Drs. Warley Luciano Fonseca Tavares and Gustavo de Cristofaro Almeida explore the advantages of bioceramic cements for endodontic retreatment.
Drs. Warley Luciano Fonseca Tavares and Gustavo de Cristofaro Almeida explore the use of bioceramic cements in nonsurgical endodontic retreatment
Abstract
The success of endodontic treatment is closely related to the complete debridement and disinfection of the root canal system (RCS) associated with its three-dimensional seal. Bioceramics, which are cements composed of silicates (particles similar to those found in the MTA) have characteristics that enable their use in the filling of the RCS. The aim of this article is to present two cases involving the use of a bioceramic root canal sealer. It is clinically notable that bioceramic cements have an effective action in inducing repair of periapical tissues. In view of the observed findings, we conclude that the use of bioceramic cements in cases of nonsurgical endodontic retreatment is well indicated.
Introduction
The success of endodontic treatment is closely related to the complete debridement and disinfection of the root canal system (RCS) associated with its three-dimensional seal.1,2 Therefore, it is essential that the filling material used is biocompatible and induces the repair process in the periapical tissues. Over the years, several types of cements have been used to fill the RCS, and those based on zinc oxide and eugenol or resin were the most used.1,2 Although very widespread, these cements have limitations regarding the induction of tissue repair.1
The filling materials, although contained within the RCS, interact directly with the surrounding tissues through the apical foramen and accessory communications.3,4 Thus, its properties and compositions can influence the immunoinflammatory reactions that occur in the periradicular region after its use.3
Recently, a new class of endodontic cements — the bioceramic cements — has emerged on the market. These materials are an evolution of mineral trioxide aggregate (MTA), which has been used frequently, presenting satisfactory clinical and laboratory results.5,6 MTA is a biocompatible, bioactive, and hydrophilic material5-9 indicated mainly for the treatment of internal and external resorption, sealing of perforations, apexification, and retro-obturations.
However, due to its sandy consistency and lack of flow, MTA is not suitable for conventional RCS filling. Bioceramics, which are cements composed of silicates (particles similar to those found in the MTA) have been developed to reverse these limitations, having characteristics that enable their use in the filling of the RCS.10
The aim of this article is to present two cases involving the use of a bioceramic root canal sealer.
Case 1
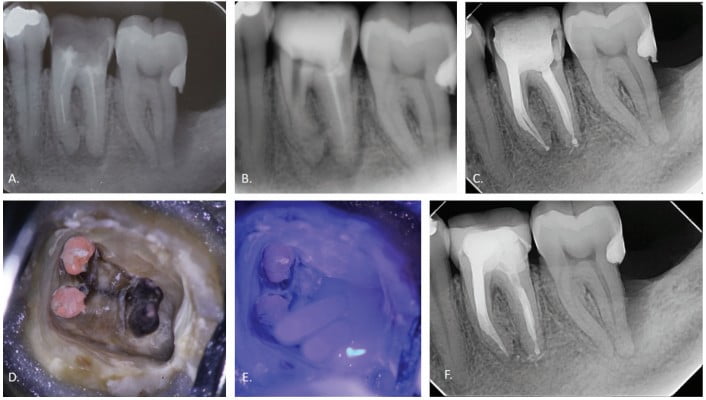
A 54-year-old man was referred for the endodontic retreatment of his mandibular left first molar. The patient presented with swelling and pain. At the radiographic evaluation, the presence of a fractured instrument in the mesial root and periapical lesion were observed. At the first appointment, the instrument was retrieved under the use of the operating microscope and the auxilium of ultrasonic tips. After complete removal of gutta percha, patency was reached, and the canals were instrumented with a series of rotary NiTi files (Bassi Logic™ shaping and glidepath files, Bassi Endo) up to size 30/.05 and irrigated with a 2.5% sodium hypochlorite (NaOCl) solution. After a 17% ethylenediaminetetraacetic acid (EDTA) solution was applied for 60 seconds, the canals were filled with calcium hydroxide, and it was left in place for 15 days until the next appointment.
During the second session, the root canal dressing was removed, and the canals were irrigated again using the following protocol. First, 3 mL of 2.5% NaOCl solution was introduced and agitated for 60 seconds with a rotary plastic activating file (Bassi Clean™, Bassi Endo) at 20,000 rpm. Next, 1 mL of 17% EDTA was placed and agitated for 60 seconds at 20,000 rpm. And last, another 3 mL of 2.5% NaOCl solution was placed and agitated for 60 seconds at 20,000 rpm, followed by a final irrigation with 1 mL of saline solution. After the canals were properly dried with absorbent paper cones, the root canal obturation was performed with a bioceramic root canal sealer (BIO-C® Sealer, Angelus) and gutta percha using the lateral condensation technique. The tooth received a fiberglass post in the distal canal and was restored with composite resin. An onlay ceramic restoration was performed. At the 6-month follow-up visit, the patient was asymptomatic, and complete healing of the periapical tissues was observed (Figure 1).
Case 2
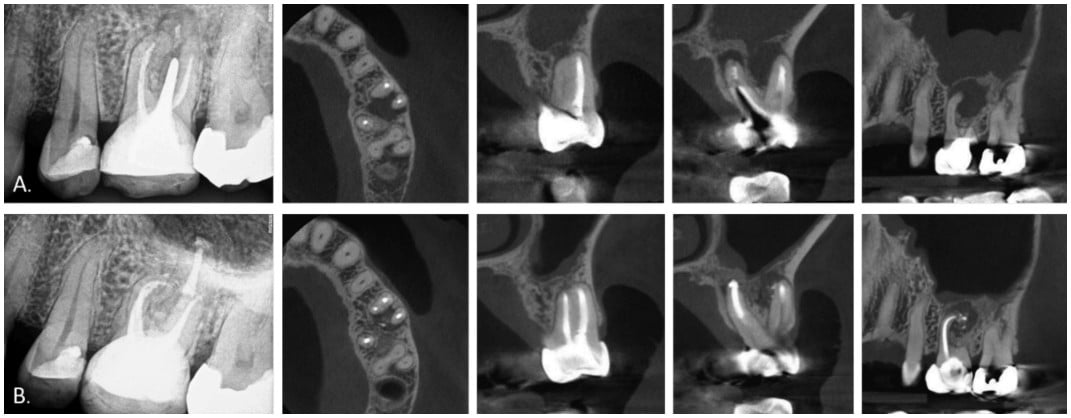
A 59-year-old woman presented with diffuse pain in the left upper jaw and symptoms compatible with sinusitis. At the radiographic and cone beam computed tomography (CBCT) evaluation, the presence of unsatisfactory endodontic treatment of maxillary first molar and associated periapical lesion were observed. The nonsurgical retreatment was performed with a series of rotary NiTi files (Bassi Logic™ shaping and glidepath files, Bassi Endo) up to size 30/.05 in buccal canals and 40/.05 in the palatal canal. During the procedure, the root canal system was irrigated with 5.25% NaOCl solution. After the application of 17% EDTA solution for 90 seconds, the canals were dried with paper points and filled with calcium hydroxide, which was left in place for 15 days until the next appointment.
At the second session, the root canal dressing was removed, and the canals were irrigated again using the same protocol described for Case 1. After the canals were properly dried with absorbent paper cones, the root canal obturation was performed with a bioceramic root canal sealer (BIO-C® Sealer, Angelus) and gutta percha using the single cone technique. The tooth received a fiberglass post in the palatal canal and was restored with composite resin. A ceramic full-crown was performed. At the 7-month follow-up visit, the patient was asymptomatic, and complete healing of the periapical tissues was observed (Figure 2).
Discussion
The lack of adequate mechanical chemical debridement and sealing of the RCS enabled the establishment and maintenance of an infectious process, which is the cause of the previous failure of the cases presented. It has been shown that infection in cases of lesions refractory to endodontic treatment is more complex than previously imagined.11 For us to be able to reverse the infectious condition, it is essential that all root canals are accessed and instrumented in all its extension. In cases of retreatment with periapical lesion, this task can bring great difficulties for the clinician.
The filling material plays an important role in retreatment cases due to the presence of irregularities in the walls caused by wear during the removal of the filling material or resorption. Interestingly, within a short period of time, we observed the repair of periapical tissues in the cases presented. This result corroborates to the findings of a recent article that presented cases of endodontic treatment on teeth with extensive lesions and resorption.12 It is clinically notable that bioceramic cements have an effective action in inducing repair of periapical tissues, in accordance to the findings of in vitro studies with such materials.13,14
In view of the observed findings, we conclude that the use of bioceramic cements in cases of nonsurgical endodontic retreatment is well indicated.
After reading about bioceramic cements, read Dr. Allen Ali Nasseh’s article on bioceramic liner material here: https://endopracticeus.com/case-studies/bioceramic-liner-material-bridging-the-gap-between-bioceramics-and-restorative-material/.
- de Oliveira Mendes ST, Sobrinho AP, de Carvalho AT, de Souza Côrtes MI, Vieira LQ. In vitro evaluation of the cytotoxicity of two root canal sealers on macrophage activity. J Endod. 2003;29(2):95-99.
- Murray PE, Garcia-Godoy F, Hargreaves KM. Regenerative endodontics: a review of current status and a call for action. J Endod. 2007;33(4):377-390.
- Bernáth M, Szabó J. Tissue reaction initiated by different sealers. Int Endod J. 2003;36(4):256-261.
- Chen I, Salhab I, Setzer FC, Kim S, Nah HD. A new calcium silicate-based bioceramic material promotes human osteo- and odontogenic stem cell proliferation and survival via the extracellular signal-regulated kinase signaling pathway. J Endod. 2016;42(3):480-486.
- Rezende TMB, Vargas DL, Cardoso FP, Sobrinho AP, Vieira LQ. Effect of mineral trioxide aggregate on cytokine production by peritoneal macrophages. Int Endod J. 2005;38(12):896-903.
- Rezende TMB, Vieira LQ, Cardoso FP, et al. The effect of mineral trioxide aggregate on phagocytic activity and production of reactive oxygen, nitrogen species and arginase activity by M1 and M2 macrophages. Int Endod J. 2007;40(8):603-611.
- Koch KA, Brave DG. Bioceramics, part I: the clinician’s viewpoint. Dent Today. 2012;31(1):130-135.
- Liu S, Wang S, Dong Y. Evaluation of a bioceramic as a pulp capping agent in vitro and in vivo. J Endod. 2015;41(5):652-657.
- Braga JM, Oliveira RR, Martins RC, Ribeiro Sobrinho AP. The effects of a mineral trioxide aggregate-based sealer on the production of reactive oxygen species, nitrogen species and cytokines by two macrophage subtypes. Int Endod J. 2014;47(10):909-919.
- Borges RP, Sousa-Neto MD, Versiani MA, et al. Changes in the surface of four calcium silicate-containing endodontic materials and an epoxy resin-based sealer after a solubility test. Int Endod J. 2012;45(5):419-428.
- Henriques LC, de Brito LC, Tavares WL, et al. Microbial Ecosystem Analysis in Root Canal Infections Refractory to Endodontic Treatment. J Endod. 2016;42(18):1239-1245.
- Tavares WL. Endodontic Obturation Using a Bioceramic Sealer. Inside Dentistry. 2020;16(4).
- Candeiro GTM, Moura-Netto C, D’Almeida-Couto RS, et al. Cytotoxicity, genotoxicity and antibacterial effectiveness of a bioceramic endodontic sealer. Int Endod J. 2016;49(9):858-864.
- Zamparini F, Siboni F, Prati C, Taddei P, Gandolfi MG. Properties of calcium silicate-monobasic calcium phosphate materials for endodontics containing tantalum pentoxide and zirconium oxide. Clin Oral Investig. 2019;23(1):445-457.
Stay Relevant With Endodontic Practice US
Join our email list for CE courses and webinars, articles and more..

