Dr. Marga Ree treats a complicated dental trauma with a multidisciplinary approach
Introduction
According to various studies on prevalence and incidence of dental trauma, approximately 20-30% of all children have sustained some type of a traumatic dental injury to their permanent teeth. Adequate management of dental trauma is crucial for the long-term prognosis of a permanent tooth. Endodontic, restorative, and periodontal aspects must all be taken into consideration during treatment planning. Treatment of young permanent teeth with pulp involvement represents both an endodontic and a restorative challenge.
[userloggedin]
If pulp vitality is lost before root formation is completed, a root with thin dentinal walls may remain, which is more prone to fracture. After finishing endodontic treatment, an adequate restorative follow-up treatment with the aim of reinforcing the tooth is crucial for long-term survival. Therefore, minimally invasive endodontic and restorative treatment is to be preferred.

Case study
A 7-year old patient was referred for diagnosis and treatment of two maxillary central incisors. A couple of weeks prior, he was involved in a traffic accident, at which time, two upper central incisors were damaged. According to the treatment report of the oral surgeon, tooth No. 11 (American tooth No. 8) showed a complicated crown-root fracture, and tooth No. 21 (American tooth No. 9) showed an uncomplicated crown fracture and was luxated. The oral surgeon repositioned tooth No. 9 and applied a rigid splint. In addition, an attempt was made to cover the exposure site with composite. The patient was referred to the family dentist, and endodontic treatment of tooth No. 8 was recommended, if needed.
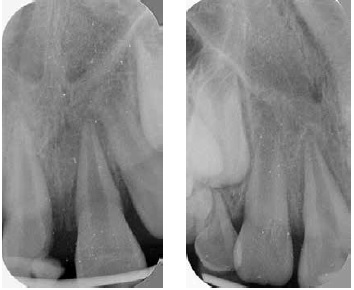
The patient was referred to our office 2 weeks after the accident took place. At the time of consultation, the splint had been in place for 2 weeks (Figure 1). The main complaint of the patient was sensitivity to percussion and palpation. His medical history was non-contributory. The splint impeded adequate oral hygiene. Clinical examination revealed an uncomplicated crown fracture of tooth No. 9 that was not sealed with composite. The fracture site of tooth No. 8 was partly covered by composite, but the bonding was insufficient to provide a hermetic seal. Radiographically, a crown-root fracture of tooth No. 8 and a widened periodontal ligament (PDL) of tooth No. 8 and No. 9 were visible (Figures 2-3). It was decided to remove the splint and re-evaluate the condition of both central incisors. After removal of the splint, it was obvious that the pulp had been exposed to the oral environment for 2 weeks, resulting in pulp necrosis (Figures 4-5). Tooth No. 9 responded positively to pulp tests, and the mobility was within normal limits. There was reasonable doubt about the reliability of the pulp test in tooth No. 9, and we suspected that the radiolucency associated with No. 9 was a sign of pulp necrosis (Figure 6). The preoperative diagnosis was a complicated crown-root fracture and apical periodontitis of tooth No. 8, and an extrusive luxation of No. 9. Treatment plan was root canal treatment in tooth No. 8 and highly likely in also in tooth No. 9, followed by restorative treatment with adhesive composite restorations.

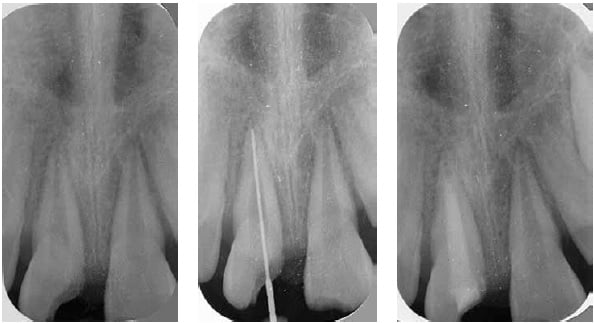
Local anesthesia was administered, and the teeth were isolated with a rubber dam. After working length determination with LightSpeed™ instruments (Figure 7) (marketed in its current form by Kerr Corporation, Orange, California), and mechanical and chemical debridement with 6% sodium hypochlorite (Vista Dental Products, Racine, Wisconsin), an interappointment dressing of calcium hydroxide (UltraCal® XS; Ultradent, South Jordan, Utah) was applied, and the tooth was temporized (Figure 8).
Three weeks later, a composite core (LuxaCore; DMG, Hamburg, Germany; DMG America, Englewood, New Jersey) was placed in tooth No. 8, while preserving the endodontic access cavity. Because the palatal outline of the fracture site was located deep under the gingiva, a gingivectomy was performed using an electrosurge. After application of retraction paste (3M, St. Paul, Minnesota), a dry work field was created, and a core form (Kuraray Noritake Dental Inc., Okayama, Japan) was applied, acting as a matrix. A pulp test in tooth No. 9 yielded a negative response, and the radiolucency associated with tooth No. 9 had increased in size. Root canal treatment was started, and the diagnosis apical periodontitis of tooth No. 9 was confirmed. After mechanical and chemical debridement of tooth No. 9, an interappointment dressing of calcium hydroxide was applied, and the tooth was temporized (Figure 9).

Four weeks later, the patient returned for finishing treatment. He was completely asymptomatic. After removing the calcium hydroxide by alternating 6% sodium hypochlorite (Vista Dental Products, Racine, Wisconsin) and 17% EDTA (Vista Dental Products, Racine, Wisconsin) ultrasonically activated, working length determination was repeated using LightSpeed instruments. The author follows a rule of thumb that if an apical foramen is equal or larger than a hand file or LightSpeed instrument No. 70 (=0.70 mm), a hydrophilic calcium silicate-based sealer in conjunction with gutta percha is to be preferred.
Traditional obturation methods do not provide an effective seal. They may shrink on setting, have little or no adhesion to dentin, and are not dimensionally stable when they come in contact with moisture, leading to dissolution and leakage over time. In recent years, new materials have been developed that overcome some of these shortcomings.
Since 2008, three premixed bioceramic products have been available: EndoSequence® BC Sealer™, EndoSequence® Root Repair Material™ (RRM) Paste, and Root Repair Material™ (RRM) Putty (Brasseler USA, Savannah, Georgia). Recently, these materials have also been marketed under the name of TotalFill® (FKG Dentaire SA, La Chaux-de-Fonds, Switzerland).
The manufacturer states that the three forms of bioceramics are similar in chemical composition (calcium silicates, zirconium oxide, tantalum oxide, calcium phosphate monobasic, and fillers), have excellent mechanical and biological properties, and good handling properties. They are hydrophilic, insoluble, radiopaque, aluminum free, and high pH, and require moisture to harden. The working time is more than 30 minutes, and the setting time is 4 hours in normal conditions, depending of the amount of moisture available. To date, over 100 studies have been published on premixed bioceramic materials in endodontics. The vast majority have shown that the properties are similar to Mineral Trioxide Aggregate (MTA).1-3
The apical foramen of tooth No. 8 was gauged to be a size 0.70 mm, and tooth No. 9 was gauged to be a size 0.90 mm

(Figure 10). After a final irrigation, the canals were dried with paper points. Gutta-percha cones taper .02 were fitted in the canals, and cut back 2 mm from working length (Figure 11) to create room for a hydrophilic calcium silicate putty, EndoSequence Root Repair Material Putty (Brasseler, Savannah, Georgia), that was applied with a Dovgan MTA gun (Hartzell and Son, Concord, California). The putty was applied by delivering it in small portions in the root canal, and tapping it in an apical direction with paper point of different diameters (Figure 12). After verifying the position of the apical plugs with a radiograph, gutta-percha cones were buttered with EndoSequence BC sealer and gently placed in the canals with a continuous movement (Figure 13). Then the gutta-percha cones were seared off with a tip of a MaxPack (Obtura Spartan, Algonquin, Illinois) to create room for a fiber- reinforced composite post (Figure 14). Many studies have shown that the use of fiber posts can increase the fracture resistance of immature, endodontically treated teeth,4-7 provided no additional tooth structure is removed to accommodate the post.
In addition to a good endodontic treatment using preferably a bioactive material, repair with minimally invasive restorative dentistry is paramount, and may hopefully result in a long-term tooth survival.
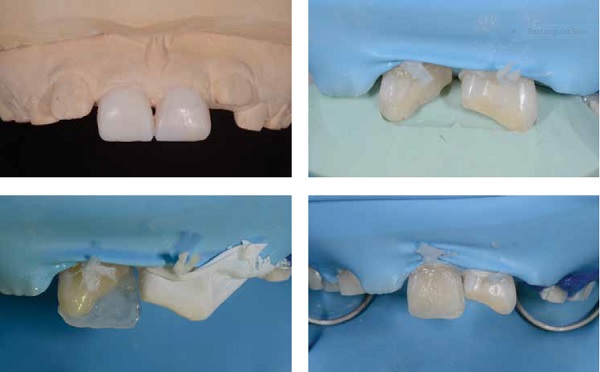
Subsequently, the dentin of the root canal walls and the pulp chamber was conditioned with Ultra-Etch® (Ultradent, South Jordan, Utah), SA primer, and Clearfil™ Photo Bond (Kuraray Noritake Dental Inc., Okayama, Japan). After conditioning the surface of the quartz fiber posts (D.T. Light-Post®, RTD, Saint Egreve, France) with Ceramic Primer (Kuraray, Kuraray Noritake Dental Inc., Okayama, Japan), they were cemented in the canals with LuxaCore, a composite core material (DMG, Hamburg, Germany; DMG America, Englewood, New Jersey). After the composite had fully set, the posts were cut back 2 mm under the cavo-surface, and covered with a hybride universal composite (Tetric Ceram®, Ivoclar Vivadent, Schaan, Lichtenstein; Amherst, New York) (Figure 15). Finally, the patient was referred to a restorative dentist for a definitive cosmetic restoration in both central incisors (Figure 16).

Courtesy of Artendo Enterprises Inc. This image was previously published in an article by Haapasalo, et al., titled “Clinical use of bioceramic materials,” in Endodontic Topics, 2015; 32:97-117, and is re-used with permission of Dr. Markus Haapasalo.


At the restorative treatment procedure, the bulk of the build-up in tooth No. 8 was removed, but the cervical part, that was located subgingivally, was left in place. The teeth were restored using a minimally invasive layering technique, after a wax-up was made by the laboratory (Figures 17A-17D). The patient and his parents were very satisfied with the result (Figures 18A-18D).

Follow-up
Radiographic and clinical examination after 20 months revealed complete resolution of the radiolucencies (Figure 19) and two healthy teeth in full function. The patient remained completely asymptomatic, he and his parents were very satisfied on the cosmetic and functional aspects of the composite restorations, and there were no signs of wear (Figure 20).

Conclusion
This case shows that a complicated fracture in a young patient can be successfully treated with a multidisciplinary approach. In addition to a good endodontic treatment using preferably a bioactive material, repair with minimally invasive restorative dentistry is paramount, and may hopefully result in a long-term tooth survival.
Common treatment planning, knowledge of each other’s areas of work, and regular communication makes interdisciplinary approach an exciting and educational experience for all parties, and may result in optimal care for our patients.
The Dental Trauma Guide, https://www.dentaltraumaguide.org, is a non-profit website dedicated to optimizing worldwide treatment of dental trauma. The website is developed in cooperation between the Copenhagen University Hospital and the International Association of Dental Traumatology (IADT). The latest update was carried out in 2014. The website is very user-friendly, and its use is strongly recommended by the author.
[/userloggedin]
[userloggedout][/userloggedout]
- Ree MH, Schwartz R. Clinical applications of bioceramic materials in endodontics. Endodontic Practice US. 2014;7(4):32-40.
- Prati C, Gandolfi MG. Calcium silicate bioactive cements: Biological perspectives and clinical applications. Dent Mater. 2015;31(4):351-370.
- Dawood AE, Parashos P, Wong RH, Reynolds EC, Manton DJ. Calcium silicate-based cements: composition, properties, and clinical applications. J Investig Clin Dent. 2015 Oct 5. doi: 10.1111/jicd.12195. [Epub ahead of print] Review.
- Desai S, Chandler N. The restoration of permanent immature anterior teeth, root filled using MTA: a review. J Dent. 2009 Sep;37(9):652-657.
- Cauwels RG, Lassila LV, Martens LC, Vallittu PK, Verbeeck RM. Fracture resistance of endodontically restored, weakened incisors. Dent Traumatol. 2014 Oct;30(5):348-55.
- Brito-Júnior M, Pereira RD, Veríssimo C, Soares CJ, Faria-e-Silva AL, Camilo CC, Sousa-Neto MD. Fracture resistance and stress distribution of simulated immature teeth after apexification with mineral trioxide aggregate. Int Endod J. 2014 Oct;47(10):958-66.
- Dikbas I, Tanalp J, Koksal T, Yalnız A, Güngör T. Investigation of the effect of different prefabricated intracanal posts on fracture resistance of simulated immature teeth. Dent Traumatol. 2014 Feb;30(1):49-54.
Stay Relevant With Endodontic Practice US
Join our email list for CE courses and webinars, articles and more..

 Since 1980, Marga Ree, DDS, MSc, has had a private practice in Purmerend, which for the past 17 years has been dedicated to endodontics. Dr. Ree obtained her degree in dentistry from the University of Amsterdam in 1979. For the next 5 years, she was a part-time staff member of the department of Cariology Endodontology Pedodontology, as well as being a clinical instructor in the central dental clinic of the University of Amsterdam. In 1998, she entered a postgraduate program in endodontics, which she completed in 2001 with a Master of Science degree. Since that time, she has lectured widely and taught hands-on courses throughout the Netherlands and abroad. She is the primary author of several articles published in national and international journals and has contributed to several books on endodontics and restorative dentistry.
Since 1980, Marga Ree, DDS, MSc, has had a private practice in Purmerend, which for the past 17 years has been dedicated to endodontics. Dr. Ree obtained her degree in dentistry from the University of Amsterdam in 1979. For the next 5 years, she was a part-time staff member of the department of Cariology Endodontology Pedodontology, as well as being a clinical instructor in the central dental clinic of the University of Amsterdam. In 1998, she entered a postgraduate program in endodontics, which she completed in 2001 with a Master of Science degree. Since that time, she has lectured widely and taught hands-on courses throughout the Netherlands and abroad. She is the primary author of several articles published in national and international journals and has contributed to several books on endodontics and restorative dentistry.