CE Expiration Date: June 21, 2027
CEU (Continuing Education Unit):2 Credit(s)
AGD Code: 070
Educational aims and objectives
This self-instructional course for dentists aims to identify the various uses of the dental laser in endodontic practice.
Expected outcomes
Endodontic Practice US subscribers can answer the CE questions by taking the quiz online to earn 2 hours of CE from reading this article. Correctly answering the questions will demonstrate the reader can:
- Identify some of the challenges of root canal therapy that may not be effectively addressed by traditional treatment.
- Realize the efficiencies of the laser in the processes of irrigation and disinfection.
- Identify other protocols besides RCT for which the laser can be an effective tool.
Dr. Fernando Meza outlines the benefits that lasers can bring to endodontic procedures.
Dr. Fernando J. Meza discusses uses of lasers in the endodontic practice
Efficient endodontic interventions are crucial for maintaining dental wellness and securing the lasting integrity of natural teeth. Root canal therapies, a prevalent endodontic solution undergone by over half of the world’s population, according to a study titled “Prevalence of root canal treatment worldwide: A systematic review and meta-analysis,” are tailored to rectify concerns within the dental pulp, to alleviate discomfort and avert additional issues.1 Despite the annual treatment of over 15 million root canals as reported by the American Association of Endodontists, dental experts face a myriad of complexities in endodontic procedures, highlighting the significance of precise and innovative treatment methodologies.2
Difficulties linked with conventional endodontic treatments commonly center on attaining comprehensive disinfection of the root canal network and securely sealing the treated tooth to forestall recontamination. The complex structure of root canals, characterized by their curved and confined pathways, presents a notable challenge for achieving thorough cleansing and shaping, even for seasoned practitioners. Furthermore, the presence of microbes within the root canal system necessitates a meticulous and holistic strategy to eradicate bacteria and forestall the resurgence of infection.
In addressing these hurdles, the adoption of dental laser technology has brought about a revolutionary shift, enhancing the availability of high-quality care. Through leveraging laser energy, various dental procedures are executed with unmatched precision and effectiveness, thereby enhancing the standard of our treatments. Laser technology enables pinpoint targeting and elimination of infected tissue, debris, and bacteria from the complex root canal system, even in the most intricate anatomical arrangements. Such precision significantly reduces the likelihood of complications and enhances the overall success rates of endodontic interventions.
Beyond their efficacy in cleaning and disinfection, dental lasers offer advantages in terms of patient comfort and recovery — the minimally invasive nature of laser-based endodontic treatments results in less postoperative pain and faster healing times.3 Patients experience reduced discomfort during and after the procedure, contributing to a more positive dental experience.
As we delve into the advantages of dental lasers in root canal treatment, it becomes evident that their versatility extends beyond traditional endodontic approaches leading to more conservative applications in certain instances. For example, the laser can be employed to assist with pulp tissue ablation, pulpal hemostasis, and decontamination of infected dentin in direct and indirect pulp cap procedures. This type of procedure may be useful in younger patients presenting with carious lesions with asymptomatic irreversible pulpitis where the pulpal tissue is more resilient.
Paradigm shift: lasers versus traditional drills
Traditional endodontic procedures, while successful, pose concerns as the intricacies of the treatment process often make it time-consuming for both the clinician and the patient. The need for multiple visits may be decreased since laser-assisted endodontics offers efficiencies in the search for difficult-to-find calcified canals and difficult to disinfect complex anatomies. More often than not, laser-assisted endodontics provides a more predictable one-visit treatment which is an advantage for both the patient and the provider.
Leveraging the principles of cavitation and acoustic streaming, dental lasers have demonstrated a remarkable improvement in disinfection efficacy. Recognizing the potential for better outcomes, and the superiority of lasers in terms of cleanliness and disinfection, I found it imperative to incorporate laser technology into our practice with the Waterlase iPlus™.4
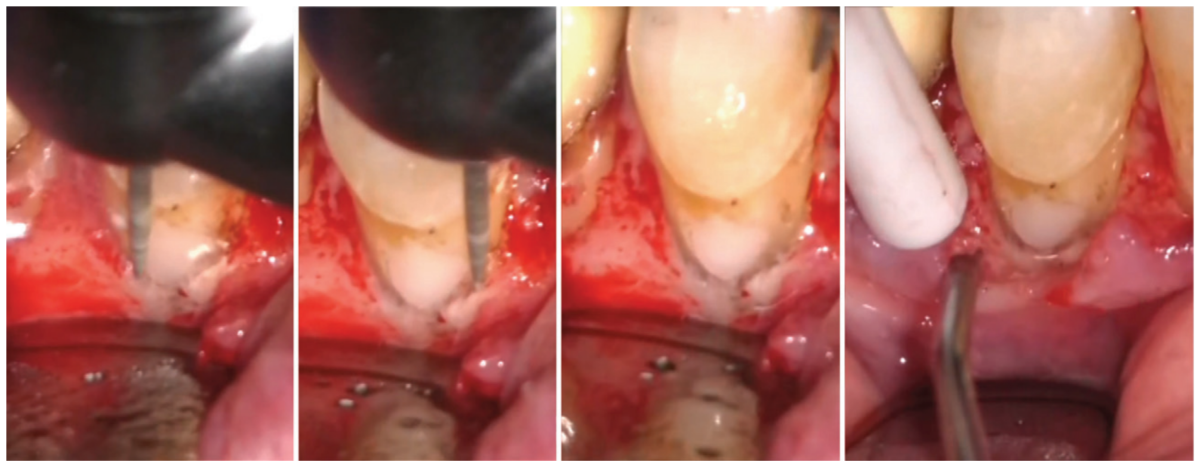
the class V subcrestal Geristore restoration. Additional images show a polished restoration with
full-thickness flap reflected
Since adopting the laser over 3 years ago, the advanced technology has surpassed our expectations. Beyond the evident improvements in cleaning and disinfecting canals, the technical aspects of the procedure have become more manageable. Laser activation of irrigants plays a pivotal role by efficiently removing debris, facilitating easier access for instruments to reach targeted areas within the tooth. This dual benefit has not only streamlined our process, making it more straightforward but also elevates the overall quality of disinfection for the patient. Incorporating the laser has resulted in shorter visits, in terms of time spent in the chair, and the possibility of reducing the number of required visits, which has demonstrated the efficiency brought about by laser-assisted root canal procedures. The newfound simplicity in the process, coupled with enhanced disinfection, signifies a positive shift in the overall treatment approach.
Irrigation and disinfection
As touched on earlier, the traditional approach to root canal procedures involved rinsing the canal system using a conventional syringe. However, based on extensive studies,5 it is well-established that irrigant delivery using this method may not effectively6 reach the entirety of the root canal system. This limitation prompted the need for improvements in the irrigation process. Sonic and ultrasonic devices were introduced as enhancements to the conventional syringe method. While these devices represented progress, they still fell short7 of achieving optimal distribution of bactericidal irrigating solutions throughout the root canal system. The introduction of laser technology marked a transformative leap in addressing this challenge and improving patient outcomes.
Dental lasers have revolutionized root canal procedures by elevating the activation of irrigants to an unprecedented level. Through the laser’s unique capabilities, including cavitation, shockwaves, and shear forces, it facilitates the dissolution, fragmentation, and thorough debridement of tissues. This innovative approach addresses the common dilemma of leaving tissue remnants behind.
There is a compelling anticipation that the advanced irrigation technique facilitated by the laser will lead to enhanced success rates for our patients. This assertion underscores the potential of laser technology to contribute to the continued improvement of outcomes in root canal procedures.
When approaching root canal cleaning and disinfection with the laser, first we instrument the canals using less tapered files to conserve tooth structure. After instrumentation, we place the dental laser tip loosely at the mid-root in a wet canal, only activating the laser while withdrawing the tip from the canal in a circular motion at a rate of 1 mm per second.
The energy from the Waterlase forms a vapor bubble at the laser tip within the irrigation solution. When the bubble collapses, a pressure wave and additional cavitation bubbles are created, cleaning the canal walls, removing the smear layer, disrupting biofilm, and extending to reach lateral canals into the apical regions. Dentinal tubules are opened by more effective smear layer removal especially when agitating with 17% EDTA solution, facilitating a deeper dentinal cleaning. LAI with YSGG used to activate EDTA was shown8 to leave only <8% of residual debris, while needle irrigation was shown9 to leave 40% of residue. Although some bacteria may remain in the tubules, this will be treated during the disinfection step of the dental laser process.
I like to refer to this deeper cleaning of the dentinal tubules as “deep disinfection.” You can think of the prior steps as the debridement phase of endodontic treatment where vital or necrotic tissue, and smear layer removal generated from instrumentation are removed. Bulk disinfection of the main canal is also established in this phase, but it’s the next step in “deep disinfection,” where the laser really shines due to tip placement in the canal.
Again, I start by placing the laser tip at the mid-root and slowly withdraw the tip once activated at 1 mm/sec and repeat 3 to 4 times per canal. This is done with a final 3% NaOCl solution. To gauge the effectiveness of disinfection, I point to two studies: first when applied inside of the canal, laser-assisted irrigation with NaOCl reaches more than twice10 as deep into the tubules than NaOCl alone. Secondly, the laser tip into the canal with either 2.5% NaOCl or 2% chlorhexidine reduced 4-week-old e. faecalis colonies by more than 99.9%.11 Always take great care not to bind the tip in the canal and stick to the recommended protocols and settings.
In addition to the system that is used in my practice, various other types of lasers have demonstrated efficacy in endodontic procedures. Among them, the Er: YAG (erbium-doped yttrium aluminum garnet) laser and the Nd: YAG (neodymium-doped yttrium aluminum garnet) laser are notable. The Er: YAG laser operates at a wavelength of 2940 nm, effectively removing soft and hard tissues with minimal thermal damage. Its ability to efficiently ablate dentin and enamel makes it suitable for root canal preparation and debridement. Similarly, the Nd: YAG laser, operating at a wavelength of 1064 nm, has shown promise in disinfection and debris removal within the root canal system. These lasers offer alternative options for endodontic treatment, providing clinicians with versatile tools to enhance cleaning, disinfection, and overall treatment outcomes. Integrating these advanced laser technologies into endodontic protocols can further optimize patient care by addressing challenges such as residual debris and microbial presence within the root canal system, ultimately leading to improved success rates and patient satisfaction.
A spectrum of possibilities
The Waterlase iPlus unit uses a versatile Erbium, Chromium: YSGG 2780 nm wavelength, and has a notable distinction in power, reaching up to 10 Watts. This versatile wavelength developed for dentistry specifically, along with its elevated power opens up a multitude of applications, allowing for not only irrigation but also enabling proficiency in soft tissue surgery and hard tissue surgery. This expanded capability establishes its utility in both routine and complex endodontic surgical procedures.
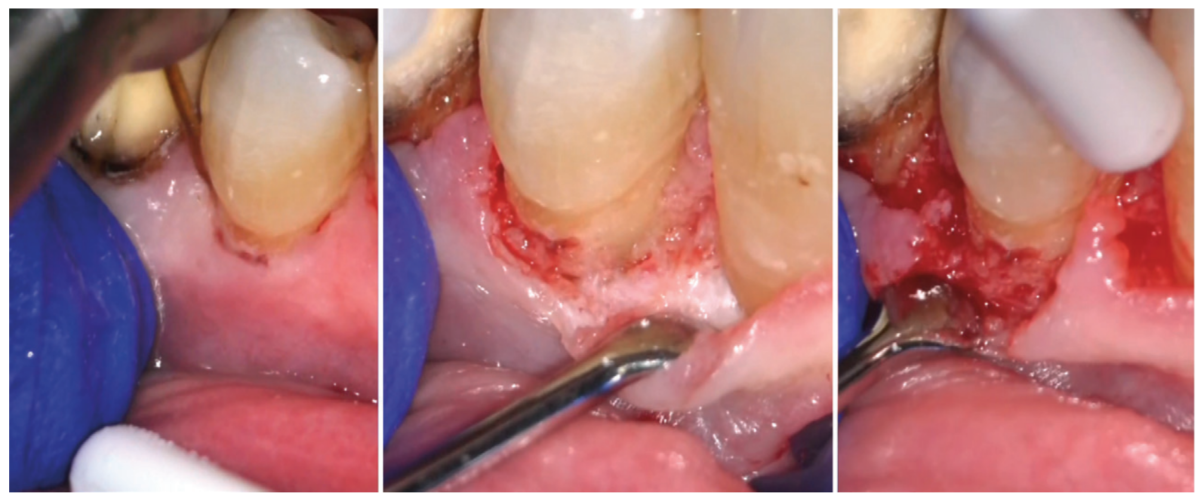
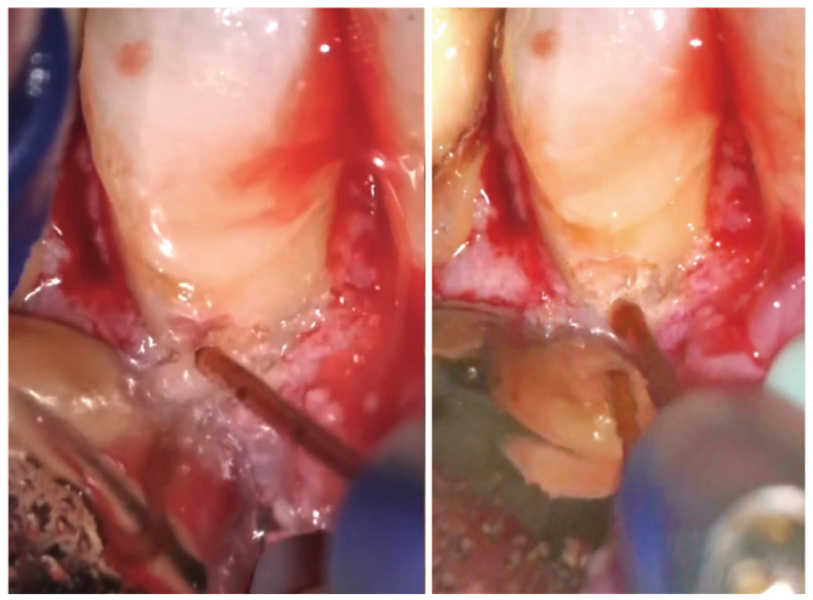
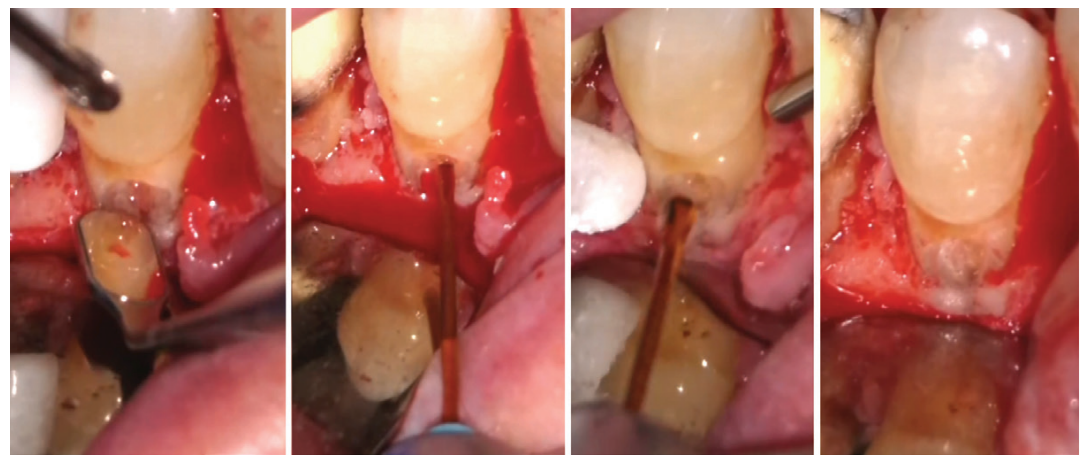
Beyond conventional root canal procedures, we also employ the laser for soft tissue surgeries, such as gingivectomy, gingivoplasty, crown lengthening, and precise incisions of flaps during endodontic surgeries. Additionally, the laser finds its utility in osteotomy, involving the judicious removal of bone and chronic apical granulation tissue during endodontic surgery. One of the benefits of the 2780 nm wavelength is deeper penetration into tissues and just the right amount of laser thermal effect to induce hemostasis while cutting at the same time.
In intricate cases, such as root resection, the laser enables precise cutting of the root tip from infected cases and debridement of the infected bone behind the resected root. Furthermore, when addressing certain resorption defects characterized by external resorptive tissue and persistent bleeding, the laser proves invaluable. It can ablate tissue minimally invasively and ensures remarkable hemostasis, mitigating the challenges commonly encountered during such procedures.
Additionally, laser-assisted vital pulp therapy techniques hold promise for preserving the vitality of dental pulp and promoting natural healing.12 The precision of lasers enables targeted stimulation of the vital pulp with simultaneous precise disinfection and control of hemostasis as inflamed layers of the pulp are removed. This innovative approach marks a paradigm shift from traditional endodontic treatments. Laser applications in carious lesions leading to direct or indirect pulp caps, taking preoperative symptoms into account, could be approached in a whole new way, and in some instances eliminate the need for root canal procedures.
Lasers leading the way
As lasers continue to improve, their role in improving patient outcomes becomes increasingly prominent. From enhanced disinfection and tissue preservation to reduced postoperative discomfort, lasers contribute to a more positive overall patient experience. The future of endodontic practice is intricately tied to the continued refinement and integration of laser technology, promising a landscape where advanced techniques and improved outcomes redefine the standards of care in the field of endodontics.
Providers have an obligation to learn about any technology that will benefit the patients we care for. If it’s reasonable, effective, and affordable, there is no reason not to incorporate it into everyday endodontic treatment and expanded functions. The integration of lasers not only addresses current challenges but also paves the way for a brighter and more patient-centric approach to endodontics, where innovation meets precision for the benefit of both clinicians and those seeking the highest quality dental care.
Dr. David Keinan sheds light on the role of lasers in smear layer removal and biofilm disinfection. Read his article here: https://endopracticeus.com/shedding-light-lasers/
References
- León-López M, Cabanillas-Balsera D, Martín-González J, Montero-Miralles P, Saúco-Márquez JJ, Segura-Egea JJ. Prevalence of root canal treatment worldwide: A systematic review and meta-analysis. Int Endod J. 2022 Nov;55(11):1105-1127.
- American Association of Endodontists. Root Canal Explained. https://www.aae.org/patients/root-canal-treatment/what-is-a-root-canal/root-canal-explained/. Accessed May 2, 2024.
- Fahim SZ, Ghali RM, Hashem AA, Farid MM. The efficacy of 2780 nm Er,Cr;YSGG and 940 nm Diode Laser in root canal disinfection: A randomized clinical trial. Clin Oral Investig. 2024 Feb 26;28(3):175.
- Waterlase iPlus Premier Edition. https://www.biolase.com/products/dental-lasers-all-tissue/waterlase-iplus/. Accessed May 29, 2024.
- Boutsioukis C, Arias-Moliz MT. Present status and future directions – irrigants and irrigation methods. Int Endod J. 2022 May;55 Suppl 3(Suppl 3):588-612.
- Ali A, Bhosale A, Pawar S, Kakti A, Bichpuriya A, Agwan MA. Current Trends in Root Canal Irrigation. 2022 May 8;14(5):e24833.
- Raducka M, Piszko A, Piszko PJ, Jawor N, Dobrzyński M, Grzebieluch W, Mikulewicz M, Skośkiewicz-Malinowska K. Narrative Review on Methods of Activating Irrigation Liquids for Root Canal Treatment. Applied Sciences. 2023; 13(13):7733.
- Kuştarcı A, Er K, Siso SH, Aydın H, Harorlı H, Arslan D, Kirmali O. Efficacy of Laser-Activated Irrigants in Calcium Hydroxide Removal from the Artificial Grooves in Root Canals: An Ex Vivo Study. Photomed Laser Surg. 2016 May;34(5):205-210.
- Meire MA, Havelaerts S, De Moor RJ. Influence of lasing parameters on the cleaning efficacy of laser-activated irrigation with pulsed erbium lasers. Lasers Med Sci. 2016 May;31(4):653-658.
- Wang X, Cheng X, Liu X, Wang Z, Wang J, Guo C, Zhang Y, He W. Bactericidal Effect of Various Laser Irradiation Systems on Enterococcus faecalis Biofilms in Dentinal Tubules: A Confocal Laser Scanning Microscopy Study. Photomed Laser Surg. 2018 Sep;36(9):472-479.
- Aydin S, Taşdemir T, Buruk K, Celik D. Efficacy of Erbium, Chromium-doped Yttrium, Scandium, Gallium and Garnet Laser-activated Irrigation Compared with Passive Ultrasonic Irrigation, Conventional Irrigation, and Photodynamic Therapy against Enterococcus faecalis. J Contemp Dent Prac. January 2020;21(1):11-16.
- Cengiz E, Yilmaz HG. Efficacy of Erbium, Chromium-doped:Yttrium, Scandium, Gallium, and Garnet Laser Irradiation Combined with Resin-based Tricalcium Silicate and Calcium Hydroxide on Direct Pulp Capping: A Randomized Clinical Trial. J Endod. 2016 Mar;42(3):351-355.
Stay Relevant With Endodontic Practice US
Join our email list for CE courses and webinars, articles and more..

