Dr. John Rhodes presents a nonsurgical retreatment of a central incisor that had previously suffered trauma
 A 20-year-old woman was referred suffering from occasional, spontaneous toothache around the maxillary right central incisor (UR1). This radiated to an area underneath the nose and varied in intensity but could be sufficiently bad enough to disrupt normal activity, such as driving a car. She was unable to bite on the tooth without discomfort.
A 20-year-old woman was referred suffering from occasional, spontaneous toothache around the maxillary right central incisor (UR1). This radiated to an area underneath the nose and varied in intensity but could be sufficiently bad enough to disrupt normal activity, such as driving a car. She was unable to bite on the tooth without discomfort.
[userloggedin]
 When she was 9 years old, she had tripped and fallen onto a post, traumatizing the UR1 and causing an enamel-dentin fracture that did not expose the pulp.
When she was 9 years old, she had tripped and fallen onto a post, traumatizing the UR1 and causing an enamel-dentin fracture that did not expose the pulp.
From the patient’s perspective, everything appeared to be fine until about 3 years after the accident when the UR1 started to become painful to bite on, and the gum was sore. The general dental practitioner root filled the tooth, and it settled down.
 More recently, this young lady had become very conscious of the tooth darkening and sought the opinion of a new dentist to see whether a veneer was feasible. When a periapical radiograph was exposed, it showed a poor root filling and large apical radiolucency, and at this point, the patient was referred to an endodontic specialist, in line with good practice (General Dental Council, 2013). Her medical history was uncomplicated, and apart from an allergy to penicillin, she was fit and well.
More recently, this young lady had become very conscious of the tooth darkening and sought the opinion of a new dentist to see whether a veneer was feasible. When a periapical radiograph was exposed, it showed a poor root filling and large apical radiolucency, and at this point, the patient was referred to an endodontic specialist, in line with good practice (General Dental Council, 2013). Her medical history was uncomplicated, and apart from an allergy to penicillin, she was fit and well.
This article describes the nonsurgical retreatment of a central incisor that had previously suffered trauma. The immature root was managed using a biological approach with micro-endodontic techniques.
Clinical examination
Intraoral examination revealed that the UR1 was tender to palpation. It was not abnormally mobile nor was it ankylosed. The color was significantly darker than the adjacent incisor teeth with a VITA equivalent shade of C3/C4 compared with healthy teeth at A2.
Photographs were taken for patient records at this point. There was an incisal/buccal composite restoration that was no longer a good color match and had visible margins.
 Soft tissue examination revealed no buccal swelling, but the mucosa was tender over the apex of UR1, and a sinus tract was present. Sensitivity testing with Hygenic® Endo-Ice® (Coltene) and electric pulp testing (SybronEndo Diagnostics Unit) revealed that the UR1 was the only non-vital incisor tooth.
Soft tissue examination revealed no buccal swelling, but the mucosa was tender over the apex of UR1, and a sinus tract was present. Sensitivity testing with Hygenic® Endo-Ice® (Coltene) and electric pulp testing (SybronEndo Diagnostics Unit) revealed that the UR1 was the only non-vital incisor tooth.
Paralleling periapical radiographs were exposed of the central incisor teeth using a Rinn Holder (Rinn, Dentsply), and all looked normal apart from the UR1. An attempt had been made to root fill the UR1, but the obturation material was significantly under-condensed in the apical third, and individual gutta-percha cones were visible.
The dentist obviously had difficulty managing the large immature canal. They may also not have had confidence fitting the rubber dam on a 12-year-old, increasing the potential for bacterial contamination of the root canal. The coronal restoration provided an inadequate seal. The root length of UR1 was significantly shorter than the UL1, and a large radiolucent area was present at the apex. No evidence of replacement resorption, inflammatory resorption, or any root fractures could be detected.
Diagnosis
Although there was history of trauma, the most likely cause of current symptoms and clinical findings was periapical periodontitis.
The root canal filling had most probably failed as a result of persistent bacterial infection in the root canal. The tooth had not undergone replacement or inflammatory resorption.
Treatment options
- Root canal retreatment and restoration with composite
- Extraction and replacement with a Maryland bridge or implant-supported crown
The prognosis for root canal retreatment should be good, and the patient could expect the tooth to remain functional for many years. Replacement at an early age with an implant may provide a good cosmetic result initially, but over a lifetime, the result would be difficult to predict.
Generally, well root-filled and restored teeth appear to function as well as single tooth implants and result in less costly repairs when things fail (Hannahan and Eleazer, 2008; Pennington, et al. (2009); Torebinejad, et al., 2007). The dark color of the tooth (and the main complaint of the patient) could be improved by:
- Internal bleaching
- Internal/external bleaching using trays
- Placement of a veneer in composite or porcelain
- Placement of a crown
Bleaching techniques are low risk and non-invasive (Zimmerli, Jeger, and Lussi, 2010). Bleaching would, therefore, be the preferred means of improving tooth color. Matching the texture and color of adjacent teeth with a porcelain or composite veneer on a single tooth would be esthetically challenging and preparation of a crown unjustifiably destructive. After discussion with the patient, an internal-bleaching technique was the option of choice.
Treatment
 Due to the history and chronicity of the infection, a two-visit strategy was adopted. This ensured adequate disinfection of the root canal and the possibility to confirm healing of the sinus tract before obturation.
Due to the history and chronicity of the infection, a two-visit strategy was adopted. This ensured adequate disinfection of the root canal and the possibility to confirm healing of the sinus tract before obturation.
Buccal infiltration of 4% articaine 1:100,000 adrenaline (Septodont) provided profound anesthesia, and the UR1 was isolated with latex rubber dam and a number one clamp.
Using an operating microscope, the existing filling was removed with a long-tapered diamond bur, and soft dentin (the result of microleakage) with a tunstgen carbide LN bur (Dentsply). This revealed a contaminated root canal containing poorly condensed gutta percha. The root filling was rapidly removed with Gates Glidden size 2 and Hedstroem file size 30 (Denstply). The loose gutta-percha points were washed out of the canal with sodium hypochlorite.
The apical foramen of the canal was large (greater than a size 40 file) and could be visualized through the operating microscope. The coronal access was refined, and a working length estimation made with an apex locator (Endo Analyzer, Sybron) and size 40 FlexoFile® (Dentsply Maillefer). A steady zero reading was achieved, and this was confirmed by direct sight.
Because the root had an immature morphology, there was no requirement for mechanical instrumentation. Instead, the canal was disinfected with a solution of heated 3% sodium hypochlorite (Teepol) irrigant, delivered using a safe-ended needle (Henry Schein®) bent short of the working length to prevent extrusion.
Disinfection was carried out over approximately 40 minutes. The sodium hypochlorite was agitated with a size 20 IRRISAFE™ ultrasonic tip (Satelec) and an EndoActivator® (Dentsply) with a blue tip. The solution was replenished every 2 minutes. A final sequence with 40% citric acid (Cerkamed) and 3% sodium hypo-chlorite completed irrigation.
The canal was dried with sterile paper points (Dentsply) and non-setting calcium hydroxide placed (Calasept®). The access was sealed with a cotton wool pellet at the level canal orifice, Cavit™ (3M ESPE) and Fuji IX (GC).
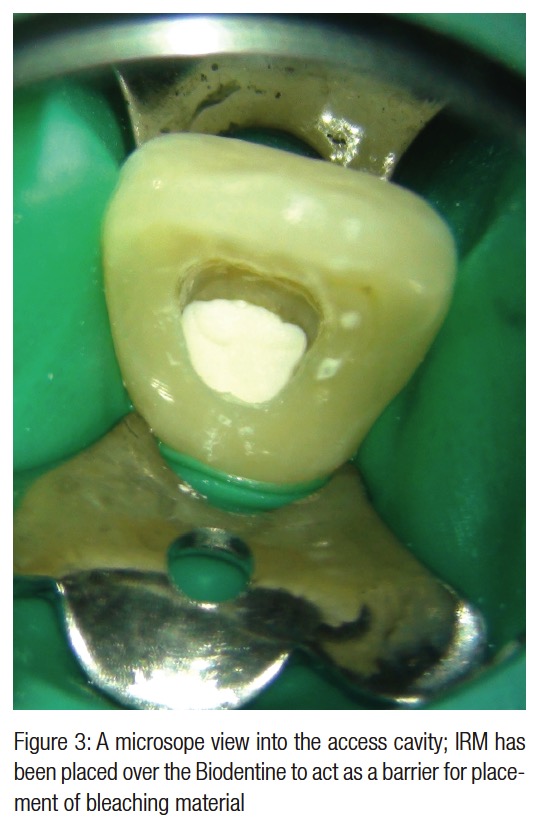
One week later, the sinus had healed, the tooth was symptom free, the canal dry, odor-free, and the tooth ready for obturation. The apical portion of the canal was sealed with Biodentine® (Septodont), packed into place using a Machtou plugger with the microscope providing direct vision. On top of this, a layer of IRM® (Dentsply) was placed. Endoperox (Septodont) internal whitening agent was mixed and packed into the access cavity. This was then sealed with Fuji IX compomer.
A week later, the tooth was reviewed. The tooth was symptom-free and the patient was happy with the color, so the access was permanently restored with Fuji IX, light-cured bulk fill composite SDR® (Smart Dentine Replacement, Dentsply) and Ceram-X™ Duo (Dentsply). The incisal tip was restored with Ceram-X duo.
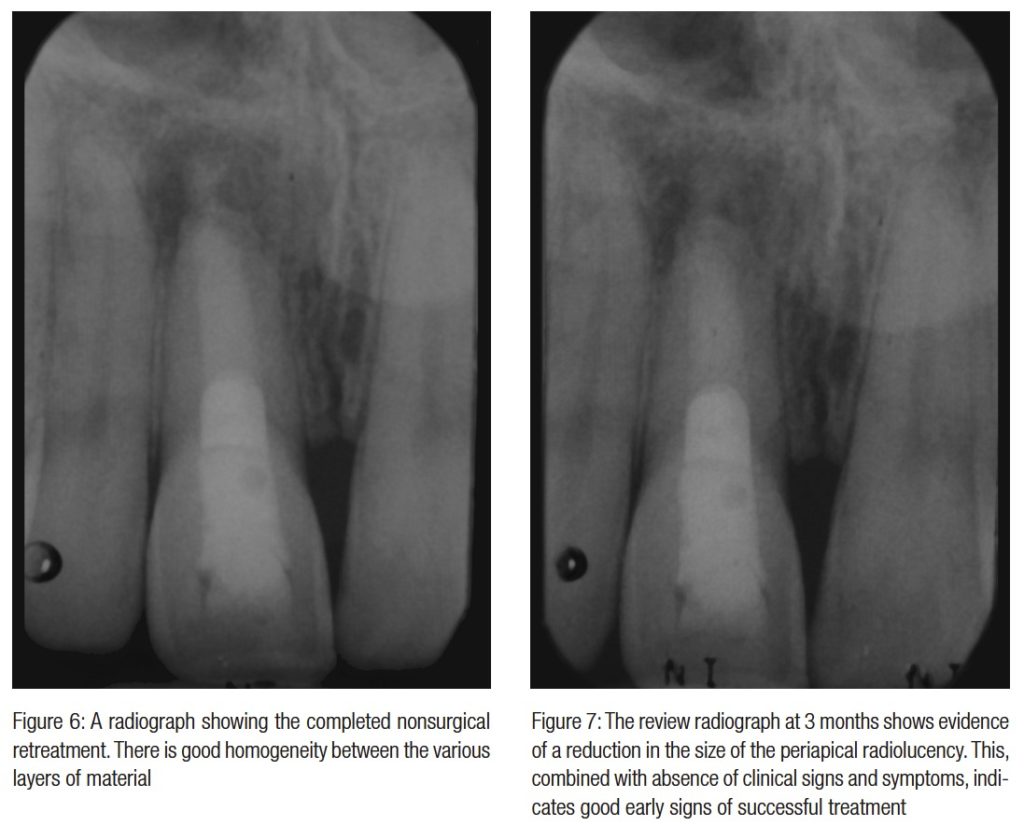
The tooth was reviewed at 3 months, when it was symptom and sign-free, and a paralleling radiograph showed good evidence of early bony healing at the apex.
A further review will be carried out at 1 year, and subsequently, at 2 years and 4 years.
Discussion
The International Association for Dental Traumatology (IADT) has produced guidelines for the management of traumatic injuries to teeth, available online as the Dental Trauma Guide (2010).
The recommended treatment for an enamel-dentin fracture is as follows:
- If a tooth fragment is available, it can be bonded to the tooth. Otherwise, perform a provisional treatment by covering the exposed dentin with glass-ionomer or a permanent restoration using a bonding agent and composite resin.
- The definitive treatment for the fractured crown is restoration with accepted dental restorative materials.
- Three angulations (periapical, occlusal, and eccentric exposures) should be used in the radiographic examination to rule out displacement or fracture of the root.
- Radiograph of lip or cheek lacerations to search for tooth fragments or foreign material.
- Follow-up — clinical and radiographic control at 6 to 8 weeks and 1 year.
The importance of checking adjacent teeth cannot be over emphasized as it is not uncommon for collateral damage to have occurred as a result of trauma.
Data from the dental trauma guide shows prognosis for an enamel-dentin fracture at 1 to 3 years to be very good, with the risk of pulp necrosis to be only extremely low. This suggests that the initial injury in this case may have been more severe. The root length of UR1 was shorter than UL1 and the root morphology immature, suggesting that root development had stalled shortly after injury.
Ravn (1981) evaluated the prognosis for permanent incisors with enamel-dentin fracture only and those with enamel-dentin fracture combined with other factors. Pulp death occurred in 3.2% of teeth with enamel-dentin fracture as the only damage. Enamel-dentin fracture and concussion resulted in pulpal necrosis in 5.8%, and cases involving both concussion and mobility showed pulpal necrosis in 30.1% of teeth.
Teeth with combined intrusion injuries would have a much higher incidence of pulp necrosis (67.6% at 1 year and 70.9% at 3 years), inflammatory root resorption approximately 35% at 1 and 3 years, and ankylosis 8.8% at 1 year, and 12.1% at 3 years (Diangelis, et al., 2012).
This confirms the requirement for meticulous examination of dental trauma cases and the potential risk of combined injuries. Compliance of the patient and parents to attend review is critical.
Limited volume, high resolution cone beam tomography can be useful in the assessment of trauma cases and the detection of resorption defects in endodontics. Evidence-based guidelines for the clinical use of CBCT, known as the European Commission Radiation Protection guidelines (SEDENTEXCT 2012), and those from the American Association of Endodontists (2011) both recommend that the need for a CBCT scan should always be assessed after a risk versus benefit analysis before each exposure.
In this case, the tooth had been traumatized 11 years earlier; it was not ankylosed and showed no sign of inflammatory resorption clinically or on radiograph. The risk of both following trauma is highest in the first 3 years (Diangelis, et al., 2012). It was therefore considered more likely that the tooth had become necrotic after injury, and the radiolucent area was the result of apical periodontitis; this was also confirmed by the presence of a sinus tract. The root canal was likely to be infected with bacteria so there was no indication to expose a CBCT scan at this stage.
It is important in root canal retreatment to remove the failed root canal filling material as efficiently as possible to allow disinfection of the root canal (Van Nieuwenhuysen, Aouar, and D’Hoore, 1994). During retreatment, the existing material and any obstructions and missed canals should be prepared and disinfected at the first visit.
Two-visit approach
Historically, it has been shown that mechanical preparation alone reduces the bacterial load in an infected root canal, according to Byström and Sundqvist, (1981), but sodium hypochlorite in a concentration of at least 1% is required to kill any remaining bacteria (1983). Sodium hypochlorite also dissolves necrotic pulp tissue. The bacteria are present in planktonic form and as a biofilm. The bacteria in biofilms are surrounded by matrix and can be difficult to remove.
The irrigant must therefore be agitated to break up these bacterial aggregations. Ultrasonic activation removes more debris form the root canal than syringe irrigation alone (Burleson, et al., 2007).
A solution of 17% EDTA or citric acid as a final rinse (Byström and Sundqvist, 1985) is used to remove smear and has a positive benefit on outcome in retreatment cases (Ng, Mann and Gulabivala, 2011).
In this case, the root canal had an immature morphology, and the terminal foramen was greater than a size 40 file. There was no requirement to carry out mechanical instrumentation as the canal was already sufficiently large to allow adequate irrigant interchange. Instead, the irrigant was activated with an ultrasonic tip, which was lightly brushed against the walls and oscillated passively in the lumen of the canal with the hope of inducing acoustic microstreaming (Ahmad, Pitt Ford, and Crum, 1987). The aim was to break up biofilm and remove contaminated surface layers of dentin.
Dressing the canals (after preparation and disinfection) with calcium hydroxide for 7 days was shown to be effective at producing bacteria-free canals and so evolved the concept of a two-visit strategy using a chemomechanical approach (Byström, Claesson, and Sundqvist, 1985; Sjögren, et al., 1991).
More recently, universal use of a two-visit approach has been questioned. Peters and colleagues (2002) concluded that a calcium hydroxide and sterile saline slurry limits but does not totally prevent regrowth of endodontic bacteria. Hargreaves in a systematic review of the literature reported that multiple visits with calcium hydroxide treatment did not improve upon clinical outcome, and there was a minimal level of evidence for considering one versus two appointments in nonsurgical endodontics (2006). Indeed, a single visit approach is used by many endodontists for many cases with no apparent repercussions for the patient nor reduced prognosis (Ng, Mann, and Gulabivala, 2011). However, not all cases are ideally suited to a single visit approach, and a two-visit strategy was adopted in this case to confirm resolution of the sinus tract before obturation and bleaching.
The immature root canal morphology can be challenging to obturate. Lateral condensation is difficult even with customized gutta-percha points, and excessive lateral pressure could potentially damage the thin root. Vertical compaction of gutta percha could result in extrusion of material unless a barrier or matrix is used at the terminal foramen. With the aid of an operating microscope, the terminus of the canal can often be visualized, and controlled placement of materials such as MTA (Dentsply) or Biodentine (Septodont) can be achieved. Bioceramics such as these have excellent sealing abilities and have many reported uses in endodontics, including management of open apices (Parirokh and Torabinejad, 2010). It was possible in this case to accurately place Biodentine without using a collagen matrix at the apex.
Tooth discoloration occurs as a result of the formation of chemically stable chromogenic products; these are oxidized during bleaching. Most discolorations can be reliably bleached apart from those that result from metal ions (Plotino, et al., 2008).
Tooth whitening following root canal treatment can be carried out using an internal bleaching technique (walking technique) with materials such as sodium perborate, or carbamine peroxide sealed in the access cavity (Zimmerli, Jeger, and Lussi, 2010), or via an internal/external approach with carbamine peroxide solutions (Poyser, Kelleher, and Briggs, 2004). According to Carraso and colleagues, carbamide peroxide has been shown to have the best penetration into dentin (2003) and the walking technique a better outcome than in-office bleaching (Dietschi, Rossier, and Krejci, 2006). The internal/external technique requires the fabrication of bleaching trays, and the access cavity can become contaminated with food particles and debris during use.
Endodontic bleaching has been cited as a possible cause of external cervical resorption (Heithersay, 1999); however, the eiology of this condition is not entirely clear. Defects in the cementum layer could potentially allow hydrogen peroxide from the pulp chamber to reach the external root surface and induce an inflammatory response (Rotstein, Torek, and Misgav, 1991). Subsequent damage to the periodontium could therefore result in cervical resorption. Avoiding placement of internal bleaching agents below the cemento-enamel junction, checking for cervical lesions, and not using heat should prevent external cervical resorption (Patel, Kanagasinam, and Pitt Ford, 2009).
 After checking to make sure that there were no cervical defects, intermediate restorative material was placed over the gutta-percha root filling material and at the cervical level of the root canal. Sodium perborate mixed with water is considered safer than hydrogen peroxide as an intracoronal bleaching agent, and 35% carbamide peroxide (urea peroxide) combines the safety of sodium perborate together with the efficacy of 35% hydrogen peroxide (Lim, 2004).
After checking to make sure that there were no cervical defects, intermediate restorative material was placed over the gutta-percha root filling material and at the cervical level of the root canal. Sodium perborate mixed with water is considered safer than hydrogen peroxide as an intracoronal bleaching agent, and 35% carbamide peroxide (urea peroxide) combines the safety of sodium perborate together with the efficacy of 35% hydrogen peroxide (Lim, 2004).
In this case, an internal bleaching technique was used with a commercially available material — Endoperox (Septodont), a carbamine peroxide material.
The case was reviewed at 3 months and will continue to be reviewed at 1 year, 2 years, and 4 years posttreatment (European Society of Endodontology, 2006).
Conclusion
This case highlights the management and diagnosis of periapical periodontitis in a tooth that suffered dental trauma 11 years previously. Nonsurgical micro-endodontic techniques were used to retreat the immature root morphology. No mechanical instrumentation was required, and the immature root was sealed with Biodentine. Internal bleaching as a non-invasive means of restoring natural color was demonstrated in this non-vital tooth.
References
1. Ahmad M, Pitt Ford TJ, Crum LA (1987) Ultrasonic debridement of root canals: acoustic streaming and its possible role. J Endod. 1987;13(10):490-499. 2. American Association of Endodontists and American Academy of Oral and Maxillofacial Radiology. Use of cone-beam computed tomography in endodontics Joint Position Statement of the American Association of Endodontists and the American Academy of Oral and Maxillofacial Radiology. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 2011;111(2), 234-237. 3. Burleson A, Nusstein J, Reader A, Beck M. The in vivo evaluation of hand/rotary/ultrasound instrumentation in necrotic human mandibular molars. J Endod. 2007;33(7):782-787. 4. Byström A, Claesson R, Sundqvist G. The antibacterial effect of camphorated paramonochlorophenol, camphorated phenol and calcium hydroxide in the treatment of infected root canals. Endod Dent Traumatol. 1985;1(5):170-175. 5. Byström A, Sundqvist G. Bacteriologic evaluation of the efficacy of mechanical root canal instrumentation in endodontic therapy. Scand J Dent Res. 1981;89(4): 321-328. 6. Byström A, Sundqvist G. Bacteriologic evaluation of the effect of 0.5 percent sodium hypochlorite in endodontic therapy. Oral Surg Oral Med Oral Pathol. 1983;55(3):307-312. 7. Byström A, Sundqvist G. The antibacterial action of sodium hypochlorite and EDTA in 60 cases of endodontic therapy. Int Endod J. 1985;18(1):35-40. 8. Carrasco LD, Froner IC, Corona SA, Pecora JD. Effect of internal bleaching agents on dentinal permeability of non-vital teeth: qualitative assessment. Dent Traumatol. 2003;19(2): 85-89. 9. Diangelis AJ, Andreasen JO, Ebeleseder KA, Kenny DJ, Trope M, Sigurdsson A, Andersson L, Bourguignon C, Flores MT, Hicks ML, Lenzi AR, Malmgren B, Moule AJ, Pohl Y, Tsukiboshi M. International Association of Dental Traumatology guidelines for the management of traumatic dental injuries: 1. Fractures and luxations of permanent teeth. Dent Traumatol. 2012;28(1):2-12. 10. Dietschi D, Rossier S, Krejci I. In vitro colorimetric evaluation of the efficacy of various bleaching methods and products. Quintessence Int. 2006;37(7): 515-526. 11. European Society of Endodontology. Quality guidelines for endodontic treatment: consensus report of the European Society of Endodontology. Int Endod J. 2006;39(12):921–930. 12. General Dental Council (2013) Standards for the Dental Team. [Online]. Available at: <https://bit.ly/1avam3q> [Accessed: April, 2015]. 13. Hannahan JP, Eleazer PD. Comparison of success of implants versus endodontically treated teeth. J Endod. 2008;34(11):1302–1305. 14. Hargreaves KM. Single-visit more effective than multiplevisit root canal treatment? Evid Based Dent. 2006;7(1): 13–14. 15. Heithersay GS. Invasive cervical resorption: an analysis of potential predisposing factors. Quintessence Int. 1999;30(2):83-95. 16. International Association of Dental Traumatology, Rigshospitalet Denmark (2010) The Dental Trauma Guide. [Online]. Available at: <https://www.dentaltraumaguide. org> [Accessed March, 2015] 17. Lim KC. Considerations in intracoronal bleaching. Aust Endod J. 2004;30(2):69-73. 18. Ng YL, Mann V, Gulabivala K. A prospective study of the factors affecting outcomes of nonsurgical root canal treatment: part 1: periapical health. Int Endod J. 2011;44(7):583-609. 19. Parirokh M, Torabinejad M. Mineral Trioxide Aggregate: a comprehensive literature review — Part III: clinical applications, drawbacks, and mechanism of action. J Endod. 2010;36(3):400-413. 20. Patel S, Kanagasingam S, Pitt Ford T. External cervical resorption: a review. J Endod. 2009;35(5):616-625. 21. Pennington MW, Vernazza CR, Shackley P, Armstrong NT, Whitworth JM, Steele JG. Evaluation of the costeffectiveness of root canal treatment using conventional approaches versus replacement with an implant. Int Endod J. 2009;42(10) 874-883. 22. Peters LB, van Winkelhoff AJ, Buijs JF, Wesselink PR. Effects of instrumentation, irrigation and dressing with calcium hydroxide on infection in pulpless teeth with periapical bone lesions. Int Endod J. 2002;35(1):13-21. 23. Plotino G, Buono g, Grande NM, Pameijer CH, Somma F. Nonvital tooth bleaching: a review of the literature and clinical procedures. J Endod. 2008;34(4): 394-407. 24. Poyser NJ, Kelleher MG, Briggs PF. Managing discoloured non-vital teeth: the inside/outside bleaching technique. Dent Update. 2004;31(4):204-210, 213-214. 25. Ravn JJ. Follow-up study of permanent incisors with enamel-dentin fractures after acute trauma. Scand J Dent Res. 1981;89(5):355-365. 26. Rotstein I, Torek Y, Misgav R. Effect of cementum defects on radicular penetration of 30% H2O2 during intracoronal bleaching. J Endod. 1991;17(5):230-233. 27. SEDENTEXCT (2012) European Commission. Radiation Protection No 172: Cone beam CT for dental and maxillofacial radiology (Evidence based guidelines). [Online]. Available at: https://www.sedentexct.eu/files/radiation_ protection_172.pdf [Accessed April, 2015]. 28. Sjögren U, Figdor D, Spångberg L, Sundqvist G. The antimicrobial effect of calcium hydroxide as a short-term intracanal dressing. Int Endod J. 1991;24(3): 119–125. 29. Torabinejad M, Anderson P, Bader J Brown LJ, Chen LH, Goodacre CJ, Kattadiyil MT, Kutsenko D, Lozada J, Patel R, Petersen F, Puterman I, White SN. Outcomes of root canal treatment and restoration, implant-supported single crowns, fixed partial dentures and extraction without replacement: a systematic review. J Prosthet Dent. 2007;98(4):285-311. 30. Van Nieuwenhuysen JP, Aouar M, D’Hoore W. Retreatment or radiographic monitoring in endodontics. Int Endod J. 1994;27(2):75-81. 31. Zimmerli B, Jeger F, Lussi A (2010) Bleaching of Non-vital teeth. A clinically relevant review. Schweiz Monatsschr Zahnmed. 2010;120(4):306-320.
Stay Relevant With Endodontic Practice US
Join our email list for CE courses and webinars, articles and more..


