Dr. Renato Piai Pereira and colleagues illustrate a case of external inflammatory root resorption and a therapeutic approach to treatment.
Drs. Renato Piai Pereira, Murilo Priori Alcalde, Rodrigo Ricci Vivan, Marco Antonio Hungaro Duarte, Rogério Vieira Silva, and Clóvis Monteiro Bramante describe the therapeutic approach for a case of inflammatory external root resorption
Abstract
Introduction
External inflammatory root resorptions are pathologies that are difficult to treat. The treatment aims to eliminate the cause or stimulating factors of clastic cells such as infection and/or pressure. The size and location of the lesions are limiting factors for the treatment and maintenance of the affected tooth.
Objective
The objective of this study was to describe the therapeutic approach of a case of inflammatory external root resorption.
Methods
A 40-year-old female patient was referred for endodontic treatment of tooth No. 30, diagnosed with external inflammatory root resorption. The patient was scheduled for endodontic therapy with calcium hydroxide paste dressing to seal the resorbed area of root canal space with MTA and coronary restoration with composite resin.
Results and Conclusion
Clinical and radiographic follow-up after 1 year showed an absence of symptomatology, repair of the periapical region, and paralysis of resorption.
Introduction
Root resorption is a pathological process that occurs in permanent teeth both internally and on the outer root surface. Resorption occurs when the pre-dentin layer and odontoblasts present in the root canal, or when the pre-cementum and cementoblasts in the periodontal ligament (PDL) are damaged or removed.1 The etiology is mainly associated with dental trauma, surgical procedures, and excessive pressure of impacted teeth or tumors. It can also occur due to chemical irritation during tooth whitening and orthodontic movement procedures.1,2

Teeth affected by resorptive lesions are usually asymptomatic, and in many situations, the diagnosis may present as an incidental finding on routine radiographic examinations.3 Once resorption is detected, cone beam computed tomography (CBCT) is the test of choice to determine the location, extent, and differentiation of lesions, which are important for establishing an appropriate treatment plan and prognosis.4,5
Root resorption occurs in three stages: initiation, resorption, and repair.6,7 The process may have a self-limiting characteristic and may not be clinically detected.8 Once started, resorption depends on common factors that stimulate clastic cells, such as infection and/or pressure, to pro-gress the destruction of mineralized dental tissue. Since the treatment of inflammatory resorption is primarily aimed at removing stimulation factors,9 in cases of inflammatory root resorption associated with root canal infection, endodontic treatment usually has a favorable prognosis. Calcium hydroxide is the drug of choice because of its antimicrobial action, pH, necrosis of the granulation tissue present in resorption gaps, and its ability to stimulate repair.3 Based on these findings, the objective of this study was to describe the therapeutic approach of a case of inflammatory external root resorption.
Case description

A 40-year-old female patient was referred for endodontic treatment diagnosed with tooth pulp necrosis of lower right first molar. The medical history was not relevant. On clinical examination, tooth No. 30 had an extensive composite resin restoration. The thermal and electric sensitivity pulp tests had negative responses, while percussion and palpation were positive. The periodontal evaluation showed normal-colored gingival tissues and the absence of periodontal pockets. The radiographic examination showed the presence of nodules and narrowing of the pulp chamber, and in the periapical tissues, it was possible to identify a discrete radiolucent area lateral to the distal root of the tooth (Figure 1). Thus, the established pulp and periapical diagnoses were pulp necrosis and symptomatic apical periodontitis, respectively.
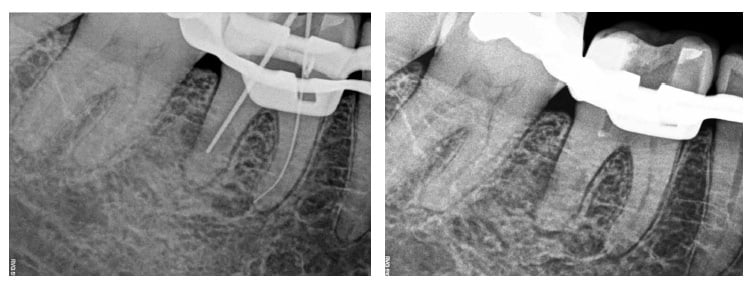
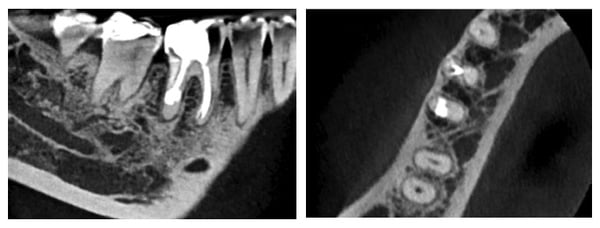
After endodontic treatment was instituted, access was performed with diamond spherical drills through the occlusal face. After access, it was difficult to locate one of the mesial conduits, so a CBCT was performed to assist in the anatomical understanding and consequent localization of the conduits. In addition to the conduit location, an extensive external inflammatory resorption lesion on the lateral surface and apical third of the distal root of tooth No. 30, communicating with the root canal, was identified on tomography (Figure 2). Soon the initial planning was changed to include resorption treatment. At the second visit, the canals were instrumented (Figure 3A), irrigated with 5.25% sodium hypochlorite and final agitation of 17% EDTA by means of an ultrasound insert (Irrisonic; Helse Ultrasonic, Santa Rosa de Viterbo, Brazil), with an application time of 1 minute by canal. The conduits, including the reabsorbed area, were filled with calcium hydroxide paste (Ultracal™ XS; Ultradent Products, Inc., South Jordan, Utah).

At the third visit, the intracanal medication was removed following the same irrigation protocol described earlier. The resorbed area was filled internally with MTA Repair HP (Angelus, Londrina, Brazil). Filling of the resorbed area was performed by interspersing the MTA condensation with radiographic examinations to ensure the complete sealing of the area and to prevent material leakage to the periodontium (Figure 3B). Endodontic obturation followed the vertical compression technique using Touch ‘n Heat™ 5004 (Kerr, Orange, California) with gutta-percha points and AH Plus® cement (Dentsply Detrey, Konstanz, Germany). The restorative procedure was performed at the end of the endodontic treatment in the same session (Figure 4). The inlet ducts were sealed with glass ionomer cement. The clinical sequence proceeded with the application of 35% phosphoric acid gel (Ultradent Products, Inc., South Jordan, Utah) for 20 seconds. The enamel and dentin surfaces were then washed and dried. The bonding agent (Tetric® N-Bond; Ivoclar Vivadent, Amherst, New York) was applied and polymerized according to the manufacturer’s instructions. The pulp chamber was filled with a low-viscosity single increment resin, SureFil SDR® Flow (Dentsply Caulk, Milford, Delaware). The occlusal anatomy was obtained using a high-viscosity nanohybrid composite resin, IPS Empress® Direct (Ivoclar Vivadent, Amherst, New York). After removal of the rubber dam, the restoration was occluded and adjusted.
Clinical and radiographic control at 1 year showed an absence of symptoms, and CBCT images showed a regression of the bone lesion and paralysis of the resorption process (Figure 5).
Discussion
The diagnosis of resorption lesions usually occurs through incidental findings on routine radiographic examinations, especially in early cases where there is no symptomatology.8 In contrast, the limitations of dental radiographic examinations are widely known3; periapical radiographs tend to underestimate the size of resorption lesions, while CBCT provides a more accurate estimate.10,11 Currently, CBCT is an important resource for the diagnosis and treatment of resorption, as it allows the identification of its correct location and extension.4,12 In the present case report, resorption was not clearly visible at the initial radiographic examination. The diagnosis was possible only after a CBCT was performed.
The treatment of root resorption is not always possible; the size, location, and restorability of the tooth are difficult obstacles to overcome.13 The therapeutic principle of dental resorption is based on the identification and elimination of the cause or factors that stimulate clastic cells, such as infection and/or pressure.9,14 For some authors, the prognosis is good when the stimulation is endodontic infection or orthodontic pressure. When the stimulation factor is periodontal infection, the prognosis may be unpredictable.3
Endodontic infection can stimulate or sustain inflammation in the PDL and lead to root resorption. Endodontic treatment, combined with calcium hydroxide paste dressing, interrupts the inflammatory process of resorption and allows periradicular recovery.15 In the present case, the control of root canal infection and the sealing of the MTA resorbed area were determinants for the prognosis of the treated tooth. The intracanal medication used, based on calcium hydroxide, also aimed to control bleeding and necrosis of granulation tissue present in the resorbed area, thus facilitating the internal repair of the lesion through the use of a repair cement, MTA HP repair. In this treatment, one of the challenges was the internal filling with the repairing cement of the resorption defect, since it was located in the apical third of the distal root of the lower molar. The result was achieved with the use of small endodontic compactors. The insertion of the MTA in the reabsorbed area was similar to the apical plug technique.16
Decision-making regarding the treatment of resorption should be based on the nature and cause of resorption, prognosis, and restorability of the tooth. The risks and benefits should be widely discussed with the patient.8 In addition to functional and esthetic restoration of the affected teeth, the treatment aims to stop the resorption process, and for this reason, a long-term follow-up is necessary to rule out the recurrence of this pathology. When conservative treatment by internal or surgical approach is not possible, other treatment options should be considered, including intentional replantation, periodic follow-up, or extraction.17
Conclusion
Based on the clinical, radiographic, and tomographic findings, the patient’s general health and the application of scientifically supported techniques, this clinical case showed the possibility of treating an external resorption by an internal approach with a satisfactory outcome.
Besides participating in this article on external inflammatory root resorption, Dr. Murilo Priori Alcalde co-authored an article titled, “Identification and resolution of edema of the head/neck in a 7-year-old child.” Read about treatment of this challenging and dangerous condition.
https://endopracticeus.com/clinical-articles/identification-resolution-edema-head-neck-7-year-old-child/.
- Leach HA, Ireland AJ, Whaites EJ. Radiographic diagnosis of root resorption in relation to orthodontics. Br Dent J. 2001;190(1):16-22.
- Fuss Z, Tsesis I, Lin S. Root resorption – diagnosis, classification and treatment choices based on stimulation factors. Dent Traumatol. 2003;19(4):175-182.
- Darcey J, Qualtrough A. Resorption: part 2. Diagnosis and management. Br Dent J. 2013;214(10):493-509.
- Fayad MI, Nair M, Levin MD, et al. AAE and AAOMR joint position statement: use of cone beam computed tomography in Endodontics 2015 update. Oral Surg Oral Med Oral Pathol Oral Radiol. 2015;120(4):508-512
- Patel S, Dawood A. The use of cone beam computed tomography in the management of external cervical resorption lesions. Int Endod J. 2007;40(9):730-737.
- Mavridou AM, Hauben E, Wevers M, et al. Understanding external cervical resorption patterns in endodontically treated teeth. Int Endod J. 2017;50(12):1116-1133.
- Mavridou AM, Hauben E, Wevers M, et al. Understanding External Cervical Resorption in Vital Teeth. J Endod. 2016;42(12):1737-1751.
- Patel S, Saberi N. The ins and outs of root resorption. Br Dent J. 2018;224(9):691-699.
- Tsesis I, Fuss Z, Rosenberg E, Taicher S. Radiographic evaluation of the prevalence of root resorption in a Middle Eastern population. Quintessence Int. 2008;39(2):e40-e44.
- Ball RL, Barbizam JV, Cohenca N. Intraoperative endodontic applications of cone-beam computed tomography. J Endod. 2013;39(4):548-557.
- Patel S, Dawood A, Ford TP, Whaites E. The potential applications of cone beam computed tomography in the management of endodontic problems. Int Endod J. 2007;40(10):818-830.
- Vaz de Souza D, Schirru E, Mannocci F, Foschi F, Patel S. External Cervical Resorption: A Comparison of the Diagnostic Efficacy Using 2 Different Cone-beam Computed Tomographic Units and Periapical Radiographs. J Endod. 2017;43(1):121-125.
- Smidt A, Nuni E, Keinan D. Invasive cervical root resorption: treatment rationale with an interdisciplinary approach. J Endod. 2007;33(11):1383-1387.
- Consolaro A. The four mechanisms of dental resorption initiation. Dental Press J Orthod. 2013;18(3):7-9.
- Ricucci D, Siqueira JF Jr, Loghin S, Lin LM. Repair of extensive apical root resorption associated with apical periodontitis: radiographic and histologic observations after 25 years. J Endod. 2014;40(8):1268-1274.
- Pace R, Giuliani V, Pini Prato L, Baccetti T, Pagavino G. Apical plug technique using mineral trioxide aggregate: results from a case series. Int Endod J. 2007;40(6):478-484.
- Ehlinger C, Ginies E, Bornert F, et al. Decision criteria influencing the therapeutic approach to invasive cervical resorption: a case series. Quintessence Int. 2019;50(6):494-5
Stay Relevant With Endodontic Practice US
Join our email list for CE courses and webinars, articles and more..

 Renato Piai Pereira, DDS, MSc, is Professor of the State University of Southwest Bahia (UESB). At the moment, he is a PhD candidate of the Department of Operative Dentistry, Endodontics, and Dental Materials at the Bauru School of Dentistry (FOB/USP).
Renato Piai Pereira, DDS, MSc, is Professor of the State University of Southwest Bahia (UESB). At the moment, he is a PhD candidate of the Department of Operative Dentistry, Endodontics, and Dental Materials at the Bauru School of Dentistry (FOB/USP).