Continuing his series on endodontics, Dr. Tony Druttman looks at the best ways to measure the length of a canal
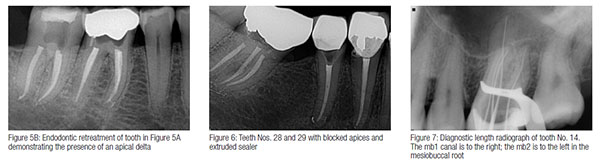
One of the main reasons endodontically treated teeth fail is because the canals have not been cleaned adequately. All too often, cases are referred for retreatment where the root fillings are short on the radiograph, and on retreating the tooth, the correct working length has been achieved (Figures 1A and 1B). Long root fillings have also been associated with endodontic failures, although this is usually due to inadequate debridement and disinfection, rather than overextension of the root filling through the root apex (Figure 2). Adequate canal preparation does not just involve reaching the apex with a file of a certain size: the canal has to be cleaned thoroughly in all its dimensions, but I’ll discuss this further in later issues.
 Determining the working length is an evolutionary process starting with the preoperative radiograph. As I have discussed in previous articles, a good quality radiograph has to be taken using the paralleling technique with the aid of an aiming device/image receptor holder. This should give an undistorted image of the crown and the roots. When using film, a reasonably accurate estimate of the working length can be achieved by measuring the length with a hand file against the film. With digital techniques, the software should be available in the program, which can measure the length, irrespective of whether the canal is curved or straight.
Determining the working length is an evolutionary process starting with the preoperative radiograph. As I have discussed in previous articles, a good quality radiograph has to be taken using the paralleling technique with the aid of an aiming device/image receptor holder. This should give an undistorted image of the crown and the roots. When using film, a reasonably accurate estimate of the working length can be achieved by measuring the length with a hand file against the film. With digital techniques, the software should be available in the program, which can measure the length, irrespective of whether the canal is curved or straight.
 Some canals are divergent from the long axis of the tooth and will look foreshortened on a radiograph. This is often the case with the palatal roots of upper molars but can affect other teeth as well (Figure 3).
Some canals are divergent from the long axis of the tooth and will look foreshortened on a radiograph. This is often the case with the palatal roots of upper molars but can affect other teeth as well (Figure 3).
It is therefore important to measure the working length accurately and to maintain working length during preparation. There are three methods for determining length: diagnostic length radiographs, electronic apex locators, and the consistent drying point,1 and during canal preparation, either two out of the three or all three methods can be used to give optimal results.
The apical extent of preparation
There are differing opinions regarding the apical extent of the preparation. The average distance between the apical constriction and the radiographic apex is 0.5 to 1.0 mm, but can be considerably more. The end point of preparation should be the minor apical diameter or apical constriction (Figure 4). The difficulty is that the position of this junction can be quite variable and by preparing the canal to an arbitrary end point, an apical plug of infected material may be left, which could result in failure. Also it is not unusual for the root tip to have multiple apical foramina, which may exacerbate the problem further (Figures 5A and 5B).

 The alternative approach is to maintain apical patency, and rather than to create an apical stop, a tapered preparation is developed, which relies on the developed geometry to create resistance form for the obturating material. Apical patency is created and maintained by inserting a small file approximately 1 mm through the apical constriction to ensure that an apical plug of dentin/infected material does not accumulate during preparation.
The alternative approach is to maintain apical patency, and rather than to create an apical stop, a tapered preparation is developed, which relies on the developed geometry to create resistance form for the obturating material. Apical patency is created and maintained by inserting a small file approximately 1 mm through the apical constriction to ensure that an apical plug of dentin/infected material does not accumulate during preparation.
Sometimes this is not possible as the canal appears to have a ledge at the apex, which has been created naturally rather than iatrogenically. This is due to the natural anatomy of the root, and it may be impossible to bypass the ledge. In this situation, the canal has to be prepared as far possible (Figure 6).
Radiographic technique
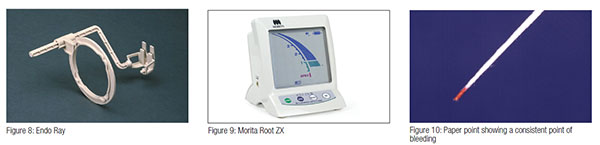
The traditional way of determining working length is by taking radiographs with files in the canals. Where canals overlap, as in the mesial canals of lower molars, the radiograph can be taken with an increased horizontal angulation to separate the canals. If the leading edge of the image receptor is angled away from the mesiodistal axis, the buccal canal is the more distal, and the palatal or lingual canal is the more mesial (Figure 7). A Hedstrom file can be used in one canal and a K-file in the other to distinguish between the canals. The radiographic technique is useful to cross check against an apex locator reading. Positioning the image receptor can be difficult with the rubber dam in place. Using a positioning device, such as the Endo Ray for use with film, ensures consistently accurate result (Figure 8).
 Electronic apex locators
Electronic apex locators
These are some of the most useful instruments that we have in endodontics and produce very reliable and reproducible readings. Recent research quotes 97% reliability.2 We now have sixth-generation units, which are designed to cope with any fluid in the canal. The convention is to take the “zero reading” length and reduce 0.5 mm to get the working length. I find my unit – a Morita Root ZX – gives me such reliable readings that I rarely need to take diagnostic length radiographs (Figure 9). Readings should be taken throughout the process of canal enlargement as the canal length can change especially in curved canals.
Consistent drying point technique
This is a simple technique, which determines the junction between where there is a blood supply, for example, the periodontal membrane, and where there is not, the prepared root canal. It can only work when patency filing is used. The canal is dried and a paper point inserted that will pass beyond this junction. The length of the dry part of the paper point is measured to confirm the working length (Figure 10). The technique is repeated three or four times to ensure that a consistent result is obtained. The canal length should also be confirmed by other means before the root filling is placed.
Dento-legal obligations
In our ever more litigious society, endodontics is one of the specialities that attracts the greatest amount of activity from our defense organizations. It is vital that the length of every canal is measured and recorded, whether by radiograph or electronic apex locator.
1. Rosenberg DB. The paper point technique, part 1. Dentistry Today. 2003;22:80-86.
Rosenberg DB. The paper point technique, part 2. Dentistry Today. 2003;22(2):62-64, 66-67.
2. Plotino G, Grande NM, Brigante L, Lesti B, Somma F. Ex vivo accuracy of three electronic apex locators: Root ZX, Elements Diagnostic Unit and Apex Locator and ProPex. Int Endod J. 2006;39:408–414.
Stay Relevant With Endodontic Practice US
Join our email list for CE courses and webinars, articles and more..

 Tony Druttman, MSc, BChD, BSc, is an endodontist working in central London. He is also a part-time teacher at the Eastman Dental Institute, University of London, and lectures in the UK and abroad.
Tony Druttman, MSc, BChD, BSc, is an endodontist working in central London. He is also a part-time teacher at the Eastman Dental Institute, University of London, and lectures in the UK and abroad.