Editor’s intro: Drs. Andrea Polesel and Arnaldo Castellucci use CBCT and nonsurgical treatment to promote conservative preservation of two maxillary incisors. Read about their aims and outcomes.
Drs. Andrea Polesel and Arnaldo Castellucci show successful combined nonsurgical-surgical endodontic retreatment aided by CBCT
Abstract
The aim of this article is to present the conservative preservation of two maxillary incisors with uncommon root anatomies (dens invaginatus). The first case shows the retreatment, an apical plug of an extra large foramen (gauging 300), the subsequent endodontic surgery and healing of a lesion in a lateral incisor, with a 4-year recall. The patient presented in emergency with a sinus tract and an access cavity prepared 10 years previously. The cone beam computed tomography (CBCT) showed a large lesion, an extra large foramen, and unique anatomy. After the orthograde retreatment, an apicoectomy with retrograde obturation in mineral trioxide aggregate (MTA) was performed. The second case shows an apical plug with MTA in a central incisor with unusual root anatomy. The 8-year-old patient presented with an acute alveolar abscess. MTA was used to seal the main central canal and cap the pulp exposure of the distal canal. A radiographic recall after 14 years is shown.
The aim of this article is to present the conservative preservation of two maxillary incisors with uncommon anatomies (dens invaginatus).
- First case, lateral incisor: retreatment, apical plug of large foramen (gauging 300), surgery, and healing.
- Second case, central incisor: apical plug and cap with MTA and 14-year recall.
Introduction
Dens invaginatus is a rare malformation of teeth described first in a human tooth by a dentist called Socrates in 1856. It demonstrates a low incidence and a prevalence of 43% in the maxillary lateral incisors.1 Dens invaginatus is a developmental anomaly that results in an enamel-lined cavity intruding into the crown or root before the mineralization phase.2 The crown and root canal anatomical variations associated with the dens invaginatus are so numerous that it is very difficult to describe a classification. The first classification of invaginated teeth was proposed by Hallett in 1953,3 but the most commonly used classification was proposed by Oehlers,4 who described three subtypes, which are based on the extent of apical migration of an enamel-lined invagination. Schulze and Brand5 proposed a more detailed classification. The most common clinical finding associated with dens invaginatus is early pulpal involvement, which is explained by the existence of canals extending from the invagination into the pulp.6
Endodontic treatment of a tooth with dens invaginatus is considered a potentially complicated procedure. A survey of 307 Flemish dentists showed that if a tooth with dens invaginatus requires endodontic treatment, 38.4% of them will refer the patient to a specialist.7
The introduction of cone beam computed tomography (CBCT) has improved the diagnosis, the therapy, and the prognosis in many fields of dentistry. Endodontics has been the specialty that received the most important advantages from three-dimensional radiography, especially in a case of anatomical variations, traumatic injuries, complex retreatments, difficult differential diagnosis, and endodontic surgery. CBCT imaging in endodontics allows for three-dimensional evaluation of the external and internal anatomy.8 The success of endodontic treatment in teeth with complex internal anatomy depends on the use of CBCT and dental operating microscope.9
The following case report presents successful combined nonsurgical-surgical endodontic retreatment of a maxillary lateral incisor with dens invaginatus anatomy with the aid of CBCT.

Case report 1
A 22-year-old male patient was referred for evaluation and possible treatment of the left maxillary lateral incisor (tooth No. 10). He presented to the dental office complaining of symptoms with several episodes of swelling in the left anterior maxilla and a bad taste in the mouth. The patient reported a previous endodontic treatment in a maxillary left lateral incisor about 10 years previously. The root canal treatment had been initiated, but not completed, by the general dentist, and the tooth had been left open. The patient’s medical history was noncontributory.
At the intraoral examination, a sinus tract was noted in the buccal periapical area of the maxillary left lateral incisor (Figure 1). The tooth showed an access cavity on the palatal side and a crown larger than the maxillary right lateral incisor. A panoramic radiograph, taken by the general dentist who referred the patient, and the periapical radiograph revealed a dens invaginatus and a periapical lesion involving especially the mesial part of the root (Figures 2A and 2B). Circumferential periodontal probing did not reveal pockets exceeding 2 mm around the tooth. In order to ascertain the variations of the root canal system, a CBCT scan was performed. Informed consent was obtained from the patient, and a multislice CBCT was taken with a Carestream CS81003D scanner (Carestream, Rochester, New York), and 3D-reconstruction images were obtained. A small field of view (FOV), 4 cm per 4 cm, was chosen. The images demonstrated the presence of a dens invaginatus with three main canals: a mesial, a middle, and a distal canal. They revealed also the presence of a periradicular lesion extending on the mesial side of the root and a very large foramen (3 mm) (Figures 3A-3D). A treatment plan with a combined root canal retreatment (orthograde and surgical) was proposed, and an informed consent was taken.
At the first treatment visit after isolation of the operating field with rubber dam, an access cavity was prepared and finished using an operating microscope (Leica, Switzerland); the coronal interferences were removed using burs and ultrasonic tips Start-X 2 and 3 (Dentsply Maillefer, Baillagues, Switzerland); and the root canal system was negotiated with K-files (Dentsply Maillefer). The mesial canal was thinner with a calcified canal, and scouting was obtained with C+ Files (Dentsply Maillefer).
The irrigation was improved by using a sonic handpiece, EndoActivator® (Dentsply Maillefer). The anatomy found during scouting confirmed the anatomic anomalies revealed in the 3D radiograph with a thin mesial canal and two larger canals: one distal and one in the middle of the root. The root canal system was shaped, cleaned, medicated with calcium hydroxide, and temporarily coronally sealed with Cavit® and a glass ionomer cement (Stomidros Stomygen, Funo, Italy, and Ionolux Voco, Cuxhaven, Germany) (Figures 4A-4C).
 Two weeks later the patient returned, reporting that he felt better, but the sinus tract was still present. During the second visit, the rubber dam was placed, temporary access filling removed, and the medication removed; the root canal system was cleaned, shaped, and obturated. The key steps of the shaping were obtained by using a No. 10 K-file for scouting, PathFile® 1, 2, 3 (Dentsply Maillefer) to obtain the glide path and ProTaper Next™ nickel-titanium rotary instruments (Dentsply Maillefer) for final shaping.
Two weeks later the patient returned, reporting that he felt better, but the sinus tract was still present. During the second visit, the rubber dam was placed, temporary access filling removed, and the medication removed; the root canal system was cleaned, shaped, and obturated. The key steps of the shaping were obtained by using a No. 10 K-file for scouting, PathFile® 1, 2, 3 (Dentsply Maillefer) to obtain the glide path and ProTaper Next™ nickel-titanium rotary instruments (Dentsply Maillefer) for final shaping.
A radiograph with the instruments at the working length was obtained. During scouting, EDTA gel (RC-Prep; Premier Dental Products, Norristown, Pennsylvania) was used as a lubricant, and irrigation was performed with 5% sodium hypochlorite at each change of file. The irrigating solutions were delivered with a 30-G open-ended needle (NaviTip™; Ultradent, South Jordan, Utah) and activated after finishing shaping by using a sonic device, Endo-Activator (Dentsply Maillefer). A rinse with 17% EDTA for 1 minute and a final flush with 5% hypochlorite were performed at the end of instrumentation. The root canal system was dried with paper points and obturated with two different techniques. The mesial canal was obturated with a gutta-percha cone X3 (Dentsply Maillefer), Pulp Canal Sealer™ EWT (Kerr Corp., Orange, California) and the vertical compaction of warm gutta-percha. The middle and the distal canals were sealed with ProRoot® MTA (Dentsply Tulsa Dental, Tulsa, Oklahona), using a carrier (MAP One System, Produits Dentaires) to place the material at the apical foramen and a Thermafil plastic carrier (number 80 in the middle canal and number 50 in the distal canal) in order to adapt it more precisely in the apical third, preventing the voids.
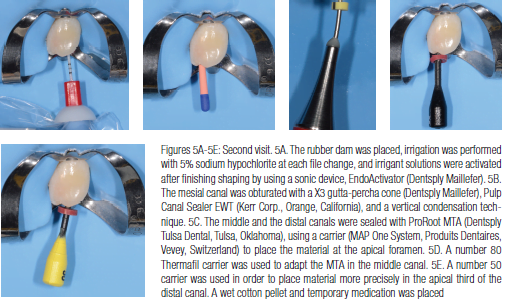

A wet cotton pellet and a temporary access filling was placed (Figures 5A-5E). Two weeks later during the third visit after rubber dam isolation of the operating field, the temporary obturation was removed, the setting of the MTA was checked, the coronal third of each canal was obturated with warm gutta percha, and an adhesive direct composite restoration was performed10 (Figure 6) (Optibond™ FL Kerr, Scafati, Italy; Enamel Plus Micerium, Avegno, Italy).
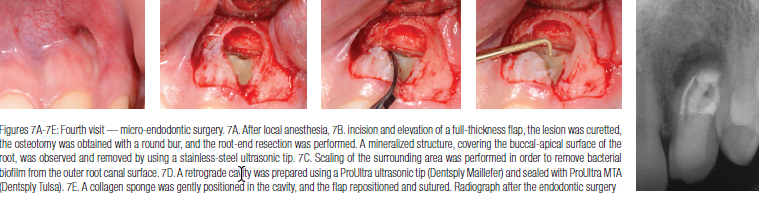
The patient was symptom-free, but the sinus tract was still present. Surgical endodontic retreatment was indicated. After local anesthesia, incision, and elevation of a full-thickness flap, the lesion was curetted, osteotomy was obtained with a round bur, and root-end resection was performed. A mineralized structure, covering the buccal-apical surface of the root, was observed and removed by using a stainless-steel ultrasonic tip. The scaling of the surrounding area was performed in order to remove any bacterial biofilm from the outer root canal surface. A retrograde cavity was prepared by using a ProUltra® ultrasonic tip (Dentsply Maillefer) and sealed with ProUltra® MTA (Dentsply Tulsa). A collagen matrix was gently positioned in the cavity, and the flap repositioned and sutured (Figures 7A-E) with Ethicon® polyamide monofilament 6-0, (Johnson & Johnson Medical NV Belgium) Postoperative instructions were given to the patient.
The patient was recalled for subsequent clinical and radiographic evaluation. During the first follow-up after 3 months, the sinus tract had resolved and was not present. The patient was symptom-free, and the periapical radiograph showed an appreciable decrease in the size of the lesion (Figure 8). After 2 years, the inspection showed the complete healing of the sinus tract (Figure 9), and the periapical radiograph revealed healing of the lesion with healthy periapical and periodontal tissues in a symptom-free patient (Figure 10).

Case report 2
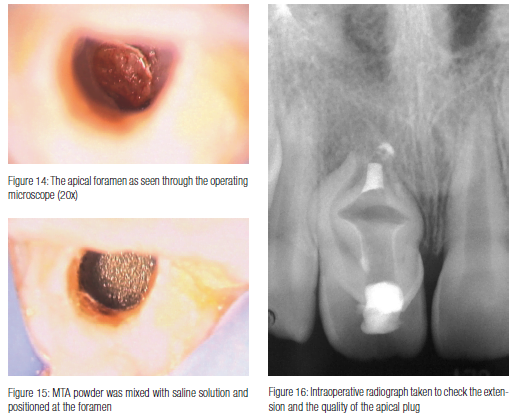
An 8-year-old female patient presented with an acute alveolar abscess in the maxillary right central incisor (Figure 11). The preoperative radiograph showed a periapical radiolucency, an unusual anatomy (dens invaginatus), with a main central canal and a wide open apex (Figure 12). During the first visit after placement of the rubber dam and preparation of an adequate access cavity, the root canal system was cleaned with copious irrigation with sodium hypochlorite. The root canal system was cleaned more than shaped in order not to increase the fragility of the dental structure. To improve disinfection and to raise the level of pH, the main central root canal was medicated with calcium hydroxide (Figure 13). One week later after removal of the intracanal medication, the root canal was irrigated with 5% sodium hypochlorite and dried with sterile paper points. By using an operative microscope, the apical foramen (Figure 14) was sealed with an apical plug of MTA, 3-mm thickness. MTA powder was mixed with saline solution and positioned exactly at the foramen (Figure 15) by using a Dovgan carrier (Dovgan, Vista Dental Products, Racine, Wisconsin). The material was adapted in direct contact with periapical tissues without overfilling. A thin layer of MTA was used for a direct pulp capping of the pulp exposure of the distal canal. An intraoperative radiograph was taken to check the extension of the apical plug (Figure 16). A wet paper point was introduced in the root canal for the setting of the apical plug, a cotton pellet was positioned in the pulp chamber in contact with the MTA, and the access cavity was sealed with a temporary obturation.

During the third visit, the rubber dam was placed; the temporary restoration, the paper point, and the cotton pellet were removed; the MTA setting was checked with an endodontic probe; and the rest of the root canal system was filled with thermoplastic gutta percha (Figure 17). The access cavity was sealed with a direct adhesive composite restoration. The radiographic recall at 2 years (Figure 18) and 14 years (Figure 19) demonstrated healthy periodontal and periapical tissues in a symptom-free patient.
Discussion
The success in endodontic complex cases depends on several factors: the experience and the skill of the clinician, the presence of specific instruments, and the respect of clinical protocols. In this case, it was very important to save the natural tooth because of the young age of the patient and the esthetic implications. The key factors for the resolution of this case can be summarized in some key points.
- 3D radiography is mandatory in order to analyze the shape of the dens invaginatus, its internal anatomy, and the diameter of the foramen, and to evaluate the dimensions of the lesion. Many recent articles in the literature report the clinical advantages of the CBCT in the management of complex anatomies11,12 and dens invaginatus.2 The international guidelines give precise indications for the use of the CBCT.13,14 In this case, two clinical conditions indicated the use of a 3D radiograph: a dens invaginatus with complex root and canal anatomy and a surgical endodontic retreatment in the treatment plan. A small field of view (FOV) was chosen in order to reduce the dose of the ionizing radiation, to reduce the area of responsibility, and to increase the resolution.15
- The dental operating microscope is mandatory in order to analyze and treat the root canal system during an orthograde and surgical approach. It has been shown that its use could help in locating additional canals during endodontic treatment,16 improving treatment accuracy and expediting treatment.17 The microscope provides a high level of magnification and illumination, essential factors in managing a very complex anatomy. Another fundamental instrument to perform a precise apical plug is the carrier, used to position the material exactly at the foramen. Selection of specific instruments is a crucial factor, but not enough to obtain success.
- Cleaning is a key factor for a good prognosis of invaginated treated teeth. The large and irregular volume of the root canal system makes proper shaping and cleaning difficult. Irrigation supported by ultrasonic cleaning has been described as an efficient means of disinfection18 and has been recommended for cleaning of the complex morphology of the root canal system in teeth with dens invaginatus.19
- A combined nonsurgical-surgical approach is mandatory to resolve the case. The most common difficulties encountered with management of dens invaginatus include inadequacies with biomechanical cleaning and three-dimensional obturation of the dysmorphic root architecture and the frequent lack of an apical and/or periradicular canal constriction, leading to potentially excessive overextension of the root filling material.20 The literature reports the healing of lesions in dens invaginatus after a surgical approach in most cases. The presence of an extra large, foramen ovale, visualized and measured 3-mm diameter in the 3D radiograph, is an anatomical complication very difficult to handle in orthograde retreatment. MTA is the elective material in order to seal large apical foramina with nonsurgical and surgical approaches.21
- The management of an extraradicular infection is another crucial factor to obtain healing of lesions and symp Apical periodontitis is a disease caused by bacterial infection of the root canal system. The infection is usually restricted to the intraradicular space, but occasionally, it can spread to the extra-radicular space. In some cases, the cause of symptoms was associated with the presence of extraradicular biofilms. In other cases, areas of mineralization with a calculus-like appearance were found on the external surface of the roots.22 In this clinical case, the extraradicular contamination was clearly present on the outer buccal root surface. A calculus-like structure could be appreciated in the apical third. Long-standing sinus tracts may function as a route of communication between the periradicular area and the external environment, permitting the passage of minerals and salts from the oral fluids into the apical periodontitis lesion.23 In this case, a double source of contamination (through the sinus tract and through the access cavity) could be the reason of the extraradicular infection. The removal of the calculus and the scaling of the surrounding area with stainless-steel ultrasonic tip are two essential steps of the endodontic surgery.
Saving the natural tooth is the first choice in dentistry, especially in young patients and esthetic areas. The advanced technology, the operating microscope, ultrasonics, CBCT, and mineral trioxide aggregate (MTA) are essential instruments and materials to treat extra large foramina. A proper diagnosis, the isolation of the operative field, the respect of the basic principles in cleaning, shaping and obturating the root canal system, and the anatomical and biological knowledge are the key factors to obtain predictable results in heavily compromised teeth. On the other side, experience, common sense, and the skill of the clinician are able to increase the long-term success in endodontic complex cases.
Editor’s call to action
Besides this article on CBCT imaging and nonsurgical treatment, Dr. Nestor Cohenca also discussed the growing popularity of 3D imaging in his article here. https://endopracticeus.com/industry-news/technology/join-the-80-cbct-and-endodontics/
2. Vier-Pellisier FV, Pellisier A, Recuero LC, et al. Use of cone beam computed tomography in the diagnosis, planning and follow up of a type III dens invaginatus case. Int Endod J. 2012;45:198-208.
3. Hallett GE. The incidence, nature, and clinical significance of palatal invagination in the maxillary incisor teeth. Proc R Soc Med. 1953;46(7):491-499.
4. Oehlers FA. Dens invaginatus (dilated composite odontome). I. Variations of the invagination process and associated anterior crowns forms. Oral Surg Oral Med Oral Pathol. 1957;10(11):1204-1218.
5. Schulze C, Brand E. Dens invaginatus (dens in dente). ZWR. 1972;8:569-660.
6. Rotstein I, Stabholz A, Heling I, Friedman S. Clinical considerations in the treatment of dens invaginatus. Endod Dent Traumatol. 1987;3(5):249-254.
7. Hommez GM, De Moor RJ, Braem M. Endodontic treatment performed by Flemish dentists. Part 2. Canal filling and decision-making for referrals and treatment of apical periodontitis. Int Endod J. 2003;36(5):344-351.
8. Cotton TP, Geisler TM, Holden DT, Schwartz SA, Schindler WG.. Endodontic application of cone-beam volumetric tomography. J Endod. 2007;33(9):1121-1132.
9. Nosrat A, Schneider C. Endodontic management of a maxillary lateral incisor with 4 root canals and a dens invaginatus tract. J Endod. 2015;41(7):1167-1171.
10. Polesel A. Restoration of the endodontically treated posterior tooth. Giornale Italiano di Endodonzia. 2014;28(1):2-16.
11. Byun C, Kim C, Cho S, et al. Endodontic treatment of an anomalous anterior tooth with the aid of a 3-dimensional printed physical tooth model. J Endod. 2015;41(6):961-965.
12. Cunha RS, Junaid A, Mello I. Unilateral fusion of a supernumerary tooth to a maxillary permanent lateral incisor: a report of a rare case. J Endod. 2015;41(3):420-423.
13. Special Committee to Revise the Joint AAE/AAOMR Position Statement on Use of CBCT in Endodontics. AAE and AAOMR Joint Position Statement. Use of the Cone Beam Computed Tomography in Endodontics 2015 Update. Oral Surg Oral Med Oral Pathol Oral Radiol. 2015;120(4):508-512.
14. European Society of Endodontology developed by Patel S, Durack C, Abella F, et al. European Society of Endodontology position statement: the use of CBCT in endodontics. Int Endod J. 2014;47(6):502-504.
15. Barnett F. Cone Beam Computed Tomography in Endodontics. Summer 2011 ENDODONTICS: Colleagues for Excellence. Chicago, IL: American Association of Endodontics and AAE Foundation.
16. Perrin P, Neuhaus KW, Lussi A. The impact of loupes and microscopes on vision in endodontics. Int Endod J. 2014;47(5):425-429.
17. Bowers DJ, Glickman GN, Solomon ES, He J. Magnification’s effect on endodontic fine motor skills. J Endod. 2010;36(7):1135-1138.
18. Cunningham W, Martin H, Pelleu G, Stoops D. A comparison of antimicrobial effectiveness of endosonic and hand root canal therapy. Oral Surg Oral Med Oral Pathol. 1982;54:238-241.
19. Skoner JR, Wallace JA. Dens invaginatus: another use for the ultrasonics. J Endod. 1994;20(3):138-140.
20. Brooks JK, Ribera MJ. Successful nonsurgical endodontic outcome of a severely affected permanent maxillary canine with dens invaginatus Oehlers Type 3. J Endod. 2014;40(10):1702-1707.
21. Parirokh M, Torabinejad M. Mineral trioxide aggregate: a comprehensive literature review — Part III: Clinical applications, drawbacks, and mechanism of action. J Endod. 2010;36(3):400-413.
22. Ricucci D, Siqueira JF Jr. Biofilm and apical periodontitis: study of prevalence and association with clinical and histopathologic findings. J Endod. 2010;36(8):1277-1288.
23. Ricucci D, Candeiro GTM, Bugea C, Siqueira JF Jr. Complex apical intraradicular infection and extraradicular mineralized biofilms as the cause of wet canals and treatment failure: report of 2 cases. J Endod. 2016;42(3):509-515.
Stay Relevant With Endodontic Practice US
Join our email list for CE courses and webinars, articles and more..

