Editor’s intro: Drs. Trent Lally and Kent Sabey show an emergent situation, when intentional replantation and an unusual storage medium resulted in retention of a tooth.
Drs. Trent Lally and Kent Sabey discuss an unusual treatment for an urgent procedure, while using a nontraditional storage medium
Abstract
Background
Unusual cases occasionally present where there may be several suitable treatment options. In this case, a 38-year-old female developed significant periapical disease, either persistent or secondary to previous endodontic treatment, where a
considerable amount of obturation material had been extruded well beyond the root confines.
Case report
Intentional replantation was selected as a treatment option and carried out in traditional fashion, albeit with a few departures. Those included the choice of this procedure as an urgent treatment modality, use of an easy-to-obtain Pedialyte® solution as a PDL cell preservation medium, the use of sutures alone to support the tooth after replantation, and the removal of an existing crown to accommodate significant occlusal interferences and masticatory discomfort several days after the procedure. Other aspects of the treatment were typical of an intentional replantation case, including root resections, root-end preparations, and root-end fillings with mineral trioxide aggregate.
Clinical implications
The outcome of the case was the retention of an asymptomatic, fully functional, properly restored molar, with evidence of periradicular tissue healing, and having met the patient’s expectations.
Background
Endodontics plays a crucial role in maintaining good oral health by eliminating both infection and pain, ultimately preserving the patient’s natural dentition. Resolution of endodontic disease and the resultant pain relief may contribute to an improved quality of life. Though modern tooth replacement procedures such as implants can be very effective, it is very difficult to truly “replace” a patient’s own natural tooth. Additionally, costs associated with dental implants and their restoration may be prohibitive to those with limited financial resources.
Modern endodontics enjoys high success rates. Root canal therapy, root canal retreatment, and periradicular surgery have shown success rates ranging from 86% to 96%.1,2,3,4 Unfortunately, even for the most experienced and skilled clinician, there are times when root canal therapy, root canal retreatment, or endodontic surgery has failed and is not feasible or even predictable, and other options must be considered. One such is intentional replantation.
Intentional replantation is defined as the removal of a tooth and its almost immediate replacement, with the object of preparing and obturating the canals apically while the tooth is out of the socket.5 Though many consider intentional replantation as a procedure of last resort, others have argued that it should be considered equally along with periapical surgery and retreatment. Success rates have been reported in the ranges of 81% and 95%.6,7 Indications for intentional replantation follow:
- intracanal obstructions that cannot be bypassed
- anatomical factors that contra-indicate root-end surgery
- resorption present in an anatomical area not amenable to surgical access
- aberrant, unnegotiable root canal anatomy
- overextension of an excess amount of root canal filling material
- situations where apical surgery would lead to damage to adjacent roots or unacceptable periodontal defects
- a patient who will not consent to potential complications associated with traditional root-end surgery such as persistent paresthesia.
Contraindications to intentional replantation follow:
- a medical history that precludes a surgical procedure
- a non-restorable tooth
- advanced periodontal disease
- missing septal bone
- extremely divergent or curved roots that predispose the tooth to fracture during extraction
- a patient who is unwilling to consent to a guarded prognosis
- a patient who is not likely to comply with requirements associated with the procedure8
When intentional replantation is selected as the treatment of choice for a tooth, it is imperative the procedure be completed while minimizing extra-alveolar time. A successful outcome is heavily dependent on the maintenance of the vitality of the periodontal membrane tissues.5 Mechanisms to achieve this include avoiding or minimizing trauma to the cemental covering of the root; maintaining a moist and physiologically compatible environment during the extra-oral period; minimizing extra-oral time of the tooth; proper splint rigidity; and appropriate splinting duration.8
The purpose of this report is to share details of a case where intentional replantation was undertaken as an urgent procedure, due to acute pain. The unusual presenting nature of this case and the selected treatment option led to some variance from traditional methods. One clear example was the utilization of unflavored Pedialyte electrolyte solution, in maintaining the viability of the periodontal membrane. Specifics of the case management and outcome will be presented.
Case report
A 38-year-old Caucasian female patient had root canal therapy completed on the maxillary right second molar tooth (tooth No. 2) 6 years prior to our involvement with the case. Following that, the crown had been adjusted several times to relieve persistent discomfort. Two months prior to her visit to our office, the pain had become intolerable, and she was referred to an oral and maxillofacial surgeon for extraction of the tooth. During evaluation by the surgeon, the patient expressed a desire to save her tooth, and she was subsequently referred to our endodontic practice for evaluation.
Both medical and dental histories were reviewed. Significant medical history included hypertension, which was managed with 12.5 mg of hydrochlorothiazide taken once daily. The patient reported a Type I penicillin allergy. The extraoral and intraoral examinations, including oral cancer screening, were unremarkable. There was no evidence of any swelling or sinus tracts. Pulp testing showed normal responses to cold by teeth Nos. 3 and 4, with no response by tooth No. 2. Tooth No. 2 was moderately tender to both percussion and palpation, while others in the sextant were non-tender. All teeth in the sextant exhibited physiologic mobility. Probing depths ranged from 3 mm-4 mm with slight bleeding on probing. Clinically, there were no caries or defective restorations apparent.
 Radiographically, a well-circumscribed, 5 mm-diameter periapical radiolucency was present. Obturation material was extended beyond the apex of both mesial and distal roots. The distal-buccal root obturation appeared to extend well into the region of the image interpreted as the right maxillary sinus (Figure 1). A CBCT scan was considered. After discussing that the amount of helpful information likely to be attained from the image was minimal and that additional images would not appreciably alter the intentional replantation procedure, coupled with the patient’s financial concerns, that option was deferred.
Radiographically, a well-circumscribed, 5 mm-diameter periapical radiolucency was present. Obturation material was extended beyond the apex of both mesial and distal roots. The distal-buccal root obturation appeared to extend well into the region of the image interpreted as the right maxillary sinus (Figure 1). A CBCT scan was considered. After discussing that the amount of helpful information likely to be attained from the image was minimal and that additional images would not appreciably alter the intentional replantation procedure, coupled with the patient’s financial concerns, that option was deferred.
It was determined that orthograde endodontic retreatment would not be adequate to address the extruded obturation material. Extraction, root-end surgery, and intentional replantation were discussed with the patient as treatment options. Due to the restrictive nature of the patient’s masticatory muscles and vestibular height, it was determined that inadequate access to the operative site would make a root-end procedure unfavorable. Intentional replantation was recommended to the patient. As part of the informed consent process, benefits and risks of the intentional replantation procedure were discussed with the patient. The patient was made aware that the tooth may have already been fractured, which might be visualized once extracted. This would render the tooth unsuitable for replantation. The patient selected intentional replantation as the choice for treatment, with acknowledged understanding that the prognosis for the ultimate retention of tooth No. 2 was “questionable” due to the possibility of either an existing root fracture or a fracture occurring during the treatment. The patient was scheduled for the procedure 2 weeks following that evaluation appointment.
Ten days later, the patient presented to our office for an unscheduled visit, complaining of severe, constant pain associated with the tooth. The tooth exhibited increased mobility and was now depressible in the socket. Due to the degree of acute discomfort, 3.4 ml of 0.5% bupivacaine with 1:200,000 epinephrine were administered via PSA block and infiltration injections to provide the patient pain relief for the evening. The patient was given the following prescriptions: 600 mg ibuprofen (1 tab every 6 hours); 5/325 mg hydrocodone/acetaminophen (1-2 tabs every 6 hours, as needed); 300 mg clindamycin (1 tab every 6 hours for 7 days); and 0.12% chlorhexidine mouth rinse (twice daily intraoral rinse and expectoration of 5 ml, starting morning of procedure until 1 week after suture removal). An appointment time was given to accomplish the intentional replantation the next day.
The patient presented the following day for the procedure. Local anesthesia was obtained via 1.7 ml 4% articaine with 1:100,000 epinephrine (buccal infiltration), 1.7 ml 2% lidocaine with 1:100,000 epinephrine (palatal infiltration), and 1.7 ml 0.5% bupivacaine with 1:200,000 epinephrine (PSA block). The periodontal attachment for tooth No. 2 was released using a No. 12 scalpel blade. The tooth was cautiously (as atraumatically as possible) extracted using a No. 150 forceps and immediately placed into gauze soaked with unflavored Pedialyte oral electrolyte solution in order to maximize maintenance of PDL cell viability. Slight purulent drainage was noted within the extraction socket.
 The two roots were fused into one S-shaped oval root mesial-distally, and what appeared to be gutta percha extended beyond the mesial canal terminus. While holding only the clinical crown, the tooth was inspected under the microscope at high magnification. No fractures were visualized. The root resection was completed using a tapered diamond bur, and 3 mm-deep root-end preparations were completed in both roots using a No. 245 carbide bur. Throughout both these procedures, the entire root surface was constantly bathed and irrigated with the Pedialyte solution by a dental assistant. ProRoot® Gray MTA (Dentsply Sirona) was placed as a root-end filling material in all root-end preparations. During the extraoral procedure time, the socket was continually irrigated by another dental assistant with a gentle flow of sterile saline, to prevent formation of an organized blood clot. All apparent granulomatous, inflamed tissue, and most of the overextended obturation material were removed from the apical portion of the extraction socket with several of the small fragments unable to be visualized or retrieved. There was no apparent exposure of the sinus during the procedure.
The two roots were fused into one S-shaped oval root mesial-distally, and what appeared to be gutta percha extended beyond the mesial canal terminus. While holding only the clinical crown, the tooth was inspected under the microscope at high magnification. No fractures were visualized. The root resection was completed using a tapered diamond bur, and 3 mm-deep root-end preparations were completed in both roots using a No. 245 carbide bur. Throughout both these procedures, the entire root surface was constantly bathed and irrigated with the Pedialyte solution by a dental assistant. ProRoot® Gray MTA (Dentsply Sirona) was placed as a root-end filling material in all root-end preparations. During the extraoral procedure time, the socket was continually irrigated by another dental assistant with a gentle flow of sterile saline, to prevent formation of an organized blood clot. All apparent granulomatous, inflamed tissue, and most of the overextended obturation material were removed from the apical portion of the extraction socket with several of the small fragments unable to be visualized or retrieved. There was no apparent exposure of the sinus during the procedure.
 After a total “out-of-socket” time of 13 minutes, tooth No. 2 was reinserted with slow, minimal pressure into the socket and secured into place with a 5-0 chromic gut “figure-eight” continuous sling suture, extended over the occlusal aspect of the crown. A postoperative periapical radiograph revealed adequate root-end fillings. An ice bag was immediately applied to the area, and both verbal and written postoperative instructions were provided to the patient. She was instructed to comply with the previously prescribed medication regimens. She was to return to the office 3 days later for a follow-up evaluation.
After a total “out-of-socket” time of 13 minutes, tooth No. 2 was reinserted with slow, minimal pressure into the socket and secured into place with a 5-0 chromic gut “figure-eight” continuous sling suture, extended over the occlusal aspect of the crown. A postoperative periapical radiograph revealed adequate root-end fillings. An ice bag was immediately applied to the area, and both verbal and written postoperative instructions were provided to the patient. She was instructed to comply with the previously prescribed medication regimens. She was to return to the office 3 days later for a follow-up evaluation.
The patient was called the evening of the procedure and the following morning. She reported that she was having only minimal discomfort with a very slight puffy feeling, but that she felt “much better.” She returned 3 days later, with no reported changes with her medical status. She indicated she had been compliant with the prescribed medications and that her discomfort was adequately controlled with the ibuprofen. She reported that her severe, constant pain had resolved but had been replaced by a moderate pain when biting. She described tooth No. 2 as occluding in the arch first, causing her discomfort. The suture was removed. To alleviate the occlusal interference and associated discomfort, occlusal adjustment was performed. Ultimately, due to the extent of interference, the existing PFM crown on tooth No. 2 was sectioned and removed, rendering the tooth free from occlusal contact in maximum intercuspation, as well as during any excursive movements. One week later the patient was seen again for a follow-up evaluation and expressed considerably reduced tenderness to biting.
The patient returned for additional evaluations at the 4- and 8-week postoperative intervals. At those appointments, the tooth exhibited acceptable mobility and was non-tender to both percussion and palpation; the patient reported being comfortable during function. There was no sinus tract or swelling present. Radiographic imaging revealed that the periapical radiolucency was diminished in size (Figure 3). At that time, the patient was referred to her general dentist for placement of a new full-coverage restoration.
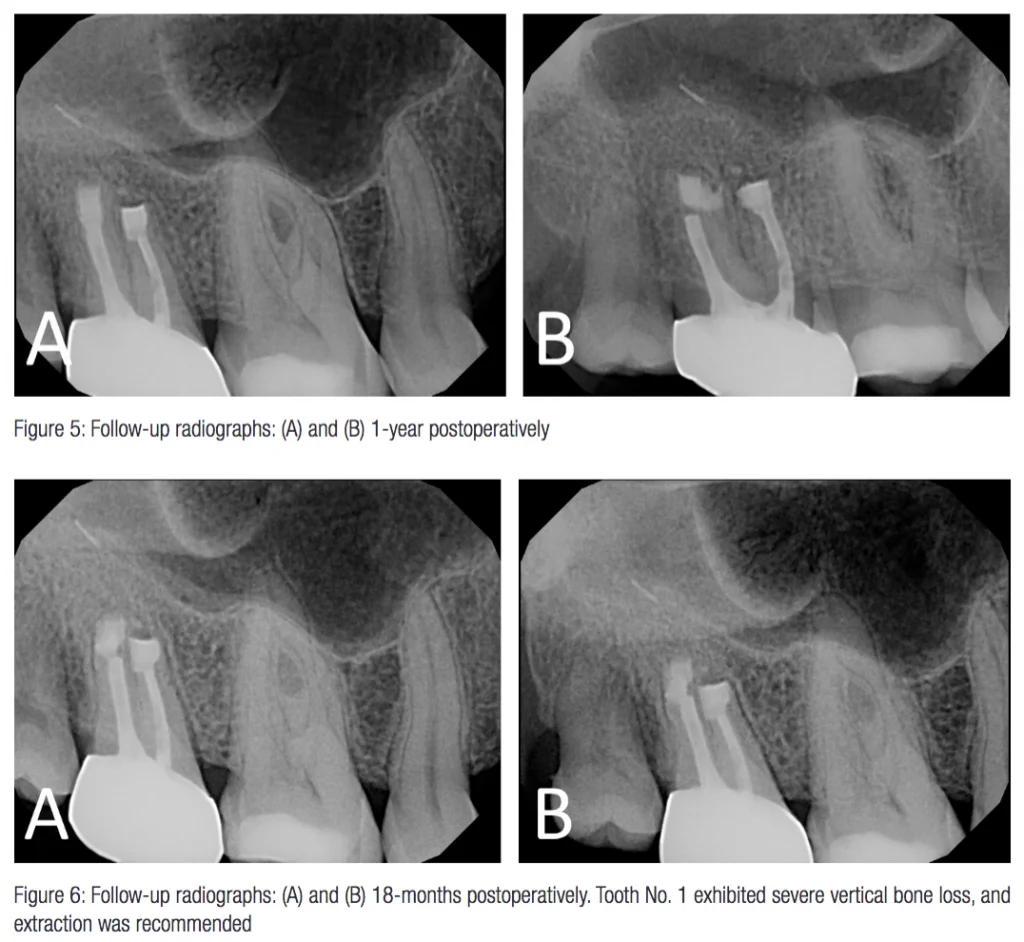
At the 6-month follow-up visit, a new full-coverage gold crown on tooth No. 2 was in place. The tooth remained non-tender to percussion and palpation. The marginal gingiva appeared pink and healthy, with normal probing depths and no bleeding. The tooth exhibited acceptable mobility. Considerable radiographic healing was observed on the radiograph (Figure 4). The patient indicated all associated discomfort had resolved, and the tooth had full normal function. At the 1-year and 18-month follow-up visit, the tooth remained asymptomatic and functional, and complete radiographic healing was present (Figures 5 and 6). Final recall was at 34 months, at which time the tooth remained asymptomatic, functional, and with no abnormal radiographic findings (Figure 7).
Discussion
 The case presented above demonstrates intentional replantation truly as a procedure of last resort, meaning that no other endodontic treatment options were feasible to maintain the tooth and that loss of the tooth was the only other alternative. The patient had limited financial resources, yet she wanted to save her tooth, if possible. The oral surgeon recognized the patient’s desire and referred the patient to determine if any other treatment possibility was feasible.
The case presented above demonstrates intentional replantation truly as a procedure of last resort, meaning that no other endodontic treatment options were feasible to maintain the tooth and that loss of the tooth was the only other alternative. The patient had limited financial resources, yet she wanted to save her tooth, if possible. The oral surgeon recognized the patient’s desire and referred the patient to determine if any other treatment possibility was feasible.
Ultimately, several aspects of the case deviated from typical treatment, the most extreme of which was the use of a nontraditional storage medium. The initial plan was to use Hanks Balanced Salt Solution (HBSS). However, when the patient returned 10 days later in severe pain, the office had not yet received the solution that had been ordered. Though HBSS is commonly recommended, several other solutions have been advocated for encouraging the preservation of PDL cell viability. Most associated studies look at tooth avulsion, though can be applied to intentional replantation (with the goal of maintaining PDL cell viability). Though early studies used sterile or physiologic saline as a medium with high success,5,6 many studies have identified solutions that are less damaging to PDL cells and thus more suitable during intentional replantation.9,10,11 These solutions include skim milk, HBSS, Propolis, and ViaSpan. A more recent study concluded that Pedialyte can also be considered a potential viable alternative as a storage solution for avulsed teeth.12 Aware of these findings, Pedialyte could be quickly acquired at a nearby store, and thus was selected for the procedure. Though more studies are necessary, its use may have elevated the likelihood of a successful outcome.
The procedure was also undertaken during a time of acute inflammation and infection. When the patient initially presented to the office for evaluation, the tooth was much less symptomatic, and we would have preferred to complete treatment under those conditions. However, she returned in severe pain, and clinical findings indicated that she was undergoing an acute exacerbation of symptoms related to the existing periapical disease. No evidence of a fluctuant swelling was noted or other indication of a systemic involvement; thus, an incision for drainage was not performed. Following the intentional replantation procedure, the patient reported complete resolution of her pain that occurred in a reasonably short span of time. This rapid resolution more typically appears following emergency treatment such as an incision for drainage, or cortical trephination. Removal of the tooth as part of the intentional replantation procedure likely served as an avenue to allow adequate drainage.
Stabilization following replantation is recommended to eliminate excess mobility and help with initial PDL healing.13 Physiologic mobility affords the best periodontal healing, and therefore, non-rigid splinting is recommended.14 Postoperative stabilization with an Essix-type retainer was also considered and planned, and would have been the preferred method in this case; however, the general dentist had not yet fabricated the appliance at the time of the patient’s emergency visit. In this case, the tooth was secured into place using a “figure-8” suture across the occlusal surface. This limited degree of splinting likely permitted slight instability of the replanted tooth, resulting in excess mobility of the tooth and resultant premature occlusion for several days. Published reports indicate that traumatic occlusion following surgery in the periodontal tissue may interfere with healing.17 The degree of occlusal interference in this case led to the decision to remove the entire existing crown restoration, as minor occlusal reduction would not have sufficiently relieved the interferences. Given the clinical presentation of this case, other splinting methods mentioned in the literature such as wire and composite, use of acrylic, or placing composite interproximally were not especially appropriate.13 Some even suggest that splinting is not mandatory in all situations.14,15,16
For intentionally replanted teeth, a common cause of failure is resorption, either inflammatory or replacement.17,18 These complications are directly related to the degree of PDL damage that may have occurred during the procedure.19,20 The process in this report was completed while limiting the extraoral dry time to only 13 minutes, lower than the favorable threshold of 20 minutes reported in the literature.21,22 Constant irrigation of the cells throughout the extraoral portion of the procedure with a high volume of favorable medium, such as Pedialyte, could account for adequate survival of these cells.
Another aspect of the case that the patient considered was the cost of treatment. The intentional replantation, even with replacement of the full-coverage crown, was decidedly less expensive than extraction and replacement with a single implant and crown restoration. Potential additional costs were any necessary bone graft and sinus elevation procedures. Publications have investigated the cost-effectiveness of molar endodontic retreatment and root-end surgery as compared with single-tooth implants. They found that a single implant-supported restoration was the least cost-effective option.24 In our endodontic practice, both endodontic retreatment as well as molar root-end surgery would have carried a higher fee than the intentional replantation.
Several authors have proposed criteria to evaluate procedural outcomes. Some propose a 3-year survival interval as successful,25 and some believe that more than 4 years is necessary,23 while others require 5-10 years of follow-up.26,27 Some prefer extended evaluation times owing that posttreatment resorptive processes can occur up to 10 years after the procedure.28 However, other authors share another view,29 that if the tooth meets the typical radiographic and clinical criteria for success — absence of pain, normal function and mobility, healthy periodontium, a decreasing or resolved radiolucency, and absence of resorption — then the case can be considered a success. Interestingly, all these conditions are met in this presented case. The patient was distinctly grateful at being able to retain her tooth, to have resolution of her discomfort, and to enjoy a return of normal dental function.
Conclusion
Despite departures from several traditional aspects of an intentional replantation protocol, biologic principles were creatively and adequately adhered to, allowing the retention of a tooth that had been recommended for removal, accompanied by resolution of significant periapical disease.
Intentional replantation is a possibility after dental trauma and avulsion of a tooth, but many factors must be considered. Read Dr. Meera Patel’s CE article “The management of avulsion and dental trauma” here.
- Sjogren UL, Hagglund B, Sundqvist G, Wing K. Factors affecting the long-term results of endodontic treatment. J Endod. 1990;16(10):498-504.
- Gorni F, Gagliani MM. The outcome of endodontic re-treatment: a 2-yr follow-up. J Endod. 2004;30(1):1-4.
- Rubinstein RA, Kim S. Short-term observation of the results of endodontic surgery with the use of a surgical operation microscope and Super-EBA as root-end filling material. J Endod. 1999;25(1):43-48.
- Rubinstein RA, Kim S. Long-term follow-up of cases considered healed one year after apical microsurgery. J Endod. 1999;28(5):378-383.
- Grossman LI. Intentional replantation of teeth: a clinical evaluation. J Am Dent Assoc. 1982;104(5):633-639.
- Bender IB, Rossman LE. Intentional replantation of endodontically treated teeth. Oral Surg Oral Med Oral Pathol. 1993;76(5):623-630.
- Kingsbury BC Jr, Wiesenbaugh JM Jr. Intentional replantation of mandibular premolars and molars. J Am Dent Assoc. 1971;83(5):1053-1057.
- Fegan S, Steiman HR. Intentional replantation. J Mich Dent Assoc. 1991;73(6):22-24.
- de Souza BD, Bortoluzzi EA, da Silveira Teixeira C, et al. Effect of HBSS storage time on human periodontal ligament fibroblast viability. Dent Traumatol. 2010;26(6):481-483.
- Hiltz J, Trope M. Vitality of human lip fibroblasts in milk, Hanks balanced salt solution, and Viaspan storage media. Endodo Traumatol. 1991;7(2):69-72.
- Blomlöf L. Milk and saliva as possible storage media for traumatically exarticulated teeth prior to replantation. Swed Dent J. 1981;8(suppl 8):1-26.
- Macway-Gomez S, Lallier TE. Pedialyte promotes periodontal ligament cell survival and motility. J Endod. 2013;39(2):202-207.
- Rouhani A, Javidi B, Habibi M, Jafarzadeh H. Intentional replantation: a procedure as a last resort. J Contemp Dent Pract. 2011;12(6):486-492.
- Kratchman S. Intentional replantation. Dent Clin North Am. 1997;41:603-617.
- Morris ML, Moreinis A, Patel R, Prestup A. Factors affecting healing after experimentally delayed tooth transplantation. J Endod. 1981;7(2):80-84.
- Koenig KH, Nguyen NT, Barkhordar RC. Intentional replantation: A report of 192 cases. Gen Dent. 1988;36(1):327-331.
- Harn WM, Chen MC, Chen YHM, Liu JW, Chuyng CH. Effect of occlusal trauma on healing of periapical pathoses: report of two cases. Int Endod J. 2001;34(7):554-561.
- Andreason JO, Hjorting-Hansen E. Radiographic and clinical study of 110 human teeth replanted after accidental loss. Act Odontol Scand. 1966;24(3):263-286.
- Andersson L. Dentoalveolar ankyloses and associated root resorption in replanted teeth. Experimental and clinical studies in monkeys and man. Swed Dent J. 1988;56(suppl):1-75.
- Dryden JA, Arens DE. Intentional replantation. A viable alternative for selected cases. Dental Clin North Am. 1994;38(2):325-353.
- Messkoub M. Intentional replantation: A successful alternative for hopeless teeth. Oral Surg Oral Med Oral Pathol. 1991;71(6):743-747.
- Caffesse RG, Nasjleti CE, Castelli WA. Long-term results after intentional tooth replantation in monkeys. Oral Surg Oral Med Oral Pathol. 1977;44(5):666-678.
- Lu DP. Intentional replantation of periodontially involved and endodontically mistreated tooth. Oral Surg Oral Med Oral Pathol. 1986;61(5):707-709.
- Kim SG, Soloman C. Cost-effectiveness of endodontic molar retreatment compared with fixed partial dentures and single-tooth implant alternatives. J Endod. 2011;37(3):321-325.
- Grossman L, Chacker F. Clinical evaluation and histologic study of intentionally replanted teeth. Transactions of the fourth international conference on endodontics. Philadelphia, University of Pennsylvania.
- Gossman LI. Intentional replantation of teeth. J Am Dent Assoc. 1966;72(5):1111-1118.
- Nosonowitz DM, Stanley HR. Intentional replantation to prevent predictable endodontic failures. Oral Surg Oral Med Oral Pathol. 1982;54:423-432.
- Andreasen JO, Borum MK, Jacobsen HL, Andreasen FM. Replantation of 400 avulsed permanent incisors, 4 Factors related to periodontal ligament healing. Endod Dent Traumatol. 1995;11(2):76-89.
- Emmertsen E. Replantation of extracted molars; preliminary report. Oral Surg Oral Med Oral Pathol. 1956;9(1):115-122.
Stay Relevant With Endodontic Practice US
Join our email list for CE courses and webinars, articles and more..

 Kent Sabey, DDS, following 8 years in an Arizona general dentistry practice, enjoyed a full career in the U.S. Air Force, retiring in January 2011. While in the military, he attended two postgraduate dental training programs — a 2-year AEGD and an endodontics residency, achieving board certification for both areas. Dr. Sabey’s current pursuit is that of a full-time educator, and he serves as the Program Director for the LSU Advanced Education in Endodontics.
Kent Sabey, DDS, following 8 years in an Arizona general dentistry practice, enjoyed a full career in the U.S. Air Force, retiring in January 2011. While in the military, he attended two postgraduate dental training programs — a 2-year AEGD and an endodontics residency, achieving board certification for both areas. Dr. Sabey’s current pursuit is that of a full-time educator, and he serves as the Program Director for the LSU Advanced Education in Endodontics.