Dr. Stuart Segelnick’s harrowing experience with sepsis made him realize the importance of recognizing the condition in the dental office and getting timely care for patients.
Dr. Stuart L. Segelnick describes lifesaving warning signs
A call comes in from an emergency patient soon after you remove a hopelessly infected tooth. Her major concern is having a fever, chills, and feeling downright terrible. She has no difficulty breathing or swallowing, though her mouth still feels swollen. Grace is a middle-aged woman who suffers from diabetes and recently finished chemotherapy for breast cancer. She doesn’t smoke or drink alcohol. Also, she relates getting home too late to pick up the antibiotics that were prescribed. What should she do?
Grace was fortunate to have gone directly to the hospital emergency room and had a CT scan, which didn’t show anything unusual. However, sepsis was suspected, and IV antibiotics were administered. Feeling much better after a night of observation, Grace went home the very next day with a prescription for oral antibiotics.
Untreated or poorly managed periodontal disease, caries, and endodontic and dental alveolar lesions can lead to sepsis. Case reports have been published in dental literature highlighting the morbidity and mortality of dental disease complications. Although rarely reported, post tooth extractions have also been linked to sepsis.1 According to the Centers for Disease Control and Prevention (CDC)2 and the Mayo Clinic,3 bacterial infections are the leading cause of sepsis (viral and fungal infections have also been implicated). When these microbes overwhelm your immune system, your body fights back, causing overt damage to your organs, which may progress to septic shock with the accompanying free fall in blood pressure, organ dysfunction, and ultimate death.
The World Health Organization (WHO) realizes the severity of sepsis and reported that in 2017, sepsis accounted for 20% of all deaths globally. In America, the CDC reports that almost 2 million adults develop sepsis, and 350,000 “die during their hospitalization or are discharged to hospice.” A third of the people who died at the hospital had sepsis during their stay. Even more frightening is that “among adult sepsis survivors, one in three died within a year, and one in six experienced significant, long-term morbidity.”4
Higher risks of acquiring sepsis are found in older people (over 65 years) and children who are under a year old, as well as those inflicted with chronic medical problems, immunocompromised individuals, sepsis survivors, and people recently hospitalized and with severe sickness. Some of the signs and symptoms of sepsis include fever, chills, shivering, sweating, severe pain, fast heart rate, fatigue, hypotension, confusion, and altered mental state.
Tests that your patient’s physician or the hospital will perform if they are suspected of having sepsis include a physical exam, blood cultures, full blood work-up, X-rays, CT scans, and ultrasounds to aid in making a sepsis diagnosis.5 High temperature, elevated heart and respiratory rate, and high white blood cell counts are red flags for sepsis.
Sepsis is considered a medical emergency, and the most important thing you can do is recognize and treat it quickly. Treatment usually includes broad spectrum IV antibiotics, IV fluids, and vasopressors. Monitoring serial lactate measurements is also important. Hospitals must report cases of sepsis to the federal and state government.
According to Mannan, et al., “Early antimicrobial intervention is associated with surviving severe sepsis, making it critical for dentists to understand local factors leading to the crisis and the signs and symptoms of the sepsis-septic shock continuum.”6 In a paper by Sato, et al., the authors stated that “When an oral infection is suspected in an elderly patient, antibiotics should be quickly administered, the patient’s local and systemic state should be confirmed. … If no improvement is observed, medical attention should be quickly sought.”7
Organizations such as END SEPSIS, the Legacy of Rory Staunton (endsepsis.org) and the Sepsis Alliance (sepsis.org) have accomplished amazing work in bringing awareness to the seriousness of sepsis. END SEPSIS has been very successful in advocating for guidelines, regulations, and increasing awareness of sepsis.8 A recent New York Times article by Emily Baumgaertner9 tells how the CDC has developed new guidelines in helping recognize and reduce sepsis in hospitals. The article also highlights that, “In 2013, New York became the first state to mandate that all hospitals adopt sepsis protocols, known as “Rory’s regulations.” Rory Staunton was only 12 years old when he died from undiagnosed sepsis, and his parents started a foundation and the END SEPSIS organization. With these wonderful organizations helping to eradicate sepsis, the future looks promising, so much so that even AIs are now being used to detect sepsis!10
A month after my own gall bladder removal surgery, I had already returned to my office on a lighter schedule when I started feeling very fatigued and had pain in my right back flank. After 3 days of decline and pushing myself through the day, I noticed that my hands had started shaking at the end of a patient examination. At that point, I knew I couldn’t continue and had my receptionist cancel the rest of my appointments.
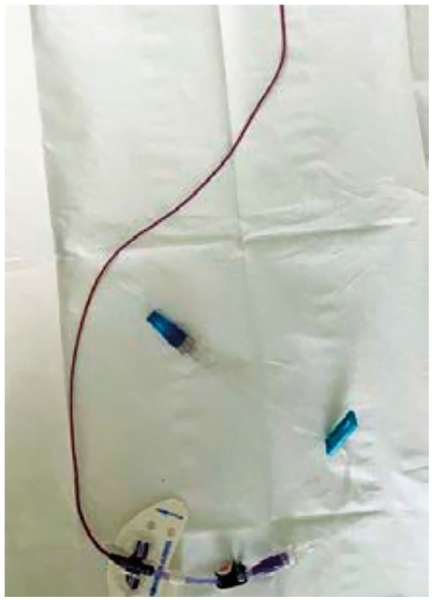
Almost falling asleep at the wheel, I barely managed to drive home. Once home, I made my way to bed and fell right to sleep. At 1 a.m., I awoke bathed in sweat, simultaneously yet uncontrollably shivering and feeling downright awful. I knew something was dangerously wrong. I woke up my wife, and we headed to the hospital ER, where they immediately took my vitals. My blood pressure was extremely low, my heart rate was racing out of control, and my temperature was burning up at 103.3 F. The diagnosis was sepsis! After a CT scan of the abdomen and blood work, I was placed on IV antibiotics. I won’t go into the horrible details of 8 miserable days in the hospital and 4 weeks of IV antibiotics, which were delivered through a picc line (Figure 1) inserted into my arm. I thank G-d every day that I’m alive and able to go back to caring for my family, friends, staff, colleagues, and patients and cherishing every moment I’m still in this beautiful world.
It makes me wonder if I, as a healthcare professional, couldn’t make a timely diagnosis of my own sepsis setting in, how could the average person? Sepsis is a major life-threatening event that dentists must be aware of. Be prepared to advise your patients when sepsis is suspected to head to the hospital ER, because that timely response just might save their lives.
This article was reprinted with permission from the Second District Dental Society of New York (SDDSNY) Bulletin.
Sepsis can cause life-threatening complications, but too much medication is detrimental for other types of dental treatments. Read the “Role of antibiotics in the healing of periapical lesions — two case reports,” by Dr. Amil Sharma and colleagues here: https://endopracticeus.com/role-of-antibiotics-in-the-healing-of-periapical-lesions-two-case-reports/
REFERENCES
- Lee JJ, Hahn LJ, Kao TP, Liu CH, Cheng SJ, Cheng SL, Chang HH, Jeng JH, Kok SH. Post-tooth extraction sepsis without locoregional infection–a population-based study in Taiwan. Oral Dis. 2009 Nov;15(8):602-607.
- Centers for Disease Control. What is Sepsis? https://www.cdc.gov/sepsis/what-is-sepsis.html. Updated August 24, 2023, Accessed February 28, 2024.
- Mayo Clinic. https://www.mayoclinic.org/diseases- conditions/sepsis/symptoms-causes/syc-20351214 Published February 20, 2023, Accessed February 28, 2024.
- World Health Organization. Global Report on the Epidemiology and Burden of Sepsis. https://iris.who.int/bitstream/ handle/10665/334216/9789240010789-eng.pdf?sequence=1. Accessed February 28, 2024.
- Sepsis (Blood Infection): Symptoms and Treatment. https://www.webmd.com/a-to-z-guides/sepsis-septicemia-blood-infection. Reviewed February 1, 2024.
- Mannan S, Tordik PA, Martinho FC, Chivian N, Hirschberg CS. Dental Abscess to Septic Shock: A Case Report and Literature Review. J Endod. 2021 Apr;47(4):663-670.
- Sato H, Tamanoi T, Suzuki T, Moriyama H, Abe S, Yoshida K, Kawaai H, Yamazaki S. Risk Perception of Septic Shock with Multiple Organ Failure Due to Acute Exacerbation of an Infectious Dental Disease. Ther Clin Risk Manag. 2021 Apr 22;17:365-369.
- End Sepsis. About End Sepsis. https://www. endsepsis.org/about/. Accessed February 28, 2024.
- Baumgaertner E. C.D.C. Sets New Standards for Hospitals to Combat Sepsis. https://www.nytimes. com/2023/08/24/health/sepsis-hospitals-cdc.html. Updated September 22, 2023.
- Moor M, Bennett N, Plečko D, Horn M, Rieck B, Meinshausen N, Bühlmann P, Borgwardt K. Predicting sepsis using deep learning across international sites: a retrospective development and validation study. eClinicalMedicine Part of The Lancet. August 2023;62(102124) https://www.thelancet.com/journals/eclinm/article/ PIIS2589-5370(23)00301-2/fulltext. Accessed February 28, 2024.
Stay Relevant With Endodontic Practice US
Join our email list for CE courses and webinars, articles and more..


 Stuart L. Segelnick, DDS, MS, currently serves as editor of the Second District Dental Society of New York Bulletin, the Northeastern Society of Periodontists Bulletin, and is Associate Editor of the New York State Dental Journal. He is a Diplomate of the American Board of Periodontology and International Congress of Oral Implantologists and President-Elect of the Northeastern Society of Periodontists. Dr. Segelnick is an adjunct clinical professor at NYU College of Dentistry Department of Periodontology and Implant Dentistry. He is a Certified Dental Editor (CDE), designated by the American Association of Dental Editors & Journalists, and serves as the association’s liaison to the American College of Dentists. Dr. Segelnick has been recognized multiple times by the International College of Dentists and the American Dental Education Association Gies Foundation for his newsletter production and editorials. He has co-edited five books on dentistry and authored/co-authored multiple scientific articles. He is a fellow of the Pierre Fauchard Academy, the International College of Dentists, and the American College of Dentists. Dr. Segelnick has a private periodontal practice in Brooklyn, New York.
Stuart L. Segelnick, DDS, MS, currently serves as editor of the Second District Dental Society of New York Bulletin, the Northeastern Society of Periodontists Bulletin, and is Associate Editor of the New York State Dental Journal. He is a Diplomate of the American Board of Periodontology and International Congress of Oral Implantologists and President-Elect of the Northeastern Society of Periodontists. Dr. Segelnick is an adjunct clinical professor at NYU College of Dentistry Department of Periodontology and Implant Dentistry. He is a Certified Dental Editor (CDE), designated by the American Association of Dental Editors & Journalists, and serves as the association’s liaison to the American College of Dentists. Dr. Segelnick has been recognized multiple times by the International College of Dentists and the American Dental Education Association Gies Foundation for his newsletter production and editorials. He has co-edited five books on dentistry and authored/co-authored multiple scientific articles. He is a fellow of the Pierre Fauchard Academy, the International College of Dentists, and the American College of Dentists. Dr. Segelnick has a private periodontal practice in Brooklyn, New York.