Dr. Judy McIntyre shows how cracked teeth and craze lines can be detected for more informed treatment planning decisions.
Dr. Judy McIntyre discusses detection and treatment of teeth with cracks or craze lines
Occlusal forces and time, especially with existing restorations, can cause craze lines and microfractures in the dentition, much like the one in Figure 1. When these small craze lines and infractions propagate with continued use and wear, cracks can develop in teeth. Older amalgam restorations that have been in patients’ mouths for several decades are giving way after years of use. This can be clinically evident often with stained craze lines or marginal ridge cracks.
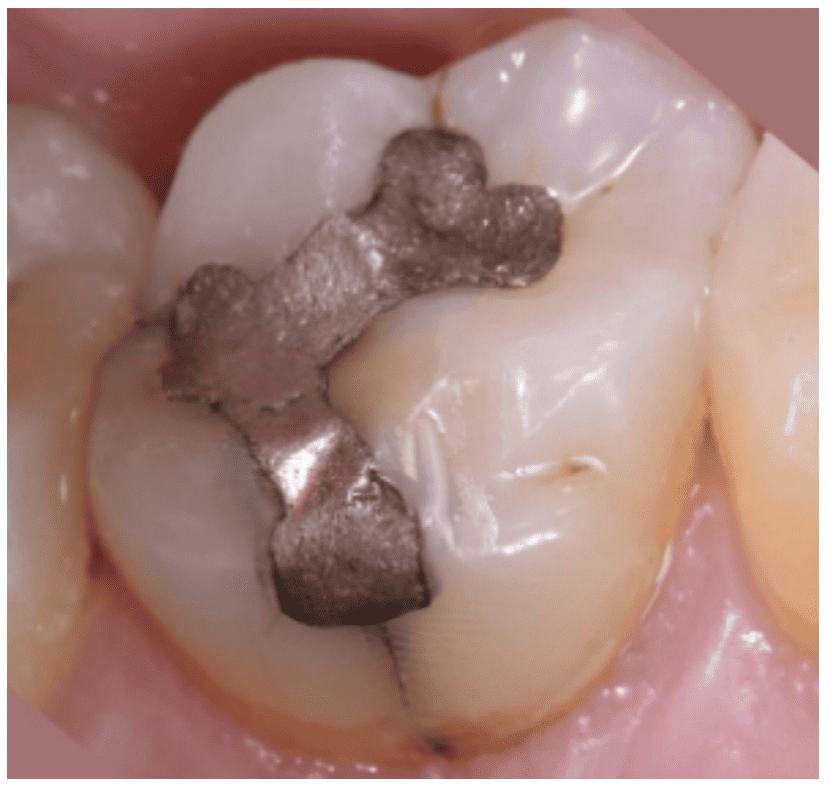 Figure 1
Figure 1
When these craze lines propagate farther – below the CEJ – the term crack is appropriately coined, and often, the tooth may become symptomatic with pulpal involvement. As cracks propagate, many patients may report biting sensitivity, which may eventually lead to cold sensitivity: often the first sign and symptom of pulpal involvement. Once cold symptoms are reported, patients are often referred to endodontists.
As an endodontist, especially when a crack is suspected, a 3D scan is typically warranted. Why? What if I enter the tooth and see a crack extending far below the canal orifices? The patient could be disappointed with wasting their time and resources. A CBCT scan allows me to better inform the patient about the likelihood of saving the tooth, the prognosis, and better informs them with the information to make a decision regarding how to proceed.
In Figures 2 and 3, the patient had a visible craze line as well as an angular defect on 3D imaging but the angular distal defect, along with the probing was favorable so that this symptomatic upper premolar could be saved with endodontic treatment and a full coverage restoration. Even with this small “crack” the pulp was necrotic on this virgin tooth!

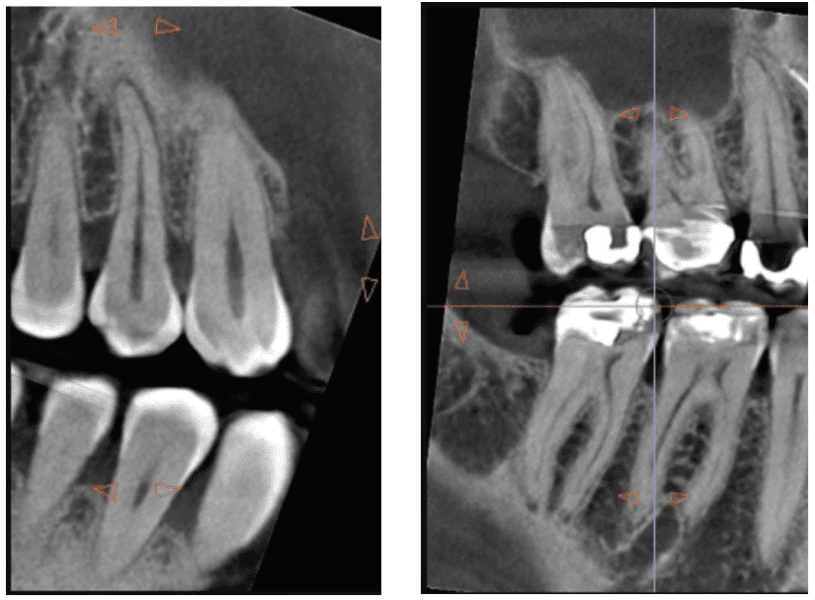
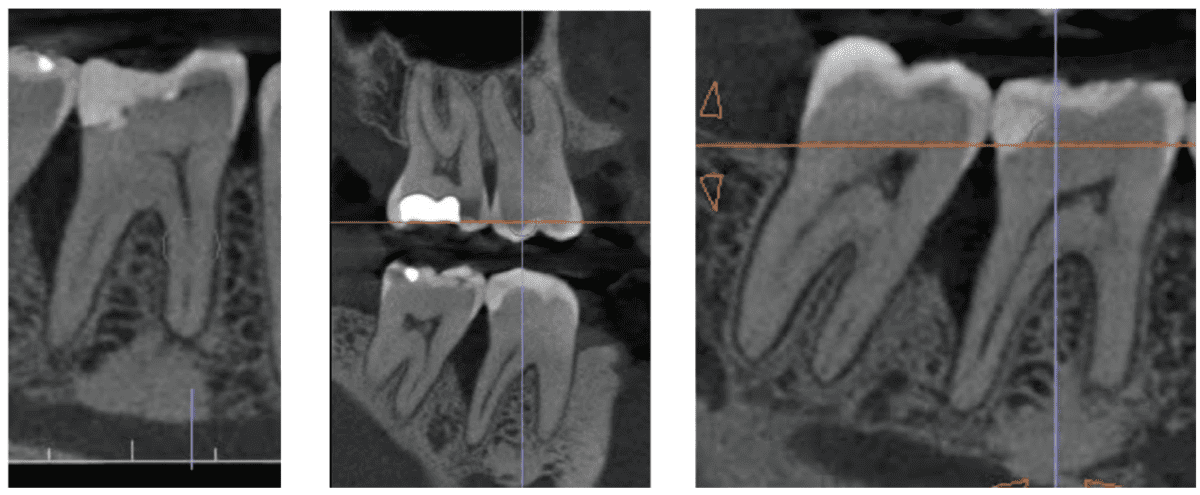
In Figures 4 and 5, cracks are clinically visible on this lower first molar. Figures 6-8 show a D angular defect on the CBCT screenshots in all planes. Once again, the angular defect along with the probing was favorable, and this molar also could be saved with endodontic treatment and a full coverage restoration. Even with these more significant and visible “cracks,” the pulp was vital but very inflamed and symptomatic.
Clinically, as we progressed to the endodontic access, we can appreciate the crack’s propagation apically in Figure 5.
The 3D axial image shows a black semi-circle lucent defect (like a Mickey Mouse ear) on the distal aspect of the tooth, reflecting the crack propagation and the lack of bone around that crack (Figure 6).
 Figures 6 (left); Figure 7 Center): Dips at point of crack; Figure 8 (right)
Figures 6 (left); Figure 7 Center): Dips at point of crack; Figure 8 (right)
The 3D coronal slice (Figure 7), however, shows the interproximal defect across the horizontal bone aspect. The 3D sagittal slice shows the D angular defect in Figure 8. Comparatively, the referring doctor’s 2D periapical film (Figure 9) does not clearly reflect the crack or the true angular defect. This diagnosis can be easily missed because of the 2D radiographic limitations. A patient may present in pain, and without the appropriate diagnostic imaging, the severity of their situation may be easily overlooked. Eventually, without the appropriate treatment, a true completely cracked tooth may result, leaving extraction as the only option.
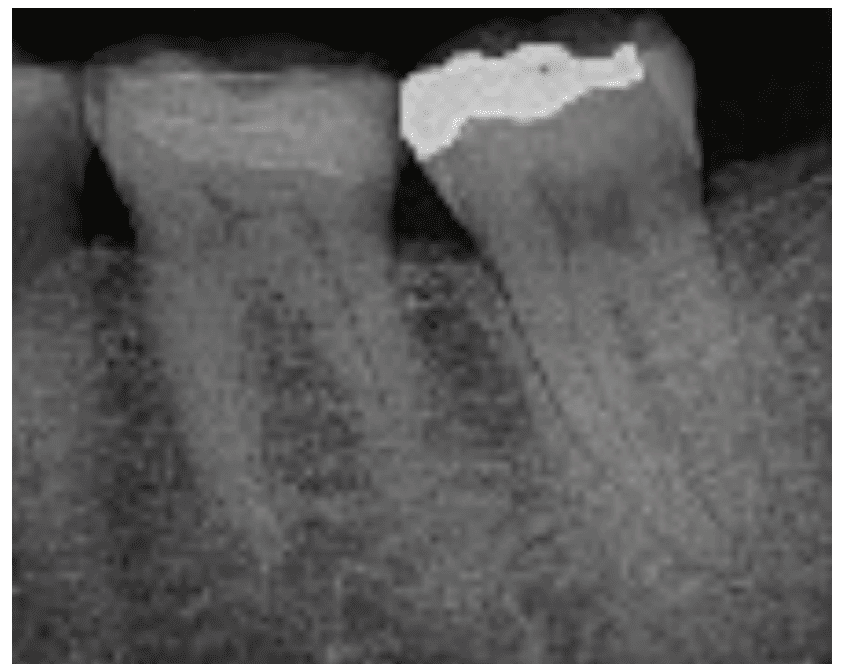 Figure 9
Figure 9
In this lower molar case, the patient had gone to the emergency room over a long weekend due to severe pain. The referring dentist had long-suspected it might be cracked, and a 6-mm periodontal probing depth (PPD) measurement was recorded.
“Based on the best available evidence to date, retaining this tooth with endodontic treatment and a full coverage restoration would have provided a predictable option.”1
Although I am biased, I personally would have elected to save this tooth if it were my own with a root canal (and a crown). With both, this tooth very likely could be functional for many years to come, and even possibly even with no further crack propagation or bone loss (with full crown coverage).
However, after much discussion, the patient shared they had already lost the same lower second molar on the opposite side due to a crack, so they elected for extraction.
Had the patient presented earlier with a smaller probing measurement and no pulpal symptoms, a root canal could have likely been avoided completely, and the tooth could’ve been saved simply with a full coverage restoration – a crown. All cracks, if caught and treated early, can be saved!
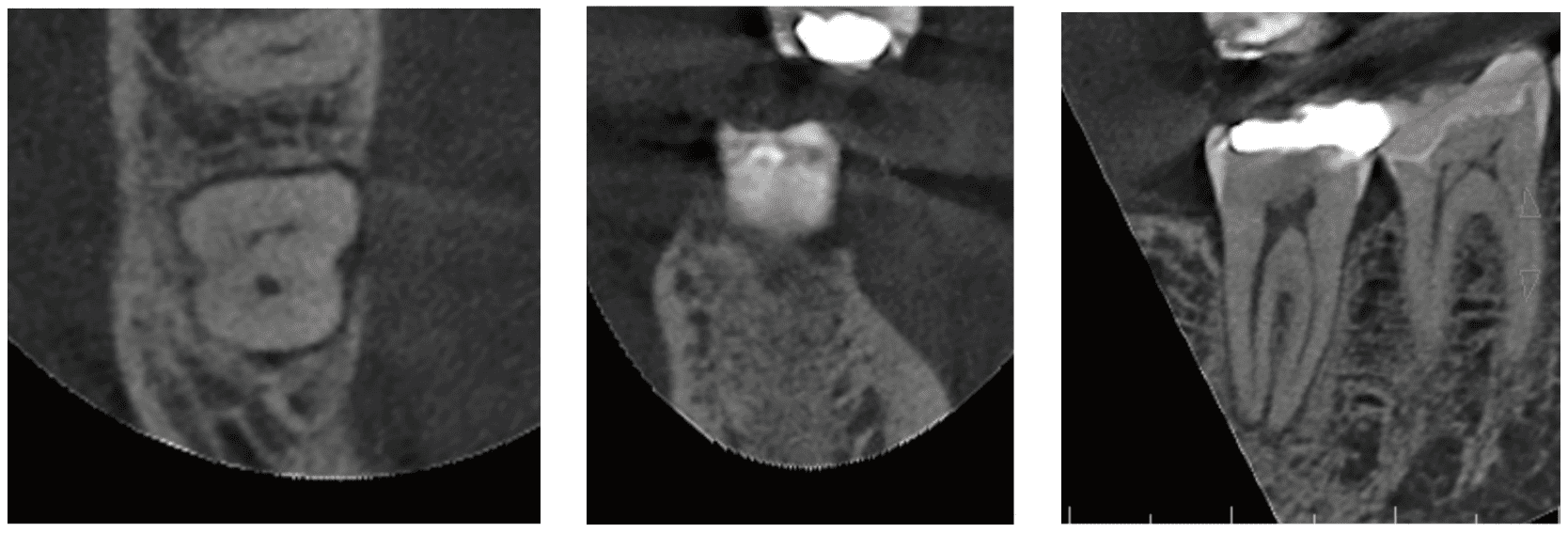
 Figures 10-12: Sagittal CBCT showing the distal angular defect extending more than 2/3 length of the root; this reflects a crack having extending apically, likely for years
Figures 10-12: Sagittal CBCT showing the distal angular defect extending more than 2/3 length of the root; this reflects a crack having extending apically, likely for years
I am often asked how deep can the crack go (PPD and be visualized on 3D) and still proceed prudently with (endo/resto) saving the tooth.
This is a complex and interdisciplinary answer. But to answer, I need more information, and I start with pulp testing. Sometimes there are endodontic symptoms – to varying degrees. Often, there is a probing defect, but sometimes there is not. Sometimes there is a bridge over the probing defect so the PPD could be inaccurate. Next is CBCT/3D-imaging, which brings things to light as it is a great representation of our 3D patient! Altogether, I then reflect on all of the information gathered – probing, the pulp vitality testing results, transillumination, the clinical exam and the patient’s chief complaint, and then their imaging: periapicals, bite wings, and 3D scan.
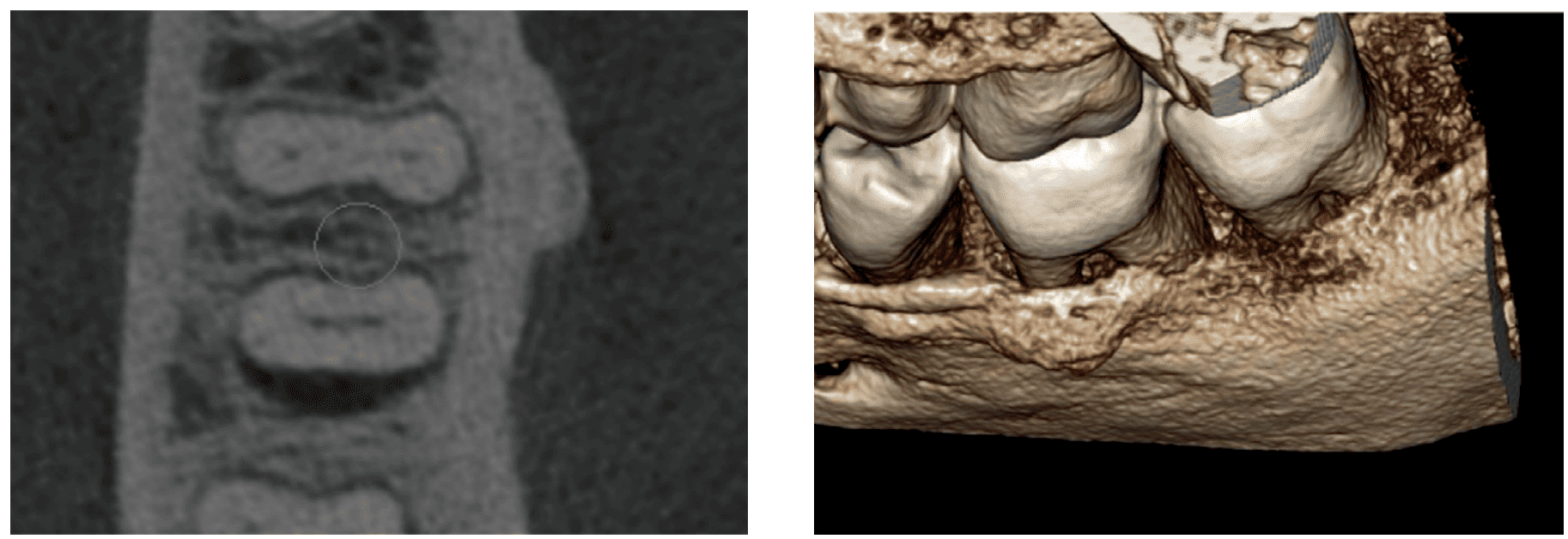 Figures 13 and 14: The axial image of the circumferential bone loss on this tooth; the 3D volume rendering showing the very clear distal aspect of the lower second molar, because there is no bone attached there
Figures 13 and 14: The axial image of the circumferential bone loss on this tooth; the 3D volume rendering showing the very clear distal aspect of the lower second molar, because there is no bone attached there
As a specialist, I defer and follow the lead of my quarterback, my referring dentist, before or after a conversation with the patient. In these cases, no matter the crack’s extent, I must connect with the patient’s general dentist. Often, the dentist decides that usually about 3 mms below the crestal horizontal bone, the prognosis is poor, and recommends extraction or an implant.
If symptomatic and urgent, then conversations are attempted in real time when possible.
A small subset of patients will still want to try to save the tooth even after knowing the guarded long-term prognosis. Understandably, if I had a cracked tooth, I would want to save it. I inform and stress the importance of follow-up to monitor for radiographic bone loss and any changes in probing measurements.
With a borderline prognosis and knowing that the tooth may only last a few years, this conversation also gets documented in the patient’s chart. Usually, the long-term prognosis is dismal, most especially because we’re sadly catching them too late.
The last case shares a patient with a very deep angular defect (Figures 10-14). This could not be saved, and in this case, there was no conversation about saving. I advised extraction as I felt any dentistry/endodontics would be a waste of everyone’s time and the patient’s resources to attempt further dentistry on this tooth.
To avoid the above scenario, the conversations we should be having are the incipient cracks and smaller PPDs that we encounter and visualize, especially during yearly prevention and prophy visits. Starting these crack conversations with discussion about occlusal guards and also full coverage restorations to avoid the propagation of these cracks when craze lines, with and without probing are visualized, is the best starting point for our patients.
My “Pro Tip” is that the team process can start in hygiene – to inform the dentists of any outlying periodontal measurements so that when these increased PPDs are visibly consistent with a craze line or crack, we can begin these conversations earlier than after when symptoms are present or cusps fracture. Very often a full coverage crown will prevent crack propagation and avoid endodontic symptoms from developing.
If you are visualizing cracks and/or a 4/5 mm probing, please consider obtaining a CBCT scan, as the 3D scan will show the true extent of a crack while most 2D X-rays may not show the extent of these cracks – even after it’s too late.
Let’s save some teeth!
Dr. John Rhodes also has helpful information regarding management of cracked teeth in his CE here: https://endopracticeus.com/ce-articles/identification-diagnosis-and-management-of-cracks/
- Davis MC, Shariff SS. Success and Survival of Endodontically Treated Cracked Teeth with Radicular Extensions: A 2- to 4-year Prospective Cohort. J Endod. 2019 Jul;45(7):848-855.
Stay Relevant With Endodontic Practice US
Join our email list for CE courses and webinars, articles and more..

 Judy McIntyre, DMD, MS, experienced dental trauma as a young child. Despite this, she had positive experiences at the dentist, and her passion to become a dentist developed. She attended the Harvard School of Dental Medicine, where she performed research on dental unit waterline biofilms. After graduation, Dr. McIntyre attended the University of North Carolina at Chapel Hill for her endodontic residency. Alongside renowned researchers in the field of endodontics, traumatology, and pediatric dentistry, her thesis and research regarding traumatic dental injuries has been published in numerous professional journals. Dr. McIntyre opened her own office in 2016 and has been active in organized dentistry. She is passionate about sharing her love for dentistry, trauma, radiology/imaging, and endodontics.
Judy McIntyre, DMD, MS, experienced dental trauma as a young child. Despite this, she had positive experiences at the dentist, and her passion to become a dentist developed. She attended the Harvard School of Dental Medicine, where she performed research on dental unit waterline biofilms. After graduation, Dr. McIntyre attended the University of North Carolina at Chapel Hill for her endodontic residency. Alongside renowned researchers in the field of endodontics, traumatology, and pediatric dentistry, her thesis and research regarding traumatic dental injuries has been published in numerous professional journals. Dr. McIntyre opened her own office in 2016 and has been active in organized dentistry. She is passionate about sharing her love for dentistry, trauma, radiology/imaging, and endodontics.