Dr. John West discusses interdisciplinary treatment planning and the art of saving compromised teeth in his Endodontic Perspective.
Dr. John West discusses saving endodontically diseased teeth with consensus diagnosis, interdisciplinary treatment planning, and sequencing
Introduction
Endodontically treated teeth can be the weakest link in the esthetic/restorative diagnosis and treatment plan. They can also be the missing link between success and failure of the interdisciplinary treatment plan.
In this, the second decade of the 21st century, we are born out of the humblest biologic stance: When the cause of a disease is removed, the disease itself disappears. The former disease cannot produce continued pathology because, quite simply, it is gone!1 And not only is the disease gone, but the results of the disease are no longer sustainable without the cause. It’s that simple. We, as dentists, are the caretakers of this biologic tenet. And yet, we sometimes forget. We forget because it is easy. We forget because it is hard. We forget because we may be thinking of ourselves and not the patient. We forget because it is convenient. We forget because we failed to do the right thing.
Doing the right thing
I chose these five predictable, long-term interdisciplinary endodontic patient presentations as examples of doing the right thing. All patients’ continued care records are from 18 to 26 years posttreatment. They may not have been the safest, the easiest, or the most clinically productive, but they were the right treatment plans for their times. Today, the narrative trend is to “remove and replace” endodontically diseased teeth when in doubt.2 My goal is for these five examples to serve as a reminder that the “always” answer in interdisciplinary endodontic treatment planning is easily found in the answer to the 8-word question “What would I do if it were me?” I am convinced that after reviewing these five patients’ options and considering that endodontic techniques can be mastered by any dentist who wants to learn endodontic skills, the reader will have a new appreciation for the long-term capacity of healing or preventing lesions of endodontic origin. And I submit that if the reader were the patient in these five patient examples, he or she would have chosen the same right thing for him or herself. The interdisciplinary endodontic treatment planning that was chosen by each patient was the right thing for that patient, for the dentist, and for dentistry. Making these choices, to me, is the hallmark of a true caregiver.3,4
The interdisciplinary endodontic treatment planning for each of the five example patients was based on three considerations: 1) biology, 2) structure, and 3) esthetics. Specifically, can the root canal system portals of exit (POEs) be predictably cleaned and sealed either nonsurgically or surgically? Is the periodontal condition healthy, or can it be made so? Structurally, is there sufficient ferrule width and ferrule height? Is there at least 4.0 mm from height of bone to height of ferrule? Esthetically, does the endodontically involved tooth enhance the dental esthetics, and if not, can it be made to do so?
Patient reports
Patient 1
A patient had a residual sinus tract tracing to the lateral wall of the maxillary right central incisor after a third, and finally esthetic bridge attempt.
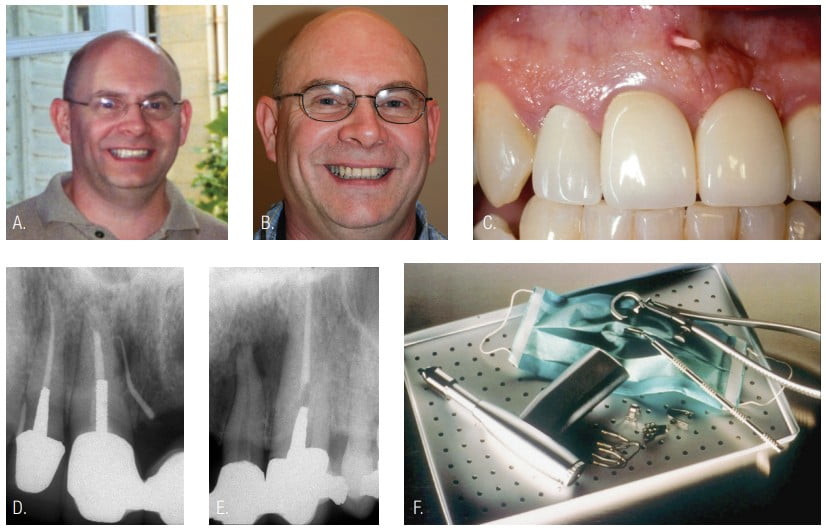
Biologic considerations: What is the multiple abutment pulpal status? Can the underfilled anatomy of tooth No. 8 be treated surgically and still seal all POEs that could be inaccessible? Can the post be removed nonsurgically, and could underfilled anatomy be successfully discovered, cleaned, and obturated? Is the periodontal condition healthy?
Structure considerations: Can the FPD be removed without breaking teeth or damaging the FPD? Note that the FPD was luted in (not bonded) with zinc phosphate cement. Can the post be removed without affecting the ferrule?
Esthetic considerations: If endodontic surgery were chosen, could scarring or black triangles be risk factors? With a high smile line, however, surgery was not contra-indicated. If surgery is done for tooth No. 8, what about for the nonvital pulp in tooth No. 10? The need to access through FPD or remove FPD already exists. What about removal and implants? The patient loved the bridge, as it was the third attempt to get his smile right again after his car accident. He had no interest in another bridge or implants and understood a nonsurgical interdisciplinary treatment plan was the most predictable but not without possible peril.
Interdisciplinary treatment planning and sequencing: The plan was to successfully remove the bridge, and for nonsurgical endodontic retreatment of tooth No. 8, and nonsurgical endodontic treatment of tooth No. 10. The bridge would be permanently cemented after evidence of sinus tract healing (Figure 1).

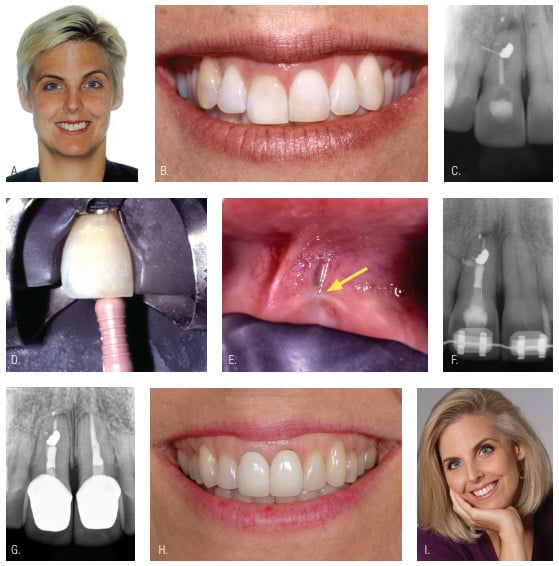
Patient 2
The patient had previously experienced multiple accidents to her maxillary anterior teeth and presented with a sinus tract in tooth No. 8.
Biologic considerations: Is nonsurgical or surgical endodontic treatment more predictable given that a lateral POE could not be only lateral but also toward the palatal, making it surgically inaccessible for preparation and obturation? The patient wanted to consider modeling someday and did not want to risk surgical scarring of any kind.
Structure considerations: Can a nonsurgical approach preserve the ferrule?
Esthetic considerations: An uneven gingival smile line was present that the patient wanted corrected. The orthodontist and prosthodontist agreed to sequencing their treatments once the endodontic status of her maxillary right central incisor was known.
Interdisciplinary planning and sequencing: After nonsurgical endodontic retreatment of tooth No. 8, orthodontic treatment to align teeth and correct tooth No. 8’s gingival levels was done. Esthetic restorative dentistry was done as needed (Figure 2).
 Patient 3
Patient 3
The patient presented with percussion and palpation sensitivity in tooth No. 8. She also wanted to remove the “black area between the tooth and gingiva.” Her dentist thought that he could cover the dark halo with a new crown, but he requested internal bleach in order to eliminate the possibility of a dark reflection into the gingiva even with new crown.
Biologic considerations: A persistent radicular LEO due to probable coronal leakage and seal breakdown of the silver cone and sealer obturation were present.
Structure considerations: Shape the endodontic preparation while preserving root width and ferrule.
Esthetic considerations: Internal bleaching, followed by a new crown once endodontic symptoms were absent.
Interdisciplinary planning and sequencing: Successful nonsurgical endodontic retreatment and safe internal bleaching were done, and a new crown was placed (Figure 3).

Patient 4
A dentist accidentally created a mesial perforation during endodontic access. The dentist and patient needed an interdisciplinary evaluation. Since implants were not yet mainstream when this patient presented 27 years ago, the choices were to extract and place an FPD or attempt to save the tooth. While the orthodontic evaluation suggested the possible removal of tooth No. 12 followed by orthodontic alignment, the patient absolutely did not want full orthodontics. He wanted “this tooth fixed.”
Biologic considerations: Seal the root canal system nonsurgically. Periodontal pocket correction with osseous recontouring was followed by forced orthodontic eruption in order to create 4 mm from height of bone to height of ferrule. Proper final restoration shape was needed to allow easy plaque control.
Structure considerations: None with nonsurgical endodontics.
Esthetic considerations: The emergence profile must look natural enough.
Interdisciplinary planning and sequencing: Successful nonsurgical endodontics, forced orthodontic eruption, osseous recontouring, and restorative dentistry (Figure 4).

Patient 5
The patient presented with a sinus tract and receding gingival tissue in tooth No. 8.
Biologic considerations: Can non-surgical endodontics be predictably successful if the silver cone is removed and if the apical tooth segment and silver cone section remain without pathology?
Structure considerations: None if the third, third, third rule can be achieved (i.e., the maximum-shaped canal should not exceed one-third the width of the root at any level).
Esthetic considerations: Can gingival levels be corrected through a connective tissue graft once the sinus tract is healed?
Interdisciplinary planning and sequencing: Nonsurgical endodontic treatment in the coronal section of tooth No. 8. After proof of sinus tract healing, a connective tissue graft was done to correct tissue levels (Figure 5).

Closing comments
Would we choose these same five endodontic interdisciplinary treatment plans today?
The answer is yes, given that implants were only becoming mainstream when these patients were treated. Nonetheless, even today, the art of saving compromised teeth, particularly endodontically treated teeth, may seem to have been lost. However, in proper hands and with interdisciplinary planning and consensus diagnosis, the art and science are alive and well. Endodontic interdisciplinary treatment planning gives patients their best path, their right path. It’s the right thing!
The following quote by author M.H. McKee perhaps best summarizes the lesson of this article: “Wisdom is knowing the right path to take … integrity is taking it.”
This article was reprinted with permission from Dentistry Today.
Interdisciplinary treatment planning is a focus of Dr. West’s article on the “three Fs of predictable endodontics.” Find out what they are here: https://endopracticeus.com/three-fs-predictable-endodontics-finding-following-finishing/
- Schilder H. Cleaning and shaping the root canal. Dent Clin North Am. 1974;18(2):269-296.
- West J. Implants versus endodontics: “As the pendulum swings.” Dent Today. 2014;33:10-12.
- West JD. Endodontic predictability—“Restore or remove: How do I choose?” In: Cohen M, ed. Interdisciplinary Treatment Planning: Principles, Design, Implementation. Hanover Park, IL: Quintessence Publishing; 2008.
- West J. Endodontic update 2006. J Esthet Restor Dent. 2006;18(5):280-300.
Stay Relevant With Endodontic Practice US
Join our email list for CE courses and webinars, articles and more..

 John West, DDS, MSD, received his DDS degree from the University of Washington, where he is an affiliate professor. He is the founder and director of the Center for Endodontics in Tacoma, Washington, and a clinical instructor at Boston University, where he earned his MSD degree and was honored with the Distinguished Alumni Award. Dr. West is in private endodontic practice in Tacoma. Dr. West can be reached at johnwest@centerforendodontics.com.
John West, DDS, MSD, received his DDS degree from the University of Washington, where he is an affiliate professor. He is the founder and director of the Center for Endodontics in Tacoma, Washington, and a clinical instructor at Boston University, where he earned his MSD degree and was honored with the Distinguished Alumni Award. Dr. West is in private endodontic practice in Tacoma. Dr. West can be reached at johnwest@centerforendodontics.com.