobility was recorded. Radiographic examination revealed a periapical radiolucency present on the distal aspect of the root apex extending toward implant No. 12. Diffuse calcification in the coronal portion of the canal was observed, and no caries was noted (Figure 3).

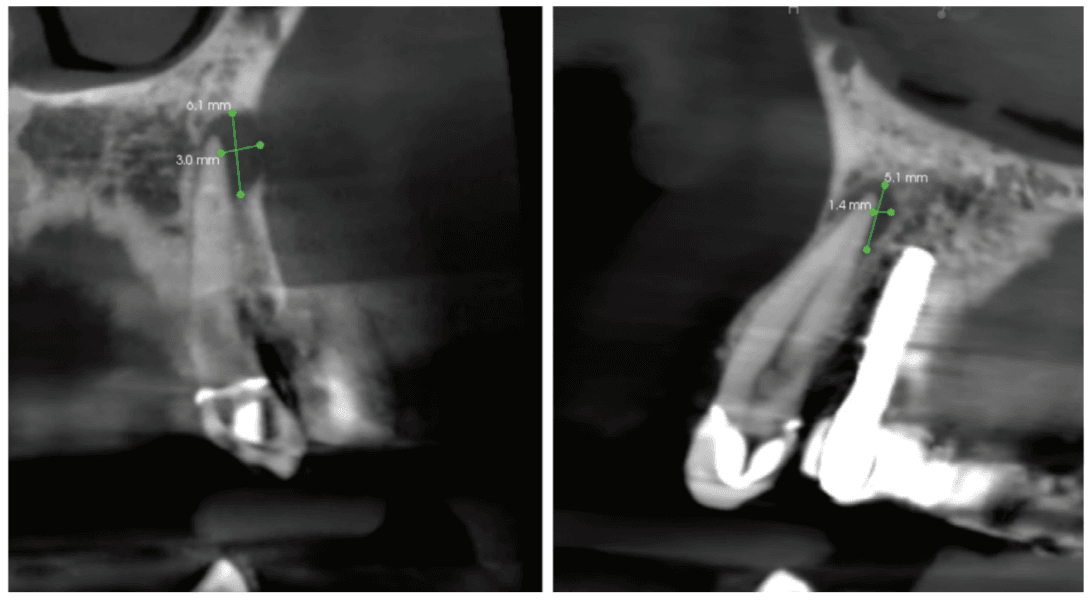
As previous literature has identified the negative effect between periradicular periodontitis of natural teeth and adjacent implants, a limited field of view CBCT (Carestream Dental S 8200 3D, Atlanta, Georgia) was exposed to properly define the periapical radiolucency. Measuring from the apex of tooth No. 11 to a line perpendicular to the long axis of the implant, spacing of 3.4 mm between the two was noted (Figure 4). The recommended amount of space between a natural tooth and dental implant should be 1.5 mm-2 mm, proving adequate spacing in this case.15 Coronal views of the CBCT evaluation revealed a 6.1 mm x 3.0 mm hypodensity extending from the apical and distal aspect of tooth No. 11 (Figure 5A). Sagittal slices revealed the presence of healthy bone morphology between the distal border of the hypodensity on tooth No. 11 and implant No. 12, thus the hypodensity did not extend to the implant (Figure 5B). Reference was made to the Treatment Options for the Compromised Tooth: A Decision Guide published by the AAE in 2017 to determine prognosis.16 In evaluating the coronal tooth structure, tooth No. 11 had a well-fitting crown with adequate margins, no need for crown lengthening, and required only routine endodontic treatment placing it in the favorable category. The periodontal condition of tooth No. 11 was also favorable with probing depths equal to or less than 3 mm and a normal periodontium. Lastly, the apical periodontitis was expected to resolve following non-surgical root canal treatment.16 Thus, tooth No. 11 was diagnosed as pulpal necrosis with asymptomatic apical periodontitis with a favorable prognosis. Nonsurgical root canal treatment was planned, and informed consent was obtained.
Procedure
The patient was anesthetized with topical benzocaine and 3.4mL Septocaine (Articaine hydrochloride 4% and epinephrine 1:100,000) (Septodont, Saint-Maur-Fosses, France) via buccal and lingual infiltration. A rubber dam was placed, and the root canal system was accessed through the crown. Working length was obtained with Root ZX II apex locator (J. Morita, Kyoto, Japan) and verified with a periapical radiograph to be 24 mm. The tooth was then mechanically instrumented with WaveOne® rotary files (Dentsply Sirona, Charlotte, North Carolina) using 10mL of 6% NaOCl throughout the procedure. A final irrigation with EDTA (3mL) and SmartLite Pro EndoActivator™ (Dentsply Sirona, Charlotte, North Carolina) for 1 minute, followed by 6% NaOCl and activator for 1 minute was completed prior to obturation. Obturation was performed with EndoSequence® BC sealer (Brasseler USA, Savannah, Georgia) and gutta percha via continuous wave condensation. EndoSequence BC liner blue (Brasseler USA, Savannah, Georgia) was placed over the gutta percha at the canal orifice, and the tooth was temporized using a cotton pellet and Fuji IX placed in the access (Figure 6). Following completion of the root canal, the patient was scheduled for a 3-month reevaluation and referred to her provider for definitive restoration.
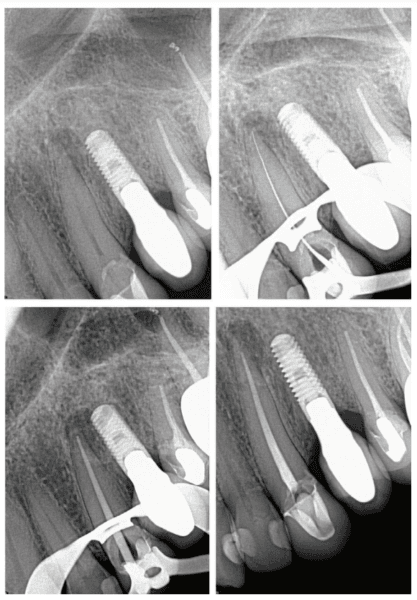

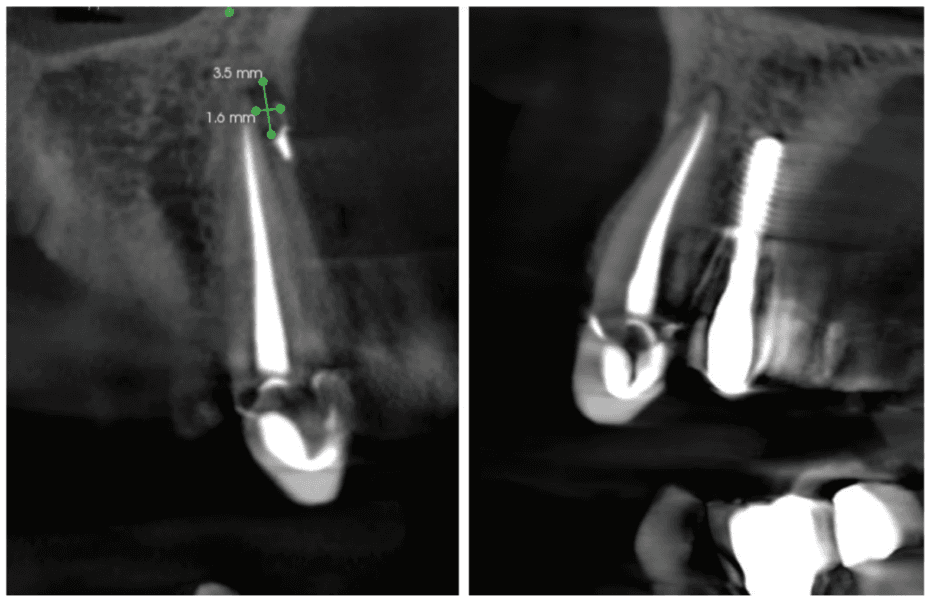
Healing was observed at the 3- and 6-month postoperative visits. Periapical radiographs were exposed at each visit revealing bony healing (Figure 7). The patient reported no pain or symptoms following nonsurgical root canal treatment. At both visits, percussion and palpation were negative. A CBCT was captured at the 6-month postoperative exam to evaluate healing. Coronal CBCT slices revealed a reduction in lesion size to 3.5 mm x 1.6 mm. Sagittal slices also showed reduction in lesion and maintained health of bone surrounding implant No. 12 (Figure 8). A 2011 article by Ng outlines eleven factors that, if present, improve periapical healing following primary non-surgical root canal treatment.17 Only two of these eleven factors, absence of a preoperative periapical lesion and size of the preoperative periapical lesion, were not met in this case report. Along with this and the 2017 AAE Treatment Options for the Compromised Tooth: A Decision Guide article, the final prognosis for healing is favorable.16
Conclusion
Current evidence suggests the risk of an implant developing peri-implantitis is higher when the adjacent tooth has periapical pathology than it is when placed in an extraction site with previous infection. When planning a dental implant, pulp sensibility testing and proper radiographic and, if necessary, CBCT evaluation must be done on teeth adjacent to the implant site prior to placement. When endodontic therapy is indicated, treatment should be completed prior to implant placement. With increased time between root canal therapy and healing of an adjacent periapical lesion and implant placement, a decrease in development of peri-implantitis is expected. It is also important to maintain adequate space of at least 2 mm between the implant and adjacent tooth to help prevent retrograde peri-implantitis. Per the reviewed literature, it can be accepted that the presence of periapical pathology in the planned implant site had no statistical significance in healing when compared to implants placed in pristine sites. Interdisciplinary communication between the implant surgeon and endodontist is key in obtaining long term success of cases when periapical pathology is diagnosed in teeth adjacent to an implant or future implant site. With proper treatment planning, predictable outcomes can be achieved.
Besides the effects on endodontic infections and implants, Dr. Gregori M. Kurtzman discusses other roadblocks to long-term success when deciding between endodontic treatment or implants: https://endopracticeus.com/endodontics-versus-implants-treatment-planning-decisions/
- Diaz P, Gonzalo E, Villagra LJG, Miegimolle B, Suarez MJ. What is the prevalence of peri-implantitis? A systematic review and meta-analysis. BMC Oral Health. 2022 Oct 19;22(1):449.
- Schwarz F, Derks J, Monje A, Wang HL. Peri-implantitis. J Periodontol. 2018 Jun;89 Suppl 1:S267-S290.
- Zhou W, Han C, Li D, Li Y, Song Y, Zhao Y. Endodontic treatment of teeth induces retrograde peri-implantitis. Clin Oral Implants Res. 2009 Dec;20(12):1326-1332.
- Shaffer MD, Juruaz DA, Haggerty PC. The effect of periradicular endodontic pathosis on the apical region of adjacent implants. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 1998 Nov;86(5):578-581.
- Saleh MHA, Khurshid H, Travan S, Sinjab K, Bushahri A, Wang HL. Incidence of retrograde peri-implantitis in sites with previous apical surgeries: A retrospective study. J Periodontol. 2021 Jan;92(1):54-61.
- Fugazzotto P. A retrospective analysis of immediately placed implants in 418 sites exhibiting periapical pathology: results and clinical considerations. Int J Oral Maxillofac Implants. 2012 Jan-Feb;27(1):194-202.
- Sarmast ND, Wang HH, Soldatos NK, Angelov N, Dorn S, Yukna R, Iacono VJ. A Novel Treatment Decision Tree and Literature Review of Retrograde Peri-Implantitis. J Periodontol. 2016 Dec;87(12):1458-1467.
- Sussman HI. Periapical implant pathology. J Oral Implantol. 1998;24(3):133-138.
- Bender IB. Factors influencing the radiographic appearance of bony lesions. J Endod. 1982 Apr;8(4):161-170.
- Costa JA, Mendes JM, Salazar F, Pacheco JJ, Rompante P, Câmara MI. Analysis of peri-implant bone defects by using cone beam computed tomography (CBCT): an integrative review. Oral Radiol. 2023 Jul;39(3):455-466.
- Sarmast ND, Wang HH, Sajadi AS, Munne AM, Angelov N. Nonsurgical Endodontic Treatment of Necrotic Teeth Resolved Apical Lesions on Adjacent Implants with Retrograde/Apical Peri-implantitis: A Case Series with 2-year Follow-up. J Endod. 2019 May;45(5):645-650.
- Chrcanovic BR, Martins MD, Wennerberg A. Immediate placement of implants into infected sites: a systematic review. Clin Implant Dent Relat Res. 2015 Jan;17 Suppl 1:e1-e16.
- Lindeboom JA, Tjiook Y, Kroon FH. Immediate placement of implants in periapical infected sites: a prospective randomized study in 50 patients. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 2006 Jun;101(6):705-710.
- Waasdorp JA, Evian CI, Mandracchia M. Immediate placement of implants into infected sites: a systematic review of the literature. J Periodontol. 2010 Jun;81(6):801-808.
- Liu W, Zhu F, Samal A, Wang HL. Suggested mesiodistal distance for multiple implant placement based on the natural tooth crown dimension with digital design. Clin Implant Dent Relat Res. 2022 Dec;24(6):801-808.
- American Association of Endodontists. Treatment Options for the Compromised Tooth: A Decision Guide. www.aae.org/treatmentoptions.
- Ng YL, Mann V, Gulabivala K. A prospective study of the factors affecting outcomes of non-surgical root canal treatment: part 2: tooth survival. Int Endod J. 2011 Jul;44(7):610-625.
Stay Relevant With Endodontic Practice US
Join our email list for CE courses and webinars, articles and more..

 Cassandra Wieczerza, DDS, earned her doctoral degree at the University of Michigan School of Dentistry in 2016. Upon graduation, Dr. Wieczerza followed her husband to Texas and then Colorado while he fulfilled his commitment with the United States Army. Following this time, Dr. Wieczerza and her family returned to Michigan where she continued her career in general dentistry for an additional 2 years. After 7 years in general practice, Dr. Wieczerza returned to school to pursue a postdoctorate degree in endodontics at the University of Detroit Mercy. She is currently a second-year resident and is eagerly looking forward to her future practice in endodontics.
Cassandra Wieczerza, DDS, earned her doctoral degree at the University of Michigan School of Dentistry in 2016. Upon graduation, Dr. Wieczerza followed her husband to Texas and then Colorado while he fulfilled his commitment with the United States Army. Following this time, Dr. Wieczerza and her family returned to Michigan where she continued her career in general dentistry for an additional 2 years. After 7 years in general practice, Dr. Wieczerza returned to school to pursue a postdoctorate degree in endodontics at the University of Detroit Mercy. She is currently a second-year resident and is eagerly looking forward to her future practice in endodontics. Susan Paurazas DDS, MS, MHSA, is a Clinical Professor and Program Director of Graduate Endodontics at the University of Detroit Mercy School of Dentistry and a Board-certified endodontist. Dr. Paurazas is a speaker at local, regional, and national continuing education courses. Dr. Paurazas has served on multiple committees of the American Association of Endodontists, including the Research and Scientific Affairs committee and is chair of the Educational Affairs Committee. She is actively involved in the American Dental Education Association as chair of the Council of Advanced Education Programs. Dr. Paurazas maintains a private endodontic practice in New Baltimore, Michigan.
Susan Paurazas DDS, MS, MHSA, is a Clinical Professor and Program Director of Graduate Endodontics at the University of Detroit Mercy School of Dentistry and a Board-certified endodontist. Dr. Paurazas is a speaker at local, regional, and national continuing education courses. Dr. Paurazas has served on multiple committees of the American Association of Endodontists, including the Research and Scientific Affairs committee and is chair of the Educational Affairs Committee. She is actively involved in the American Dental Education Association as chair of the Council of Advanced Education Programs. Dr. Paurazas maintains a private endodontic practice in New Baltimore, Michigan. Mazin Askar, BDS, MS, teaches in the Postgraduate Endodontics Residency Program at University of Detroit Mercy School of Dentistry. He has special interest in Microsurgical Endodontics. He received his BDS degree in dentistry from the University of Baghdad, Iraq and a Certificate and Master’s Degree in endodontics from the University of Minnesota. He has received several teaching awards. His areas of interest include microbiology of the root canal system, metallurgy of the root canal file systems, cytotoxicity and genotoxicity of different root canal materials, and tissue reaction to the growth factors.
Mazin Askar, BDS, MS, teaches in the Postgraduate Endodontics Residency Program at University of Detroit Mercy School of Dentistry. He has special interest in Microsurgical Endodontics. He received his BDS degree in dentistry from the University of Baghdad, Iraq and a Certificate and Master’s Degree in endodontics from the University of Minnesota. He has received several teaching awards. His areas of interest include microbiology of the root canal system, metallurgy of the root canal file systems, cytotoxicity and genotoxicity of different root canal materials, and tissue reaction to the growth factors.