Drs. Iris Slutzky-Goldberg, Rotem Ophek, Dar Slutzky, and David Keinan treat dens invaginatus conservatively with CBCT imaging.
Drs. Iris Slutzky-Goldberg, Rotem Ophek, Dar Slutzky, and David Keinan explore the use of CBCT, ultrasonics, strict biomechanical preparation, and bioceramics for a specific condition
Abstract
Dens invaginatus is a rare developmental malformation of the tooth that mainly affects the permanent maxillary lateral incisors. Endodontic treatment might be challenging due to the complex canal anatomy of the tooth with the diagnosed invagination. This invagination is often not connected to the main canal, so if it becomes infected, the main canal is usually unaffected. CBCT imaging is necessary to evaluate the complex anatomy and accurately determine the source of the periapical lesion and, thereafter, the treatment plan. The purpose of this article is to describe the careful evaluation of the source of infection by combining data from clinical findings and the use of 3D imaging. The correct obturation material should be selected, and the biomechanical preparation should be adjusted to the complex anatomic irregularities to ensure success.
“In order to visualize the complex anatomy, the use of a CBCT is an essential step. It is especially important to evaluate if there are any separate apical foramina and communications between the main canal and the invagination.”
Introduction
Dens invaginatus (DI), otherwise known as dens in dente, is a dental anomaly that occurs during tooth development and is characterized by an invagination of the enamel organ into the dental papilla before mineralization.1 The distortion of the enamel organ during tooth development can lead to a formation of an enamel-lined canal that ends at the cingulum and in some cases at the incisal edge, producing an irregular coronal shape.2
Dens invaginatus is observed mainly in maxillary lateral incisors, and its prevalence ranges from 0.3% to 10%.1,3 Oehlers (1957) classified dens invaginatus into three types based on the depth of invagination and communication with the periodontal ligament and periradicular tissues. These types range from a minimal Invagination (Type I ) confined within the coronal to an invagination that extends to the root and communicates with the periradicular tissues, either laterally (Type IIIa) or at the apical foramen (Type IIIb).1
Several treatment alternatives have been suggested for the treatment of teeth with Type III DI. These include nonsurgical endodontic treatment of the invagination alone,4 treatment of the main canal alone or along with the invagination, combined orthograde and surgical treatment,5,6 or extraction.
Conventional periapical radiographs, which are the gold standard for identification of DI7 provide only a two-dimensional illustration of the complex anatomy of the tooth7,8 and thus might not yield sufficient information to correctly evaluate the true anatomy of the invagination as well as the main canal.9
Cone beam computed tomography (CBCT) provides a three-dimensional (3D) representation of the tooth.8.9 It enables not only the understanding of the involvement of the main canal in the infection but also whether the invagination is completely separated from the main canal and may allow treatment of the DI without involvement of the main canal.8
The aim of this case report is to present two cases of dens invaginatus, treated by conservative endodontic treatment after a 3-dimensional illustration of the inner anatomy of the tooth using CBCT, ultrasonic, and additional means of improved irrigation.
Case No. 1
A 19-year-old male presented to the endodontic clinic with pain and swelling in the gingiva surrounding his upper left central and lateral incisors. The patient was generally healthy and received endodontic treatment for the maxillary left central incisor following a dental injury 6.5 years ago. A scar of a previous sinus tract was also observed in the oral mucosa. The left lateral incisor was sensitive to percussion and palpation, but positively responded to sensibility testing (Endo-Ice, Coltene). The central incisor did not present any irregular signs or symptoms.
A periapical radiograph demonstrated a DI with an apical radiolucency extending from the mesial aspect of the lateral incisor towards the apex and distal aspect of the central incisor. A slight inclination of the root of the maxillary left lateral incisor was observed in the periapical radiograph.
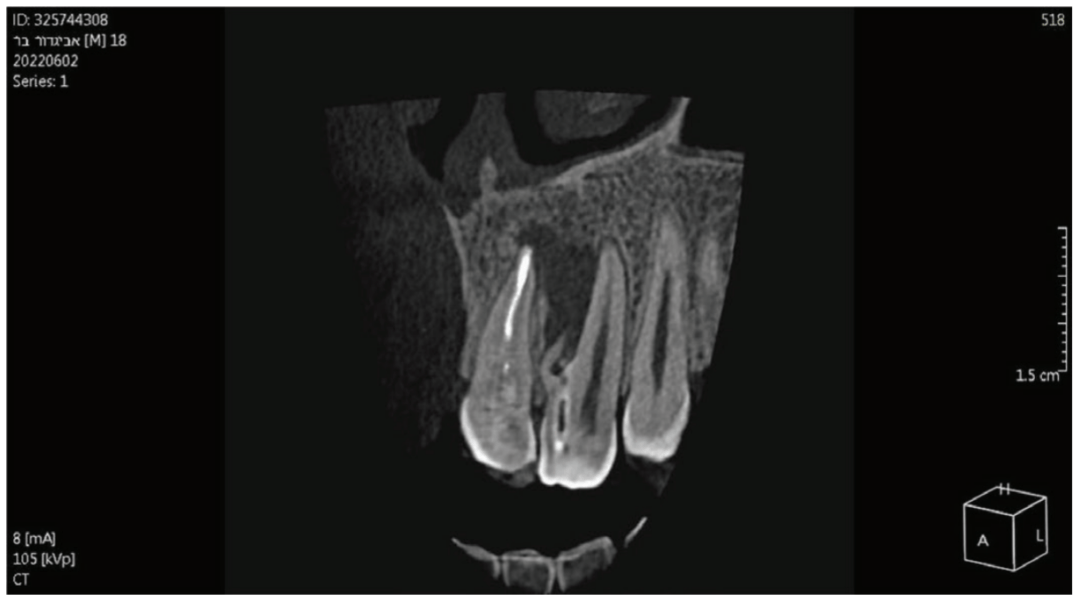
Considering the irregular anatomy of the tooth, the patient was referred for a CBCT scan.
The CBCT scan confirmed the presence of a Type IIIa invagination and a large radiolucent lesion that was associated with the invagination in the lateral incisor and extended mesially towards the apex of the central incisor. Since the apex of the main canal in the lateral incisor was not involved, it was decided to limit the treatment to the invagination. The diagnosis of the periapex of the previously treated central incisor was unclear; there was either periapical healing or asymptomatic apical periodontitis; therefore, no intervention was done, and the tooth was kept for follow-up.
During the first appointment, a palatal access cavity was prepared under a surgical operating microscope based on the external morphology of the tooth and the CBCT scan. After gaining access to the invagination, the enamel-lined canal was conservatively enlarged using an ultrasonic tip. Biomechanical preparation was based on copious irrigation with 2.5% Sodium hypochlorite (NaOCl) and 17% ethylene diamine tetra-acetic acid (EDTA) and the use of the XP Finisher (FKG Dentaire Sarl, La Chaux-de-Fonds, Switzerland). A calcium hydroxide dressing was placed using a spiral Lentulo, and the access cavity was temporized with Coltosol® (Coltene Whaledent) provisional filling material.
At the second appointment (2 weeks later), the patient was asymptomatic. The invagination was irrigated with 2.5% NaOCl and 17% EDTA, and the enamel-lined invagination was obturated with BC Putty (EndoSequence®, BC RRM™ Fast Set, Brasseler). The access cavity was then filled with a Coltosol F® (Coltene Whaledent) and Fuji Equia glass ionomer (GC America) as a temporary filling to seal the access. One week later, it was replaced by a permanent composite restoration.
One year later, the tooth was asymptomatic, with no tenderness to palpation or percussion, and normal mobility was observed. Radiographic examination demonstrated healing of the lesion. Complete healing was observed around the apex of the central incisor, which was symptom-free, and therefore no intervention was necessary for this tooth.
The patient has been scheduled for a follow-up appointment in 1 year.

Case No. 2
An 8.5-year-old girl was referred by her pediatric dentist due to extraoral swelling that extended into the infra-orbital space originating from the left lateral incisor. The immature tooth had only 2/3 of the root completed and therefore was staged as Nolla 8.10 The deciduous lateral incisor was extracted at the age of 2 years after a traumatic dental injury. She was administered Amoxycillin to manage the infection.
Considering the irregular anatomy of the tooth, which was seen in the periapical radiograph, the patient was referred for a small-field CBCT scan. A Class III dens invaginatus was verified. A few days after undergoing emergency treatment, including incision and drainage at the oral surgery department, swelling in the buccal vestibule was still evident upon arrival at the follow-up appointment. Local anesthesia was administered before tooth isolation with a rubber dam. Access cavity was then achieved through the invagination alone, and a transparent liquid leaked from the canal. The invagination was then irrigated with 3% NaOCl and 17% EDTA, dressed with CaOH2, and sealed with a temporary filling material (Coltosol), placed between appointments. Ten days later, at a follow-up appointment, there was still buccal swelling, so similar irrigation and dressing were repeated.
Two weeks later, since there was still swelling, it was decided to treat the main canal as well. The main canal was prepared and irrigated with copious irrigation with 3% NaOCl and 17% EDTA, combined with the use of SAF (Redent Nova, Raanana, Israel) owing to its ability to adapt three-dimensionally to the shape of the canal, and its continuous flow of irrigant through its hollow file, which facilitates better cleaning and debridement. Dressing of the invagination and the main canal were done with a slurry of calcium hydroxide (Ca(OH)2). This step led to the resolution of the swelling; therefore, at the next appointment, it was decided to obturate the canals with Biodentine® (Septodont), and the access cavity was filled with a composite resin.
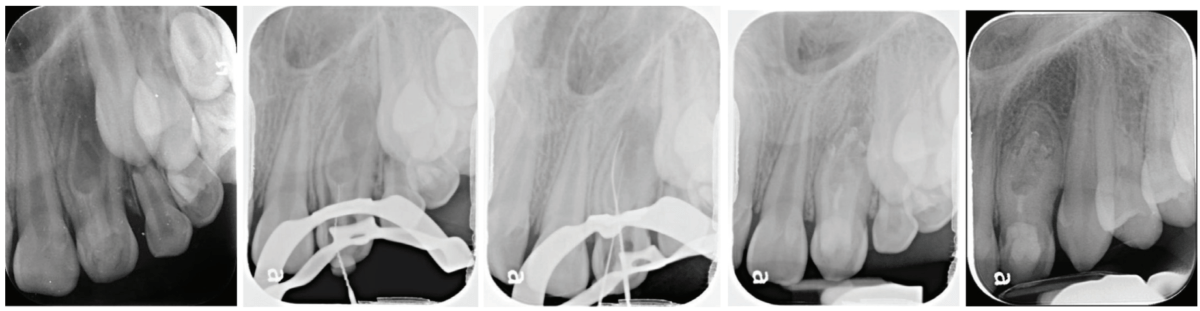
Follow-up examinations were scheduled for 6 months and then yearly. At the 3-year follow-up, complete healing was observed; continuous PDL was observed around the root and resolution of the periapical lesion. The immature root canals continued to develop, and apical closure is evident in the periapical radiograph.
Discussion
Dens invaginatus is a relatively common anatomical aberration mainly found in the maxillary lateral incisors with a prevalence up to 10%.1,3 The invagination can be a simple enamel fold in the coronal or a complex anatomy with a separate communication to the periapical area.1 Diagnosing the source of infection and planning treatment for this complex anatomy can be challenging. A careful diagnosis is necessary to determine whether to treat the invagination alone, the main canal or both.4 Moreover, in certain cases, additional surgical intervention may be required after the orthograde endodontic treatment5 and even intentional replantation.6
In order to visualize the complex anatomy, the use of a CBCT is an essential step.8,9 It is especially important to evaluate if there are any separate apical foramina and communications between the main canal and the invagination.8 This data should be evaluated in conjunction with clinical signs like swelling, sinus tract location and response to thermal tests.11 The use of high magnification and proper lighting is mandatory during access cavity preparation, negotiation of complex canal anatomy, and, if needed, during endodontic microsurgery.12 The use of a guided splint was also reported for the conservative pulp access during endodontic treatment of dens invaginatus.13
The two cases described were treated by a strict protocol for biomechanical preparation. The initial access cavity preparation includes penetration into the invagination using a small file, and then gradual enlargement with ultrasonic tips. Thereafter, copious irrigation with both 3% NaOCl and 17% EDTA, combined with the use of rotary file systems facilitates better availability of the solutions throughout the canal system.14,15 Irrigation with sodium hypochlorite and dressing with Ca(OH)2 are required to dissolve any necrotic tissue in the canals, or any isthmi and cul de sacs.16,17 In the first case, additional debridement and finishing were performed using the XP finisher files (FKG Dentaire Sarl, Switzerland),18 and in the second case, the self-adjusting file system (Redent Nova, Raanana, Israel) was used.19 Both file systems allow for more effective disinfection of the complex canal system with minimal tooth structure removal.20
During canal obturation, we used a bioceramic material to treat the invagination, similar to that of open apices,21 or for root perforation repair.22 The material is known for its excellent sealing ability and biocompatibility, which has made it widely used clinically.23 The high success rate of this material can be attributed to its antimicrobial properties, which result from its high pH during setting.24,25 The use of BC putty, with its higher radiopacity, allows for easy evaluation of radiographic sealing, whereas it may be more challenging with Biodentine due to its similar radiopacity to dentin.25
Conclusion
This article outlines the essential steps for the successful evaluation and treatment of a tooth diagnosed with type III dens invaginatus. These steps include the use of a 3D imaging, ultrasonic access cavity preparation, strict biomechanical protocol and dressing, and then obturation with a bioceramic material. Further study is recommended to evaluate the effect of a revascularization protocol as an alternative treatment option for those teeth.
To read more on treating dens invaginatus, read “Nonsurgical endodontic treatment of a maxillary central incisor diagnosed with infected dens invaginatus (Oehlers’ Type III) and apical periodontitis” by Drs. Jorge Vieyra and Fabian Acosta. Subscribers can take the quiz and receive 2 CE credits! https://endopracticeus.com/ce-articles/nonsurgical-endodontic-treatment-of-a-maxillary-central-incisor-diagnosed-with-infected-dens-invaginatus-oehlers-type-iii-and-apical-periodontitis/
- Alani A, Bishop K. Dens invaginatus. Part 1: Classification, prevalence and aetiology. Vol. 41, Int Endod J. 2008;41(12): 1123-1136.
- Hülsmann M. Dens invaginatus: Aetiology, classification, prevalence, diagnosis, and treatment considerations. Int Endod J. 1997;30(2):79-90.
- Siqueira JF Jr, Rôças IN, Hernández SR, Brisson-Suárez K, Baasch AC, Pérez AR, Alves FRF. Dens Invaginatus: Clinical Implications and Antimicrobial Endodontic Treatment Considerations. J Endod. 2022 Feb;48(2):161-170.
- Tagger M. Nonsurgical endodontic therapy of tooth invagination. Report of a case. Oral Surg Oral Med Oral Pathol. 1977 Jan;43(1):124-129.
- da Silva Neto UX, Hirai VH, Papalexiou V, Gonçalves SB, Westphalen VP, Bramante CM, Martins WD. Combined endodontic therapy and surgery in the treatment of dens invaginatus Type 3: case report. J Can Dent Assoc. 2005 Dec;71(11):855-858.
- Li N, Xu H, Kan C, Zhang J, Li S. Retrospective Study of Intentional Replantation for Type IIIb Dens Invaginatus with Periapical Lesions. J Endod. 2022 Mar;48(3):329-336.
- Kfir A, Flaisher Salem N, Natour L, Metzger Z, Sadan N, Elbahary S. Prevalence of dens invaginatus in young Israeli population and its association with clinical morphological features of maxillary incisors. Sci Rep. 2020 Oct 13;10(1):17131.
- Patel S. The use of cone beam computed tomography in the conservative management of dens invaginatus: a case report. Int Endod J. 2010 Aug;43(8):707-713.
- Kfir A, Telishevsky-Strauss Y, Leitner A, Metzger Z. The diagnosis and conservative treatment of a complex type 3 dens invaginatus using cone beam computed tomography (CBCT) and 3D plastic models. Int Endod J. 2013 Mar;46(3):275-288.
- Nolla CM. The development of permanent teeth. J Dent Child. 1960;27:254-266.
- Petersson K, Söderström C, Kiani-Anaraki M, Lévy G. Evaluation of the ability of thermal and electrical tests to register pulp vitality. Endod Dent Traumatol [Internet]. 1999 Jun [cited 2022 Jul 20];15(3):127–131. Available from: http://www.ncbi.nlm.nih.gov/pubmed/10530156
- Pecora G, Andreana S. Use of dental operating microscope in endodontic surgery. Oral Surg Oral Med Oral Pathol. 1993 Jun;75(6):751-758.
- Mena-Álvarez J, Rico-Romano C, Lobo-Galindo AB, Zubizarreta-Macho Á. Endodontic treatment of dens evaginatus by performing a splint guided access cavity. J Esthet Restor Dent. 2017;29(6):396-402
- Caron G, Nham K, Bronnec F, Machtou P. Effectiveness of different final irrigant activation protocols on smear layer removal in curved canals. J Endod. 2010 Aug;36(8):1361-1366
- Haapasalo M, Shen Y, Wang Z, Gao Y. Irrigation in endodontics. Br Dent J. 2014 Mar;216(6):299-303.
- Slutzky-Goldberg I, Hanut A, Matalon S, Baev V, Slutzky H. The effect of dentin on the pulp tissue dissolution capacity of sodium hypochlorite and calcium hydroxide. J Endod. 2013 Aug;39(8):980-983.
- Hasselgren G, Olsson B, Cvek M. Effects of calcium hydroxide and sodium hypochlorite on the dissolution of necrotic porcine muscle tissue. J Endod. 1988 Mar;14(3):125-127.
- Villalta-Briones N, Baca P, Bravo M, Solana C, Aguado-Pérez B, Ruiz-Linares M, Arias-Moliz MT. A laboratory study of root canal and isthmus disinfection in extracted teeth using various activation methods with a mixture of sodium hypochlorite and etidronic acid. Int Endod J. 2021 Feb;54(2):268-278.
- Neves MA, Rôças IN, Siqueira JF Jr. Clinical antibacterial effectiveness of the self-adjusting file system. Int Endod J. 2014 Apr;47(4):356-365.
- Sasanakul P, Ampornaramveth RS, Chivatxaranukul P. Influence of Adjuncts to Irrigation in the Disinfection of Large Root Canals. J Endod. 2019 Mar;45(3):332-337.
- Torabinejad M, Smith PW, Kettering JD, Pitt Ford TR. Comparative investigation of marginal adaptation of mineral trioxide aggregate and other commonly used root-end filling materials. J Endod. 1995 Jun;21(6):295-299.
- Main C, Mirzayan N, Shabahang S, Torabinejad M. Repair of root perforations using mineral trioxide aggregate: a long-term study. J Endod. 2004 Feb;30(2):80-83.
- Fischer EJ, Arens DE, Miller CH. Bacterial leakage of mineral trioxide aggregate as compared with zinc-free amalgam, intermediate restorative material, and Super-EBA as a root-end filling material. J Endod. 1998 Mar;24(3):176-179.
- Camilleri J. Staining Potential of Neo MTA Plus, MTA Plus, and Biodentine Used for Pulpotomy Procedures. J Endod. 2015 Jul;41(7):1139-1145.
- Caron G, Azérad J, Faure MO, Machtou P, Boucher Y. Use of a new retrograde filling material (Biodentine) for endodontic surgery: two case reports. Int J Oral Sci. 2014 Dec;6(4):250-253.
Stay Relevant With Endodontic Practice US
Join our email list for CE courses and webinars, articles and more..

