Drs. Tiago André Fontoura de Melo and Daniel Galafassi, along with Bruna Machado dos Passos, Sheila Machado dos Passos Zini, Priscila Souza de Souza, and Cláudia Wagner, analyze the effects of calcium hydroxide as intracanal medication and the type of cement used on the adhesion of fiberglass posts with RelyX™ U200
Abstract
This article analyzes if calcium hydrox-ide as intracanal medication and the type of cement used in endodontic treatment influence adhesion of fiberglass posts with RelyX™ U200. Forty bovine teeth were endodontically prepared and then randomly divided into four groups:
G1: Intracanal medication and endo-dontic filling with AH Plus®
G2: Endodontic filling with AH Plus® and without intracanal medication
G3: Intracanal medication and endo-dontic filling with Endofill®
G4: Endodontic filling with Endofill® and without intracanal medication.
The fillings were then removed to receive the fiberglass post, cemented with RelyX U200, and stored for 48 hours in an oven. The samples were sectioned at 1 mm according to the thirds of the roots and subjected to the push-out test. The data obtained was treated by two-way ANOVA. The significance level was 5%. There were no statistical differences between the four groups tested.
Conclusions
The use of medication intracanal calcium hydroxide-based as well as the type of endodontic sealer tested (AH Plus or Endofill) did not interfere with the strength of adhesion of fiberglass posts cemented in the root canal with RelyX U200.
Introduction
Endodontically treated teeth often have insufficient amount of tooth structure to promote a good retention of restorative material. The use of prefabricated intrarradicular posts such as fiberglass posts presents physical chemical properties very similar to the dental structure (Monticelli, et al., 2006), which provides a homogeneous restoration self-contained among the intrarradicular portion and the coronary portion (Souza-Júnior, et al., 2010).
Despite the good bonding response between the fiberglass posts and the tooth structure with the use of resin cements, gaps in the adhesive layer are still reported (Ferrari and Mannocci, 2000). In the literature, one of the variables that can influence this adhesion is the type of the intracanal medication (ICM) employed in endodontic treatment (Paul and Schärer, 1997) as well as the endodontic sealer (Cohen, et al., 2002).
Calcium hydroxide intracanal medications are one of the most widely used by professionals in endodontics. The possible permanence of calcium hydroxide on dentin walls may interfere negatively in the adhesion of the cement (Cohen, et al., 2002).
The use of endodontic sealers is based on the belief that zinc oxide and eugenol can impair the adhesive cementation (Watanabe, et al., 1997). This may be related to the fact that endodontic sealer residues remain on the surface or even to its own constitution. The presence of eugenol is believed to inhibit the polymerization of composite materials, affecting its mechanical properties and adhesive-bonding ability (Fonseca, et al., 2005).
Thus, the characteristics between the materials and the protocols used in the endodontic treatment and the cementation of prefabricated posts are important aspects to be considered to obtain the success on the tooth rehabilitation. The present study proposes to analyze with the mechanical push-out test if calcium hydroxide as an intracanal medication and the type of the endodontic sealer used in root canal treatments influences the adhesion of fiberglass posts.
Methods
Selection and preparation of samples
Forty inferior bovine incisors were selected according to the standardization of the initial apical diameter of the root canal, equivalent to an endodontic instrument type-K No. 40 (Dentsply/Maillefer Instruments S.A., Ballaigues, Switzerland).
After being cleaned, the crowns of the teeth were sectioned at the cementoenamel junction (CEJ) with the aid of a carburundum disc in low rotation. The actual length of root remainder was standardized at 17 mm, and the working length (WL) was 1 mm short of this measurement (WL = 16 mm).
Division of experimental groups
Samples were randomly divided into four experimental groups (Table 1), using the simple random sample technique using the Excel program (Microsoft Excel, Microsoft, USA).
Endodontic preparation of the samples
All samples were prepared manually with first- and second-series K-type stainless steel endodontic instruments (Dentsply Maillefer Instruments S.A., Ballaigues, Switzerland; Tulsa, Oklahoma, USA).
The mechanical chemical preparation was performed using the instrument type K No. 30, continuing until No. 60 (all calibrated in WL). Afterward, the programmed progressive retreat was performed with two more instruments (Nos. 70 and 80), with a 1 mm and 2 mm retreat of the WL, respectively. During the step of staging the preparation, care was taken to recapitulate the WL with instrument No. 60.
At each instrument change, the canals were irrigated with a plastic syringe (BD Solumed, São Paulo, São Paulo, Brazil) and NaviTip 25 mm 30ga needles (Ultradent, Indaiatuba, São Paulo, Brazil; South Jordan, Utah, USA), with 5% sodium hypochlorite (Iodontec Indústria e Comércio de Produtos Odontológicos Ltda., Porto Alegre, Rio Grande do Sul, Brazil) in a standard quantity of 2 mL.
After the preparation, the final disinfection was made with 17% EDTA (Biodinamica, Ibiporã, Paraná, Brazil) for 3 minutes and under agitation of instrument No. 60. The canals were then dried with sterile absorbent paper tips No. 60 (Dentsply/Maillefer Instruments S.A., Ballaigues, Switzerland).
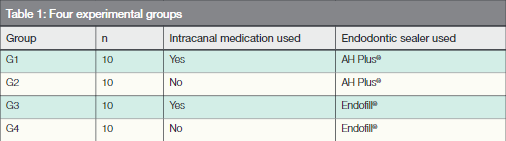

Figure 1: Images of the execution of the push-out test — A (1 mm test body), B (test body positioned on the universal test machine), and C (test specimen with the extruded post after the mechanical test)
Intracanal medication protocol
In the samples of groups G1 and G3, the intracanal medication protocol described here, before the endodontic obturation stage, was performed.
Calcium hydroxide PA (SS White, Rio de Janeiro, Rio de Janeiro, Brazil; Lakewood, New Jersey, USA) associated with saline solution (Cremer S.A., Blumenau, Santa Catarina, Brazil) was used as intracanal medication. The two substances were manipulated under a glass plate and with the aid of a cement spatula No. 24 until obtaining a homogeneous and consistent paste. The pulp was taken from (into) the root canal with the aid of a Lentulo spiral filler No. 45 (KG Sorensen Indústria e Comércio Ltda., Barueri, São Paulo, Brazil), calibrated 2 mm short of WL (14 mm).
After placement of the intracanal medication, the samples were temporarily restored with 2 mm of Cavitec™ (Kerr Dental, Orange, California, USA) and stored in a bottle containing distilled water in an oven at 37°C for 7 days.
No intracanal medication was administered in the G2 and G4 groups. The canals were immediately filled after completion of the mechanical chemical preparation.
Endodontic obturation protocol
Before endodontic obturation for the samples of groups G1 and G3, the restorations were removed with the aid of a diamond bur No. 1012 (KG Sorensen Indústria e Comércio Ltda., Barueri, São Paulo, Brazil), and ICM was removed with the use of instrument No. 60 and 2.5% sodium hypochlorite irrigation. After the removal of the intracanal medication and final disinfecting procedure, 17% EDTA was performed again, followed by drying the canals with absorbent paper tips prior to filling.
The protocol of endodontic obturation executed in all of the samples followed the one recommended by the Tagger Hybrid Technique. As endodontic sealer, zinc oxide and eugenol — Endofill® (Dentsply Maillefer Instruments SA, Ballaigues, Switzerland; Tulsa, Oklahoma, USA) or epoxy resin-based material — AH Plus® (Dentsply/Maillefer Instruments SA, Ballaigues, Switzerland; Tulsa, Oklahoma, USA), according to each experimental group, were provided and spatulated according to the manufacturer’s recommendations, and then the main gutta-percha points No. 60 (Dentsply Maillefer Instruments S.A., Ballaigues, Switzerland; Tulsa, Oklahoma, USA) were wrapped in sealer and introduced into the WL. After insertion of the fifth accessory point (Dentsply Maillefer Instruments SA, Ballaigues, Switzerland; Tulsa, Oklahoma, USA) with the aid of the bidigital spacer B (Dentsply/Maillefer Instruments SA, Ballaigues, Switzerland; Tulsa, Oklahoma, USA) during lateral condensation to obturate the middle and cervical thirds of the canals, gutta percha were plasticized by McSpadden® compactor No. 60 (Dentsply/Maillefer Instruments S.A., Ballaigues, Switzerland; Tulsa, Oklahoma, USA) calibrated at 4 mm below the WL. The compactor, driven clockwise in the low-rotating piece, was introduced and withdrawn from the moving canal. After the gutta-percha plastification and removal of the activated McSpadden® from the canal, the vertical condensation of the gutta percha was carried out using the Paiva instrument No. 2 (SS White, Rio de Janeiro, Rio de Janeiro, Brazil; Lakewood, New Jersey, USA).
After an obturation of all samples, they were temporarily restored with Cavitec and immersed in a bottle containing distilled water in an oven at 37°C and relative humidity to 100% for 2 days to complete setting of the endodontic sealer.
Protocol for removal of gutta percha from the canal and cementing the fiberglass post
After removal of the restoration, the removal of gutta percha from the canals was done with the aid of a 12 mm drill DC2 (Whitepost, FGM, Joinville, Santa Catarina, Brazil) at low rotation, remaining 4 mm of the obturator material in the apical third.
Prior to the cementation of the fiberglass posts, the canals were irrigated with 2.5% sodium hypochlorite solution and dried with absorbent paper points, as recommended by the adhesive cement manufacturer.
On the dried canals, silane (FGM Produtos Odontológicos, Joinville, Santa Catarina, Brazil) was applied. Drying at room temperature followed by application of air jets at a distance of 15 cm for 1 minute. The resinous cement RelyX U200 (3M/ESPE, Saint Paul, Minnesota, USA) was applied to the root canal using a centrix syringe (DFL, Rio de Janeiro, Rio de Janeiro, Brazil) with a metal tip. The post was introduced into the root canal and filled with cement to the coronal portion to seal the entrance and photoactivated with the EC450 (ECEL, Ribeirão Preto, São Paulo, Brazil) for 40 seconds. The fiberglass posts used in the experiment were No. 2 (Angelus, Londrina, Paraná, Brazil). They were cleaned prior to use with 70% alcohol (Icarai, São Paulo, São Paulo, Brazil).
Shear extrusion test (push-out)
The samples were sectioned perpendicular to the long axis of the root, with a diamond disk (American Burrs, Porto Alegre, Rio Grande do Sul, Brazil) at a low rotation under refrigeration. A first cervical portion approximately 1 mm thick was discarded, as inherent imperfections in the adhesive zone may have influenced the results due mainly to the presence of oxygen. Then three slices of approximately 1 mm thickness each were obtained — one from the cervical third, one from the middle third, and the other from the apical third. After cutting each slice, markings were made with an overhead pen on the cervical surface of the sample to highlight this face for later positioning of the piece on the time of the test. Then during the push-out test, each sample was placed on a metal device with a central opening larger than the canal diameter. The slices always remained with the cervical side down, facilitating the extrusion of the canal post/cement, which already presents a conical shape, thus leaving the larger part of the diameter down. For the push-out test, an adapted metal cylinder (Ø = 1 mm) induced the load on the central portion of the post/cement without the load being applied to the dentin (Figure 1).
The test was performed in a universal test machine (EMIC, São José dos Pinhais, Paraná, Brazil) with a velocity of 0.5 mm/min and a load of 50 N (newton). The results were recorded in newton and later converted to MPa (MegaPascal). The adhesion area (A) was calculated by the formula (2TTr) multiplied by the height (L). The force (F) that occurred resulting in the fault was recorded in N and converted to MPa. The adhesive resistance to push-out was measured by dividing the force (F) by the adhesion area (A).
Statistical analysis
The obtained data was submitted to two-way ANOVA tests for multiple comparisons. The level of significance was 5% (P ≤ 0.05). Statistical analysis was performed using SPSS 13.0 software (SPSS Inc., Chicago, Illinois, USA).
Results
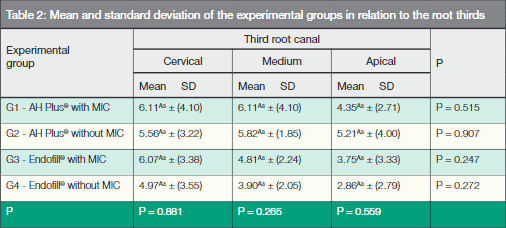
The mean values of the adhesion forces (map) of the different experimental groups in the different regions of the canals are shown in Table 2.
Means followed by distinct uppercase letters in the line and means followed by different lowercase letters in the line differ significantly by means of the analysis of variance at the significance level of 5%.
The ANOVA two-way statistical test did not show any statistical difference between the experimental groups, whether or not calcium hydroxide-based intracanal medication and endodontic sealer were used, regardless of the thirds of the roots on the evaluated canal.
Discussion
The use of prefabricated intraradicular esthetic posts such as fiberglass represents a treatment option that offers optimal esthetics and function, which can be fixed by adhesion to root dentin. However, innumerable factors related to the endodontic approach may influence the clinical success of this rehabilitation technique throughout the time of preservation.
The mechanical push-out test method used is one of the research resources used to measure adhesive strength of materials (Armstrong, et al., 2010). According to Soares, et al. (2008), this method provides a more homogeneous distribution of tensions and less variability in the calibration process, thus preservation recommended and widely used to determine the bond strength of fiberglass posts to intrarradicular dentin.
The results obtained, regarding the adhesion strength of intrarradicular cemented fiberglass posts, did not show an influence in relation to the type of endodontic sealer tested, as verified in the studies of Manicardi, et al. (2011) and Aggarwal, et al. (2012). Similar results were found by Shokouhinejad, et al. (2013) that compared the AH-Plus® and EndoSequence BC® sealers, which is a bioceramic sealer. On the other hand, Zhu, et al. (2006) found that endodontic sealer containing eugenol (Endofill®) may compromise the bond strength of intraradicular fiberglass posts when compared to resinous composites such as AHPlus. In the study by Mosharraf and Zare (2014), with the use of eugenol-based sealer (Endofill), there was a significant reduction in union strength by the push-out test between intraradicular fiberglass posts when compared to AH26®, which is a resinous sealer.
Rosa, et al. (2013) also performed a study to evaluate the influence of the endodontic sealer type (Endofill, AH Plus, and MTA Fillapex) on the adhesion of fiberglass posts to the bovine dentin root through the push-out test. The authors evaluated the cementation process of the posts in two experimental times, immediate cementation, that is, after the endodontic obturation and cementation after 15 days of obturation. They could observe that when the fiberglass posts were cemented immediately, the adhesive strength was similar regardless of the type of endodontic sealer tested. However, after 15 days, teeth sealed with resin-based epoxy resin (AH Plus) presented the highest values of adhesive strength, which may help explain in a way the results obtained in the present study, since it is probable that the reduced time (48 hours) between completion of endodontic treatment and cementation of the fiberglass post may not have been able to influence the adhesion difference between the experimental groups.
The presence of eugenol (2-methoxy-4-allylphenol) and phenolic components in the composition of the endodontic sealer can deactivate the polymer chain molecules and compromise the cementation process of the intraradicular post, decreasing the bond strength (Dias, et al., 2009; Demiryurek, et al., 2010; Aleisa, et al., 2012). This factor doesn’t seem to have influenced the adhesive strength of the studied groups. The authors believe that the reduced time between canal obturation and disembedding may have been the most relevant factor in the good result obtained in this study.
For Davis and O’Connell (2007), a correct root canal cleansing protocol prior to adhesive cementation of the intraradicular post is essential to reduce interference and increase the bond strength.
Regarding the influence in the adhesion process from the use of intracanal medication in the previous endodontic treatment, no statistical differences were obtained between the groups, corroborating with the study of Erdermir, et al. (2004), who used chlorhexidine digluconate and calcium hydroxide as a medication.
Lambrianidis, et al. (2006) and Balvedi, et al. (2010), who evaluated different forms of calcium hydroxide-based intracanal medication, found that traces of calcium hydroxide in the walls of the root canal may impair the cementation and adhesion process of intraradicular posts. Calcium hydroxide reduces dentin permeability by physical blockage of the dentin tubules (Ngoh, et al., 2001) and by the chemical interaction between the RelyX self-adhesive cement and the calcium hydroxyapatite of the dentin wall as observed by Pashley, et al. (1986); Balvedi, et al. (2010), and Gerth, et al. (2006), who obtained lower results in the adhesion force when calcium hydroxide-based intracanal medication was previously used.
Conclusions
According to the results, it can be concluded that the use of calcium hydroxide-based intracanal medication as well as the type of endodontic sealer tested (AH Plus or Endofill) did not interfere in the adhesion strength of fiberglass posts cemented intraradicular with RelyX U200.
- Aggarwal V, Singla M, Miglani S, Kohli S. Effect of different root canal obturating materials on push-out bond strength of a fiber dowel. J Prosthodont. 2012;21(5):389-392.
- Aleisa K, Alghabban R, Alwazzan K, Morgano SM. Effect of three endodontic sealers on the bond strength of prefabricated fiber posts luted with three resin cements. J Prosthet Dent. 2012;107(6):322-326.
- Armstrong S, Geraldeli S, Maia R, Raposo LH, Soares CJ, Yamagawa J . Adhesion to tooth structure: a critical review of “micro” bond strength test methods. Dent Mater. 2010;26(2):50-62.
- Balvedi RP, Versiani MA, Manna FF, Biffi JC. A comparison of two techniques for the removal of calcium hydroxide from root canals. Int Endod J. 2010;43(9):763-768.
- Cohen BI, Volovich Y, Musikant BL, Deutsch AS. The effects of eugenol and epoxy-resin on the strength of a hybrid composite resin. J Endod. 2002;28(2):79-82.
- Davis ST, O’Connell BC. The effect of two root canal sealers on the retentive strength of glass fiber endodontic posts. J Oral Rehabil. 2007;34(6):468-473.
- Demiryürek EO, Külünk S, Yüksel G, Saraç D, Bulucu B. Effects of three canal sealers on bond strength of a fiber post. J Endod. 2010;36(3):497-501.
- Dias LL, Giovani AR, Silva Sousa YT, et al. Effect of eugenol-based endodontic sealer on the adhesion of intraradicular posts cemented after different periods. J Appl Oral Sci. 2009;17(6):579-583.
- Erdemir A, Ari H, Güngünes H, Belli S. Effect of medications for root canal treatment on bonding to root canal dentin. J Endod. 2004;30(2):113-116.
- Ferrari M, Mannocci F. A ‘one-bottle’ adhesive system for bonding a fiber post into a root canal: an SEM evaluation of the post-resin interface. Int Endod J. 2000;33(4):397-400.
- Fonseca RB, Martins LR, Quagliatto PS, Soares CJ. Influence of provisional cements on ultimate bond strength of indirect composite restorations to dentin. J Adhes Dent. 2005;7(3):225-230.
- Gerth HU, Dammaschke T, Züchner H, Schäfer E. Chemical analysis and bonding reaction of RelyX Unicem and Bifix Composites — a comparative study. Dent Mater. 2006;22(10):934-941.
- Lambrianidis T, Kosti E, Boutsioukis C, Mazinis M. Removal efficacy of various calcium hydroxide/chlorhexidine medicaments from the root canal. Int Endod J. 2006;39(1):55-61.
- Manicardi CA, Versiani MA, Saquy PC, Pécora JD, de Sousa-Neto MD. Influence of filling materials on the bonding interface of thin-walled roots reinforced with resin and quartz fiber posts. J Endod. 2011;37(4):531-537.
- Monticelli F, Osorio R, Albaladejo A, et al. Effects of adhesive systems and luting agents on bonding of fiber post to root canal dentin. J Biomed Mater Res B Appl Biomater. 2006;77(1):195-200.
- Mosharraf R, Zare S. Effect of type of endodontic sealer on the bond strength between fiber post and root wall dentin. J Dent (Tehran). 2014;11(4):455-463.
- Ngoh EC, Pashley DH, Loushine RJ, Weller RN, Kimbrough WF. Effects of eugenol on resin bond strengths to root canal dentin. J Endod. 2001;27(6):411-414.
- Pashley DH, Depew DD. Effects of the smear layer, Copalite, and oxalate on microleakage. Oper Dent. 1986;11(3):95-102.
- Paul SJ, Schärer P. Post and core reconstruction for fixed prosthodontic restoration. Pract Periodontics Aesthet Dent. 1997;9(5):513-520.
- Rosa RA, Barreto MS, Moraes Rdo A, et al. Influence of endodontic sealer composition and time of fiber post cementation on sealer adhesiveness to bovine root dentin. Braz Dent J. 2013;24(3):241-246.
- Shokouhinejad N, Gorjestani H, Nasseh AA, Hoseini A, Mohammadi M, Shamshiri AR. Push-out bond strength of gutta-percha with a new bioceramic sealer in the presence or absence of smear layer. Aust Endod J. 2013;39(3):102-106.
- Soares PV, Santos-Filho PC, Martins LR, Soares CJ. Influence of restorative technique on the biomechanical behavior of endodontically treated maxillary premolars. Part I: Fracture resistance and fracture mode. J Prosthet Dent. 2008;99(1):30-37.
- Souza-Júnior EJ, Bueno VC, Dias CT, Paulillo LA. Effect of endodontic sealer and resin luting strategies on pull-out bond strength of glass fiber posts to dentin. Acta Odontol Latinoam. 2010;23(3):216-221.
- Watanabe EK, Yamashita A, Imai M, Yatani H, Suzuki K. Temporary cement remnants as an adhesion inhibiting factor in the interface between resin cements and bovine dentin. Int J Prosthodont. 1997;10(5):440-452.
- Zhu S, Liu C, Zheng Z, Yang L, Gao X. Analysis of different endodontic sealers and strategies of root canal irrigation on the bond strength of fiber posts. Hua Xi Kou Qiang Yi Xue Za Zhi. 2015;33(3):311-314.
Stay Relevant With Endodontic Practice US
Join our email list for CE courses and webinars, articles and more..

