Jordan Reiss, Carestream Dental’s national sales director for 3D imaging, addresses some questions about CBCT imaging for the endodontic office
It’s a fact that endodontists have consistently embraced new technology faster than general practitioners. As specialists, it’s only natural that they should require specialized technology. Today, cone beam computed tomography (CBCT) systems give endodontists greater diagnostic capabilities and provide enhanced care to patients. There’s compelling evidence that you should be using this technology in your practice; however, “going 3D” is an even bigger paradigm shift than moving from film to digital.
A CBCT system is a worthy investment, but admittedly a big one. And with more than 50 different CBCT solutions on the market, taking it all in can be overwhelming. If you’re considering a CBCT system for your practice, there are some key questions to ask to ensure your new technology works to your advantage.
The must-haves
- Does it feature a focused field of view (FOV)?
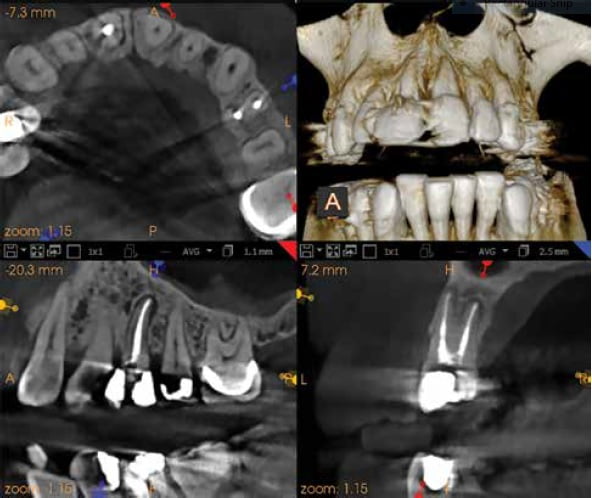
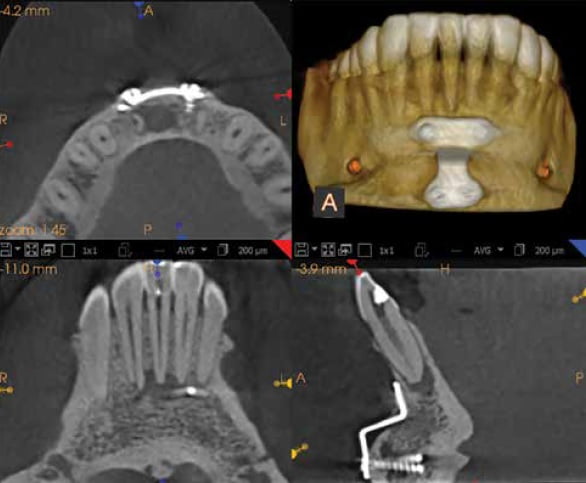
In 2015, the AAE and American Academy of Oral and Maxillofacial Radiology (AAOMR) released a more comprehensive update to the original joint position statement released 5 years prior regarding CBCT. Of the 12 recommendations for when limited FOV CBCT “should be considered the imaging modality of choice,” 10 recommend the use of CBCT over intraoral radiography. Therefore, it’s essential that any CBCT system you choose provide a focused FOV, such as 5 cm x 5 cm. Ideally, a system should include endodontic-specific modes that combine a focused FOV with high resolution at a low dose. Many studies have shown that high resolution scans greatly assist with diagnosis. Per an AAE Communiqué (January 2014), “numerous authors have illustrated the usefulness and importance of CBCT in the diagnosis and management of dentoalveolar trauma, especially root fractures” to most effectively diagnose disruptions to the space.
- Can I view clinical images taken with this unit to determine image quality?
One of the greatest benefits of a CBCT system is its ability to remove overlying structures — superimpositions — when viewing a scan. But the patient’s own anatomy isn’t the only thing that can block your diagnostic efficacy when trying to treatment plan a region of interest. When looking at a CBCT system, be sure to request scans of complex cases involving metal, silver points, gutta percha, or implants — clinical cases where there are a lot of foreign materials. Slick marketing for CBCT systems focus on catchy terms like metal artifact reduction (MAR) or scatter reduction technology (SRT), but looking at real cases in the software that comes with the system will provide clarity. High-quality scans are what will help you make the best diagnosis in a clinical setting, not idealized marketing images.
- How intuitive is it for the clinician and the staff to use?
Easy-to-use 3D imaging software makes using your system more intuitive. We’ve seen how much CBCT software has progressed in the past few years. With all of these changes, supportive educational resources for using the software and consistent, reliable updates are key. Also, consider a system that makes it easy for your staff to acquire images — some examples of this include laser-free positioning and face-to-face positioning. Don’t forget about how the new system will integrate with your existing dental practice management software (DPMS). Seamless integration not only shortens the learning curve, but also creates the staff perception that the new unit is simply an additional module to the DPMS they’re already familiar with using.
- Does the company you’re looking to purchase from offer ongoing training?
Every CBCT system on the market comes with an upfront training session, but I cannot overemphasize the value of good training, education, and support on an ongoing basis. You’re about to make a big investment, and you’ll want to ensure you’re getting the most out of your system. Look to partner with a company that wants you to succeed as a clinician by offering live hands-on courses to better understand your imaging software. Other examples of ongoing education include access to an online video library of tips and tricks and how-tos or free webinars, both recorded and live, for your staff to participate in. The most advanced system on the market doesn’t benefit you or your patients if not used properly, and training ensures you’re using the system to your best advantage.
The nice-to-haves
- How easy is it to share files?
All systems are DICOM-compatible, but does the system you’re considering acquire images natively in DICOM, or do you need to convert the file? A DICOM-ready file eliminates extra steps, reduces overall storage, and easily imports into third-party systems that allow for surgical guides, implant planning, and many other procedures.
- Will this system help or hinder my relationship with referrals?
The ease of sharing images brings me to the importance of referrals. In fact, you may find that a “side effect” of CBCT is a better relationship with other doctors. It’s important that you can share the full version of your 3D software (including implant planning) with referrals, so they can better understand your diagnosis and eliminate the chance of miscommunication.
Today, cone beam computed tomography (CBCT) systems give endodontists greater diagnostic capabilities and provide enhanced care to patients.
The splurges
- Are there any add-ons or upgrades I could consider in the future?
Look for a system that can grow as your practice does. If you plan to collaborate with implantologists or are hoping to someday add another specialist to your practice, consider a CBCT system that allows you to add FOVs to meet future needs. Other add-ons include extraoral imaging filters, object acquisition, and cephalometric arms.
- Will this system help me with advanced treatments and techniques?
Having a system with a deeper gray scale (or bit depth) allows you to do more, such as create STL files (digital models and impressions) that can be used for surgical guides and implant planning. These features are already popular with implantology, but will likely grow into endodontics in the next few years.
What you should take away from these questions is that, as a specialist, your technology must adapt to your unique needs — not the other way around. Invest in a solution that provides endo-specific features for more precise diagnosis, increased patient case acceptance, and improved relationships with referrals.
Like the microscope before it, a CBCT system is the new standard of practice for endodontists. If you’re in doubt, consider the words of Dr. John Khademi of Four Corners Endodontics in Durango, Colorado.:
“Unlike the microscope — which I think is necessary for practicing at a high level — I do think that it’s possible to practice high-level endodontics without CBCT.”
“However, I think it is impossible to practice at the highest level.”
When you’re ready to practice at the highest level, asking the preceding questions can help you navigate the selection of CBCT systems on the market and ultimately help you find the one that will improve your diagnostic capabilities, treatment planning, patient care, and colleague collaboration.
Stay Relevant With Endodontic Practice US
Join our email list for CE courses and webinars, articles and more..

