Editor’s intro: In this Step-by-step, Dr. Carlos A. Spironelli Ramos shows the improved mixing and delivering properties of MTAFlow second-generation MTA cement.
Dr. Carlos A. Spironelli Ramos discusses a second-generation MTA with improved mixing/delivering properties
 Tricalcium silicate hydraulic cement materials such as the well-known mineral trioxide aggregate (MTA) are biocompatible materials with high-sealing ability and have been used for various reparative purposes in dentistry, including root-end filling, sealing perforations, treating open apices, and direct pulp-capping.1 Primarily composed of tricalcium silicates, MTA cements are radiopaque materials that form a self-setting calcium silicate hydrate mix when manipulated with water.2
Tricalcium silicate hydraulic cement materials such as the well-known mineral trioxide aggregate (MTA) are biocompatible materials with high-sealing ability and have been used for various reparative purposes in dentistry, including root-end filling, sealing perforations, treating open apices, and direct pulp-capping.1 Primarily composed of tricalcium silicates, MTA cements are radiopaque materials that form a self-setting calcium silicate hydrate mix when manipulated with water.2
The first formulation of MTA (1995) was composed of gray Portland cement with the addition of bismuth oxide powder as a radiopacifier. MTA has been recognized as a bioactive material that is hard tissue conductive, hard tissue inductive, and biocompatible, so the applications of this material have been rapidly expanding in dentistry. Despite such good characteristics, the first generation of MTA repair material presented some drawbacks, including difficult handling properties, a long setting time, and an unfriendly delivery method. The multipurpose use of MTA demanded the development of improved formulations. A shorter setting time and better washout performance were desired, so the clinician could feel confident that the product had set before the procedure was finished and wouldn’t be flushed out by water or blood. Considering the importance of the ideal flowability that a repair material should have to reduce the difficulty of handling and delivering, a high-plasticity MTA cement was developed with the aim of improving these characteristics.
Released in 2015, MTAFlow™ cement (Ultradent Products Inc.; South Jordan, Utah, Figure 1) is a bioactive repair material that represents a second-generation MTA with improved mixing/delivering properties. Keeping the same biological characteristics of the original MTA, this product presents advantages in the plasticity during mixing and versatility in terms of syringe-cannula delivery. The main differences in the presentation of MTAFlow are the particle size of the di- and tricalcium silicate powder and the viscosity of the water-soluble silicone-based gel. The use of antiwashout gel aims to increase viscosity and the resistance of particles to external water solutions while enhancing physical properties such as compressive strength, reduced setting time, and porosity. According to studies,3,4 the water-based gel in conjunction with the small particles facilitates manipulation and insertion into the cavity when compared with first-generation MTA, while showing biocompatibility and the ability to form biomineralizated tissue, representing an alternative to the conventional MTA.
Tricalcium silicate cements such as MTAFlow are now considered the materials of choice for vital pulp therapy. Histologic studies have demonstrated dentin-pulp regeneration without pulp inflammation in human teeth.5 The therapeutic use of these materials in direct pulp-capping implies their straight application on the underlying fibroblasts that have been reported to play a significant role in initiating pulp regeneration.6
A clinical direct pulp-capping application of MTAFlow is described in the numbered list.

 Direct pulp-capping
Direct pulp-capping
- Assess the pulp vitality and pulp inflammatory stage (normal, reversible, or irreversible pulpitis) using an ice test before anesthesia.
- Complete a cavity preparation outline under rubber dam isolation.
- Excavate all carious tooth structure using a round bur at low speed or use hand instruments.
- Gently rinse the exposed pulp with sterile saline solution.
- Control hemorrhage with pressure on the exposed pulp using a cotton pellet moistened with saline (Figure 2). If the hemorrhage/bleeding is abundant and cannot be controlled, correlate with the initial ice test result. In cases of suspected irreversible pulpitis and uncontrolled bleeding, consider a pulpectomy rather than a conservative procedure.
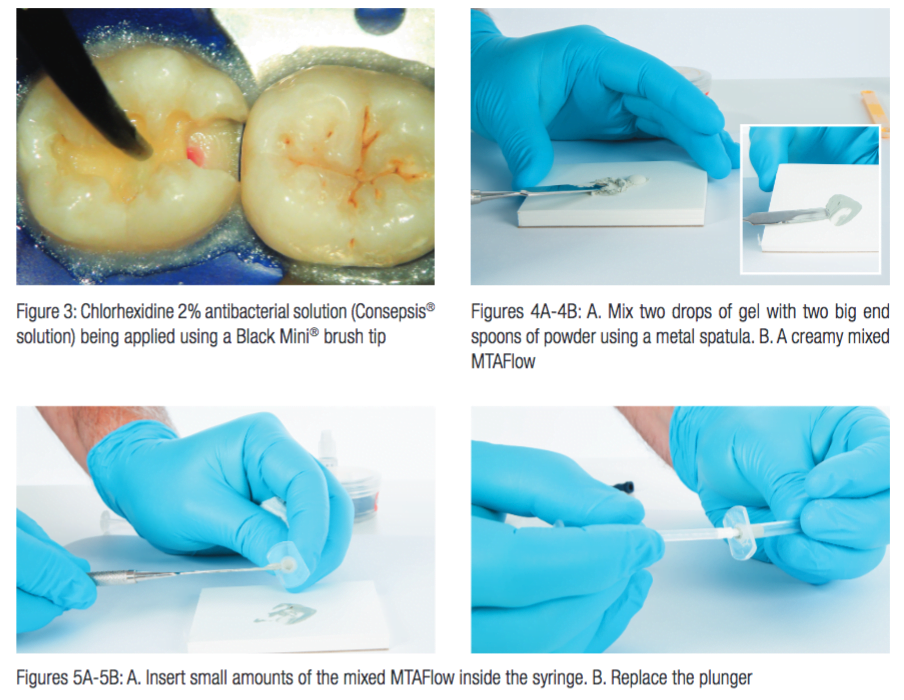
- Optionally, apply Consepsis® chlor-hexidine 2% antibacterial solution (Figure 3) for 60 seconds. Do not rinse. Gently air-dry.
- Using a metal cement spatula, gradually mix the 2 drops of gel into 2 big measuring spoon ends (0.26g) of powder until the chosen consistency is obtained. Thoroughly mix with the spatula to ensure all the powder particles are hydrated. Add more powder or liquid during or right after mixing to achieve the desired consistency (Figure 4).
- Remove the cap and plunger of the clear Skini syringe. Take small portions of the mixed MTAFlow with the mixing spatula, and insert the cement in the back part of the barrel. Replace the plunger back to the barrel (Figure 5). The mixed MTAFlow inside the syringe capped can be used for up to 15 minutes after mixing. Be sure there is no air inside the syringe
- Attach the Micro 20 ga Tip securely onto Skini syringe. Gently move the plunger to remove the air inside the syringe. Verify flow of cement prior to applying intraorally
- Gently insert MTAFlow cement on the pulp exposure without pressure (Figure 6).
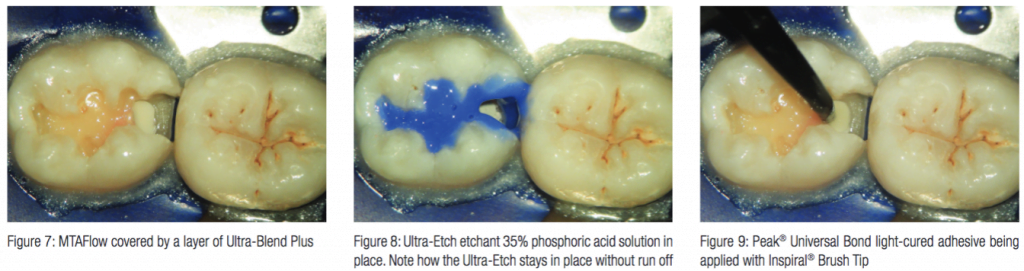
- Approximately 5 minutes after application, dry with a gentle blast of air (using ¼ to ½ air pressure). Note than now MTAFlow has an opaque surface. Place a light-activated liner (Ultra-Blend® Plus liner ) or a flowable composite (PermaFlo® composite) over the MTAFlow (Figure 7).
- Apply Ultra-Etch® etchant with the Blue Micro® Tip to all surfaces of tooth preparation for 20 seconds (Figure 8). Rinse thoroughly for 5 seconds. Apply Consepsis with Black Mini Brush Tip to preparation with a scrubbing motion. Lightly dry, leaving preparation slightly damp.
- Apply a puddle coat of Peak® Universal Bond light-cured adhesive with Inspiral® Brush Tip. Gently agitate for 10 seconds (Figure 9). Thin/dry 10 seconds using ¼ to ½ air pressure. Light-cure for 10 seconds (20 seconds for lights with output < 600mW/cm2).
- Proceed with the restoration.

 What makes MTAFlow different than other second-generation MTA cements? See a product profile by Ultradent here.
What makes MTAFlow different than other second-generation MTA cements? See a product profile by Ultradent here.
- Akbari M, Rouhani A, Samiee S, Jafarzadeh H. Effect of dentin bonding agent on the prevention of tooth discoloration produced by mineral trioxide aggregate. Int J Dent. 2012;563203; Epub 2011.
- Parirokh, M, Torabinejad, M. Mineral trioxide aggregate: a comprehensive literature review—part I: chemical, physical, and antibacterial properties. J Endod. 2010;36(1):16-27.
- Guimarães BM, Vivan RR, Piazza B, Alcalde MP, Bramante CM, Duarte MAH. Chemical-physical properties and apatite-forming ability of mineral trioxide aggregate flow. J Endod. 2017;43(10):1692-1696.
- Bueno CRE, Vasques AMV, Cury MTS, Sivieri-Araújo G, Jacinto RC, Gomes-Filho JE, Cintra LTA, Dezan-Júnior E. Biocompatibility and biomineralization assessment of mineral trioxide aggregate flow. Clin Oral Investig. 2018;Mar 23; ePub ahead of print.
- Nowicka A, Lipski M, Parafiniuk M, Sporniak-Tutak K, Lichota D, Kosierkiewicz A, Kaczmarek W, Buczkowska-Radlińska J. Response of human dental pulp capped with biodentine and mineral trioxide aggregate. J Endod. 2013;39(6):743-747.
- Klos A, Tenner AJ, Johswich KO, Ager RR, Reis ES, Köhl J. The role of the anaphylatoxins in health and disease. Mol Immunol. 2009;46(14):2753-2766.
Stay Relevant With Endodontic Practice US
Join our email list for CE courses and webinars, articles and more..

