CE Expiration Date: September 13, 2027
CEU (Continuing Education Unit):2 Credit(s)
AGD Code: 070
Educational aims and objectives
This self-instructional course for dentists aims to review management of endodontic cases with periapical lesions using minimal instrumentation.
Expected outcomes
Endodontic Practice US subscribers can answer the CE questions by taking the quiz online to earn 2 hours of CE from reading this article. Correctly answering the questions will demonstrate the reader can:
- Review the keys to successful endodontic treatment.
- Define how the GentleWave System uses multisonic acoustic energy to transmit the irrigation solution to the root canal system.
- Observe two case reports to show management of periapical lesions.
Drs. Karen Potter, Seda Falakaloğlu, and Mustafa Gündoğar explain the multisonic energy technology of the GentleWave System for managing teeth with periapical lesions.
Drs. Karen Potter, Seda Falakaloğlu, and Mustafa Gündoğar describe how multisonic technology can clean and disinfect teeth
Endodontic treatment aims to restore and preserve the health of apical tissues so that patients can achieve a functional and asymptomatic tooth structure. Removal of infected tissue and bacteria appears to increase the success rate of endodontic treatment.1,2 Due to the inadequacies of mechanical debridement alone and complex anatomy, many different irrigation and activation techniques have been used. Adequate irrigation is the key to successful endodontic treatment because it is the only way to reach areas untouched by instrumentation.3-5
The GentleWave® system (GWS) (Sonendo® Inc, California) uses multisonic technology to deliver irrigation solutions from the tip of a procedure instrument into the pulp chamber and canal system. These solutions are degassed to prevent energy loss.6 GWS consists of a console and three different handpieces (Anterior/Premolar, Molar, and Cleanflow PI). Integrated flow diverters in these handpieces convert the degassed solution flow into a spatter, which interacts with the stationary liquid. This movement in the negative pressure environment allows the continuous formation and bursting of microbubbles within the root canal system to create hydrodynamic cavitation. As a result of this mechanical movement, multisonic acoustic energy is generated that transmits the irrigation solution to the root canal system.7-9
This article deals with managing two endodontic cases with periapical lesions using GWS and minimal instrumentation. The aim is to discuss the clinical outcome of GWS and offer clinicians treatment guidance.
Case reports
Case 1
A 43-year-old female patient with a noncontributory medical history was referred with a chief complaint of a bad toothache that was very painful to touch. The patient reported a history of trauma and had been told that tooth No. 8 had been dead for years. There was a history of internal bleaching 4 years prior with some success, but the shade had regressed. Clinical examination of the right first maxillary central revealed fluctuant swelling of the labial gingiva. Radiographic examination revealed a lingual composite restoration and a blunted root tip with calcific metamorphosis. Also, a periapical lesion was associated with the root canal (Figure 1A). The patient’s history of symptoms and the clinical examination indicated a pulpal diagnosis of pulp necrosis and an acute apical abscess. After a review of options with the patient, root canal treatment with internal bleaching was recommended to retain the tooth, and the patient consented to care.
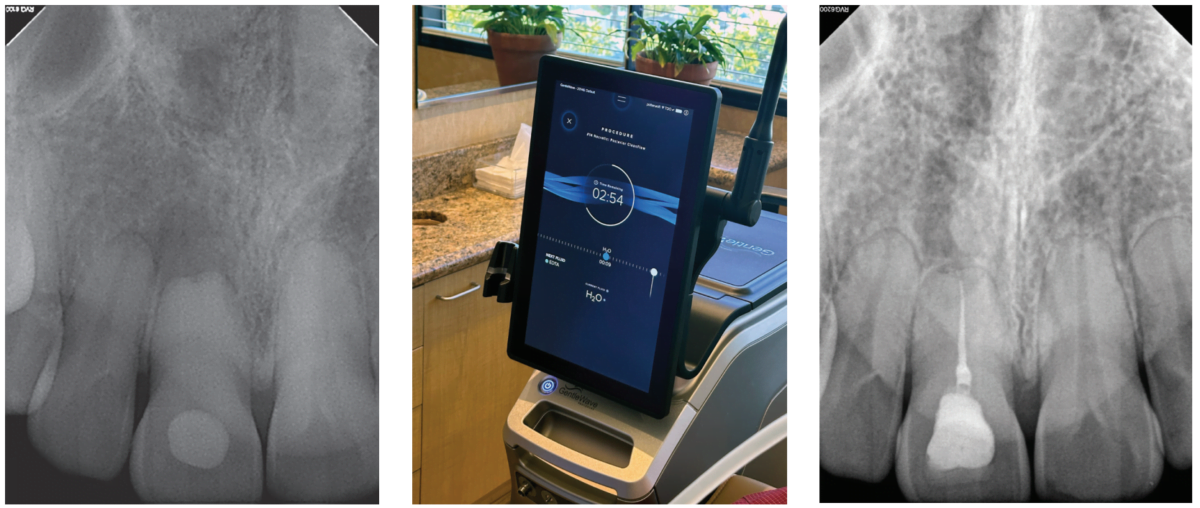
A standard anesthesia protocol (lidocaine with 1:100.000 epinephrine and articaine with 1:200.000 epinephrine through buccal and palatal infiltration) was followed, and the tooth was isolated with a rubber dam. A dental operating microscope was utilized for creating a minimally invasive, straight-line endodontic access opening. After patency and working length were established, mechanical instrumentation was prepared with No. 20 variable taper SlimShaper® file (Avalon Biomed, Houston, Texas). Following minimal preparation, debridement and disinfection were completed utilizing the GWS, where sodium hypochlorite (NaOCI) + distilled water + ethylenediaminetetraacetic acid (EDTA) + distilled water were delivered using Multisonic UItracleaning technology (Figure 1B). After the cleaning process, the root canal was dried using sterile paper points. A single cone technique employing gutta percha and bioceramic sealer (EndoSequence® BC Sealer HiFlow; Brasseler USA, Savannah, Georgia) was utilized during obturation. A coronal seal was placed, and the access cavity was sealed with temporary filling material. The patient was advised to return to the referring general dentist for internal bleaching.
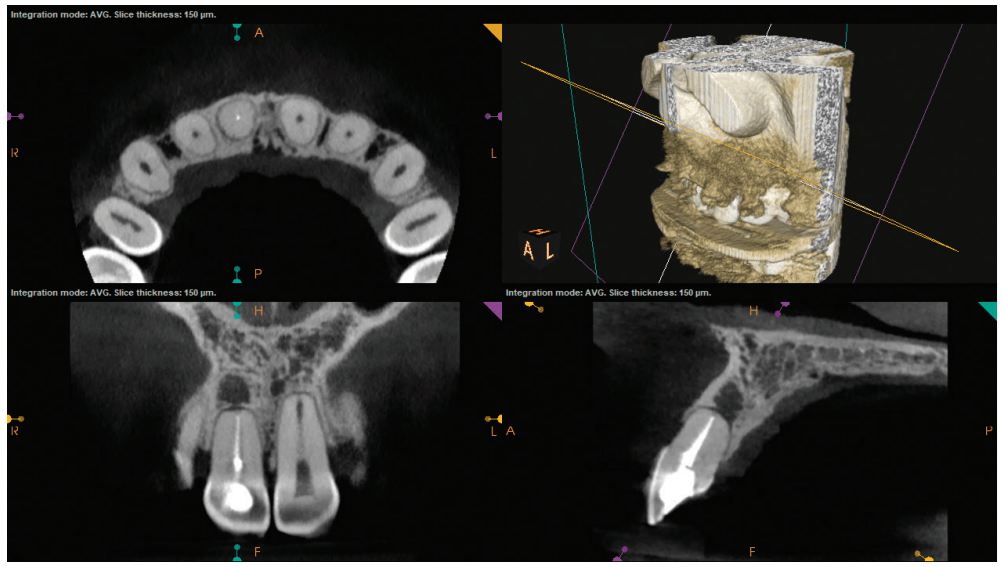
A postoperative radiograph is presented in Figure 1C. At the 2-year recall, the patient was asymptomatic. Upon clinical and radiographic examination, there was no painful response to percussion or palpation, no presence of mobility, fractures, soft tissue lesions, or root resorption radiographically. After 2 years of GWS, cone beam computed tomography (CBCT) images show intact lamina dura and growth of trabecular bone in Figure 1D.
Case 2
A 75-year-old female patient with a noncontributory medical history was referred with a chief complaint of dull pain in the lower right quadrant for 1 month, worsened by pressing on the gum. The patient reported a history of crown preparations of teeth Nos. 30 and 31, 1 week prior. Gingival swelling for several days had partially subsided since starting antibiotic therapy. Clinical examination of the right first maxillary molar (No. 30) revealed negative sensitivity to percussion and a mild pain response to palpation. There was a vestibular swelling over the mesial root of tooth No. 30. Vitality testing elicited a negative response. Radiographic examination revealed a large periapical lesion on the mesial root of tooth No. 30 (Figure 2A). The patient’s history of symptoms and the clinical examination indicated a diagnosis of pulp necrosis and an acute apical abscess. After a review of options with the patient, endodontic therapy was recommended to retain the tooth.
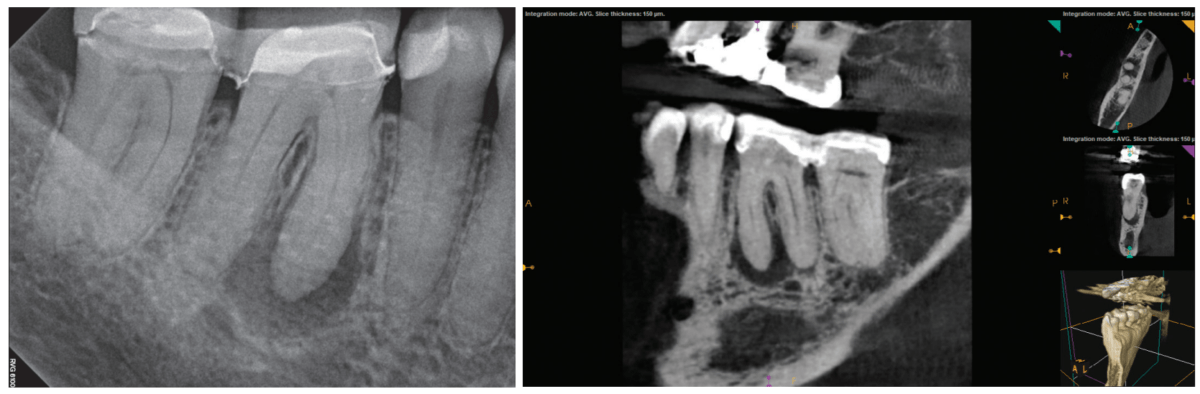
After standard local anesthesia and isolation protocols, the temporary crown was removed, and the tooth was accessed under the dental operating microscope. Upon entry to the pulp chamber, necrotic tissue and purulence was noted from the mesial canals. After patency and working length were established, mechanical instrumentation was prepared with at No. 20 variable taper SlimShaper file. Following minimal preparation, debridement and disinfection were completed utilizing the GWS, where sodium hypochlorite (NaOCI) + distilled water + ethylenediaminetetraacetic acid (EDTA) + distilled water were delivered using Multisonic UItracleaning technology. After the cleaning process, root canals were dried using sterile paper points. A single cone technique employing gutta percha and bioceramic sealer were utilized during obturation (Figure 2B). A coronal seal was placed, and the temporary crown was re-cemented with TempBond™ (Kerr).
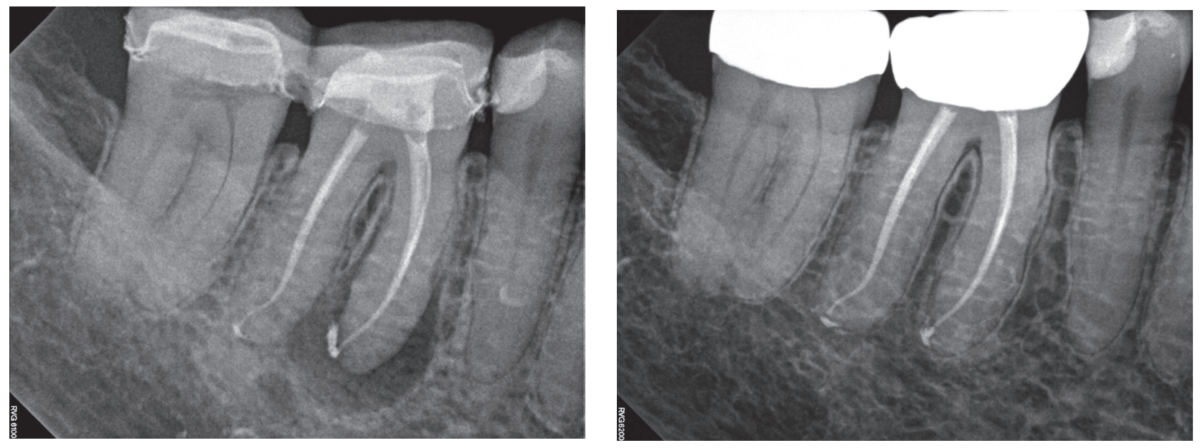
Upon completion of endodontic therapy with the GWS, at the 6-month recall, the tooth was asymptomatic (Figure 2C). The CBCT was taken, and images showed complete healing of the apical bone (Figure 2D).

Discussion
The primary goal of endodontic treatment of pulpal infected teeth and periapical lesions is to eliminate the infection and prevent microorganisms from infecting or re-infecting the root and surrounding tissues.10 In this article, we evaluated the efficacy of GWS on the healing of periapical lesions. The patients with periapical lesions in their teeth healed after endodontic therapy with the GentleWave Procedure which allows better irrigation and canal anatomy contact with the irrigants then standard irrigation techniques.
The concept of minimally invasive preparation to save root dentin by instrumenting smaller file sizes in root canals has been discussed for years. Preserving the dentin structure in its natural form is one of the main factors improving the prognosis after endodontic treatment.11 Notwithstanding, the GWS is a minimally invasive alternative treatment for root canal therapy. GWS reduces the need to shape the roots using extensive instrumentation, thus preserving dentin for minimal invasive endodontic technique. In the literature, in-vitro GWS studies have shown that a statistically significant clean root canal system was observed even when molars were shaped with No. 15/.04.7-9 This remarkable effect results from the combined washing effect, multisonic energy, and the dissolving action of NaOCl and EDTA irrigating solutions. Cavitation releases energy from imploding, microscopic vacuum, and gas bubbles, allowing the freed force to dissolve and break down pulpal tissue.12 In our cases, the root canals were prepared with a No. 20 variable taper SlimShaper file. This preparation size adheres to GWS’s minimally invasive root canal preparation philosophy, which achieved successful results.
Sigurdsson, et al., reported that treatment of sizable periapical lesions with the GWS resulted in a success rate of 97.7% at 12-month re-evaluation.13 Essentially, unsuccessful root canal treatments are often the result of microorganisms remaining in the canals after treatment. The lack of success is probably due to the limitations of traditional chemomechanical instrumentation and the difficulties in accessing the morphological complexities in the root canals.10 The success of GWS in removing microorganisms from anatomical complexities was able to facilitate both the healing of the periapical lesion and the regrowth of the alveolar bone.14,15 Healing depends on the disinfection process’s effectiveness and the host’s response to the debris or biofilm remaining in the root canals, so lesion healing is a dynamic process.16 GWS has been shown to remove the smear layer and biofilm effectively.17,18 In addition, Haapasalo, et al., reported that GWS greatly improved the effectiveness of tissue dissolution compared to other irrigation methods.8 The rapid organic tissue ability and effective removal process could contribute to the healed periapical lesions in our cases. Noticeably, one of the cases presented healed after 6 months. This rapid healing has been consistent with a prospective clinical study using GWS.19
In these case reports, both teeth were cleaned and disinfected during the GWS with no evidence of reinfection, clinical signs, or symptoms present at the 6 month and 2 year recalls. These case reports demonstrate the ability of the GWS to clean and disinfect teeth with apical periodontitis and minimally instrumented canals.
Conclusion
The cases presented in this paper highlight the use of multisonic energy technology as the GentleWave System, in managing teeth with periapical lesions. Although more extensive clinical studies need to be utilized, these clinical cases show that the GentleWave System improves the success of endodontic treatment results with minimal instrumentation.
Dentists are using GentleWave on pediatric patients too. Read how Dr. Lauren Tink provided endodontic treatment to an anxious young patient here: https://endopracticeus.com/single-visit-regenerative-endodontics-using-the-gentlewave-procedure-a-pediatric-case-report/.
References
- Vera J, Siqueira JF Jr, Ricucci D, Loghin S, Fernández N, Flores B, Cruz AG. One- versus two-visit endodontic treatment of teeth with apical periodontitis: a histobacteriologic study. J Endod. 2012 Aug;38(8):1040-1052.
- Sjögren U, Figdor D, Persson S, Sundqvist G. Influence of infection at the time of root filling on the outcome of endodontic treatment of teeth with apical periodontitis. Int Endod J. 1997 Sep;30(5):297-306.
- Burleson A, Nusstein J, Reader A, Beck M. The in vivo evaluation of hand/rotary/ultrasound instrumentation in necrotic, human mandibular molars. J Endod. 2007 Jul;33(7): 782-787.
- Susin L, Liu Y, Yoon JC, Parente JM, Loushine RJ, Ricucci D, Bryan T, Weller RN, Pashley DH, Tay FR. Canal and isthmus debridement efficacies of two irrigant agitation techniques in a closed system. Int Endod J. 2010 Dec;43(12):1077-1090.
- Gu LS, Kim JR, Ling J, Choi KK, Pashley DH, Tay FR. Review of contemporary irrigant agitation techniques and devices. J Endod. 2009 Jun;35(6):791-804.
- Shon WJ. Introducing the GentleWave System. Restor Dent Endod. 2016 Aug;41(3):235. Epub 2016 Jul 26.
- Molina B, Glickman G, Vandrangi P, Khakpour M. Evaluation of Root Canal Debridement of Human Molars Using the GentleWave System. J Endod. 2015 Oct;41(10): 1701-1705.
- Haapasalo M, Wang Z, Shen Y, Curtis A, Patel P, Khakpour M. Tissue dissolution by a novel multisonic ultracleaning system and sodium hypochlorite. J Endod. 2014 Aug;40(8):1178-1181.
- Charara K, Friedman S, Sherman A, Kishen A, Malkhassian G, Khakpour M, Basrani B. Assessment of Apical Extrusion during Root Canal Irrigation with the Novel GentleWave System in a Simulated Apical Environment. J Endod. 2016 Jan;42(1):135-139.
- Narayanan LL, Vaishnavi C. Endodontic microbiology. J Conserv Dent. 2010 Oct;13(4): 233-239.
- Murdoch-Kinch CA, McLean ME. Minimally invasive dentistry. J Am Dent Assoc. 2003 Jan;134(1):87-95.
- Chen B, Szabo D, Shen Y, Zhang D, Li X, Ma J, Haapasalo M. Removal of calcifications from distal canals of mandibular molars by a non-instrumentational cleaning system: A micro-CT study. Aust Endod J. 2020 Apr;46(1):11-16.
- Sigurdsson A, Garland RW, Le KT, Rassoulian SA. Healing of Periapical Lesions after Endodontic Treatment with the GentleWave Procedure: A Prospective Multicenter Clinical Study. J Endod. 2018 Mar;44(3):510-517.
- Patel S, Wilson R, Dawood A, Foschi F, Mannocci F. The detection of periapical pathosis using digital periapical radiography and cone beam computed tomography – part 2: a 1-year post-treatment follow-up. Int Endod J. 2012 Aug;45(8):711-723.
- Vandrangi P. Evaluating Penetration Depth of Treatment Fluids into Dentinal Tubules Using the GentleWave System. 2016;6(3).
- Zhang MM, Liang YH, Gao XJ, Jiang L, van der Sluis L, Wu MK. Management of Apical Periodontitis: Healing of Post-treatment Periapical Lesions Present 1 Year after Endodontic Treatment. J Endod. 2015 Jul;41(7):1020-1025.
- Choi HW, Park SY, Kang MK, Shon WJ. Comparative Analysis of Biofilm Removal Efficacy by Multisonic Ultracleaning System and Passive Ultrasonic Activation. Materials (Basel). 2019 Oct 25;12(21):3492.
- Zhang D, Shen Y, de la Fuente-Núñez C, Haapasalo M. In vitro evaluation by quantitative real-time PCR and culturing of the effectiveness of disinfection of multispecies biofilms in root canals by two irrigation systems. Clin Oral Investig. 2019 Feb;23(2):913-920.
- Sigurdsson A, Le KT, Woo SM, Rassoulian SA, McLachlan K, Abbassi F, Garland RW. Six-month healing success rates after endodontic treatment using the novel GentleWave™ System: The pure prospective multi-center clinical study. J Clin Exp Dent. 2016 Jul 1;8(3):e290-298.
Stay Relevant With Endodontic Practice US
Join our email list for CE courses and webinars, articles and more..

 Karen Potter, DDS, has provided endodontic care in San Clemente, California for almost 15 years. She graduated from the University of Southern California Magna Cum Laude with degrees in Spanish and Natural Sciences. She then went to dental school at the UCLA School of Dentistry, and after that she attended her Endodontic residency program at the University of Iowa. Her research project in residency regarding the placement of dental implants by endodontists has been published in the JOE and cited frequently.
Karen Potter, DDS, has provided endodontic care in San Clemente, California for almost 15 years. She graduated from the University of Southern California Magna Cum Laude with degrees in Spanish and Natural Sciences. She then went to dental school at the UCLA School of Dentistry, and after that she attended her Endodontic residency program at the University of Iowa. Her research project in residency regarding the placement of dental implants by endodontists has been published in the JOE and cited frequently. Seda Falakaloğlu, DDS, graduated from Ege University, Faculty of Dentistry in Turkey, receiving her dental degree in 2011. She worked as a research assistant in the Department of Endodontics at Dicle University Faculty of Dentistry and became qualified to become an endodontist in 2017 and has worked as an associate professor in the Department of Endodontics, Faculty of Dentistry at Istanbul Health and Technology University, Istanbul, Turkey, since 2023.
Seda Falakaloğlu, DDS, graduated from Ege University, Faculty of Dentistry in Turkey, receiving her dental degree in 2011. She worked as a research assistant in the Department of Endodontics at Dicle University Faculty of Dentistry and became qualified to become an endodontist in 2017 and has worked as an associate professor in the Department of Endodontics, Faculty of Dentistry at Istanbul Health and Technology University, Istanbul, Turkey, since 2023. Dr. Mustafa Gündoğar, DDS, graduated from Marmara University, Faculty of Dentistry in Turkey with his dental degree in 2005. He attended the Endodontics Program of Graduate Study offered by Institute of Health Sciences at Marmara University and graduated with a PhD degree in Endodontics in 2011. He is currently working in the Department of Endodontics, Faculty of Dentistry at Medipol University, Istanbul, Turkey as an associate professor. Dr Gündoğar has been working at the Regenerative and Restorative Medicine Research Center (REMER) since 2020. Dr. Gündoğar is a social media influencer with more than 55K people on Instagram. He is the founder of ENDOTALKS Library, the first patented endodontic education platform on social media.
Dr. Mustafa Gündoğar, DDS, graduated from Marmara University, Faculty of Dentistry in Turkey with his dental degree in 2005. He attended the Endodontics Program of Graduate Study offered by Institute of Health Sciences at Marmara University and graduated with a PhD degree in Endodontics in 2011. He is currently working in the Department of Endodontics, Faculty of Dentistry at Medipol University, Istanbul, Turkey as an associate professor. Dr Gündoğar has been working at the Regenerative and Restorative Medicine Research Center (REMER) since 2020. Dr. Gündoğar is a social media influencer with more than 55K people on Instagram. He is the founder of ENDOTALKS Library, the first patented endodontic education platform on social media.