CE Expiration Date:
CEU (Continuing Education Unit): Credit(s)
AGD Code:
Educational aims and objectives
This article aims to explain with illustrations the clinical reasons for the cortical window technique in endodontics.
Expected outcomes
Endodontic Practice US subscribers can answer the CE questions by taking the quiz to earn 2 hours of CE from reading this article.
Correctly answering the questions will demonstrate the reader can:
- Identify when and how to perform the cortical window technique.
- Identify some characteristics of piezo surgery in microsurgical endodontics.
- Realize what part ultrasound plays in the piezo surgery process.
- Recognize some drawbacks to traditional osteotomies.
- Recognize the positive role of CBCT in the cortical window technique.
The cortical window technique is a minimally invasive approach to accessing the roots that allows for maximum regenerative potential. Read about this interesting microsurgical approach that enhances treatment outcomes!
Drs. Naheed Mohamed, Yosi Nahmias, and Ken Serota discuss the evolution of endodontic surgery in the first of this 2-part article

Nonsurgical endodontic therapy requires access preparations that uncover entrances to the labyrinthine tunnels of the root canal system. The era of bio-minimalism has altered the traditional configuration of endo-dontic access cavities. These bio-minimalistic trends are also transforming endodontic surgery (Wang, et al., 2004). The use of surgical operating microscopes (Global Surgical Corporation) facilitates smaller crypt sizes and reduces the volume of bone removed. The wound architecture created by microsurgical scalpels (Kerr Hawe) is more precise resulting in minimal damage to the soft tissues (Tsesis, et al., 2013). Enhanced visibility facilitates perpendicular resection of the apical segment to the long axis of the root. Monofilament sutures (Johnson & Johnson® Ethicon®) minimize posttreatment inflammation. Soft and hard tissue augmentation corrects deficits in biotype and buttressing bone. These are but a few of the new adjuncts in endodontic microsurgical techniques (Tsesis, et al., 2013; Kim and Katchman, 2006; Setzer, et al., 2012).
Ultrasonic osteotomy
Used in both periodontal and implant surgery, piezo surgery in microsurgical endodontics produces micrometric cuts that diminish cortical bone loss and retain root length. Saline pumped through irrigation lines cools the piezotome tip (NSK, UK) (Figure 1). In deep spaces, ultrasonic vibrations break down the irrigation into very small particles readily suctioned from the surgical field. Reduction of heme in the crypt minimizes the use of hemostatic agents and interference with the setting of retro-seal materials. The inclusion of piezo surgery in endodontic microsurgical protocols produces less morbidity during the healing phase.
Ultrasound consists of mechanical waves of frequencies greater than 20 kHz. Generated by transducers (lead zirconate titante), electrical energy is converted to ultrasonic waves with minimal heat production. The clinician controls the pressure applied, cutting frequency, pulse frequency, rate of delivery of coolant fluid, and power (3-90 watts). Minimal heat generation on cutting creates lower proinflammatory cytokine levels, an earlier increase in BMP4 and TGF2 and more active neo-osteogenesis (Vercellotti, 2009; Abella et al, 2014).
Traditional osteotomies require large instruments to remove cortical bone in order to access the apical segment of the root. These instruments can lead to delayed healing, increased postoperative pain, and/or complications. With microscopes and piezotome surgical tips, smaller osteotomies (less than 5 mm) are big enough to accommodate ultrasonic tips (tip length of 3 mm).
Cortical window technique
Dental radiographs are essential to all aspects of endodontics. Historically, they were two-dimensional images of three-dimensional structures; as such, data interpretation was subjective. The introduction of cone beam computed tomography (CBCT) and digital volume technology (DVT) provides images in sagittal, axial, and coronal planes showing previously indeterminable views (Venskutonis, et al., 2014; Leonardi Butra, et al., 2016). The three-dimensional data gathered from the CBCT scan allows a pre-planned window to be made to access the apical portion of the roots. The use of CBCT imaging in conjunction with piezo surgery provides a precise and less traumatic outline for the cortical bone window in contrast to traditional free-hand guided crypt creation. The cortical bone window is sectioned so that the facial or palatal wall converges from the external surface to the internal surface. This ensures accuracy of removal of the cortical bone plate and re-seating when the window is replaced.




Case report
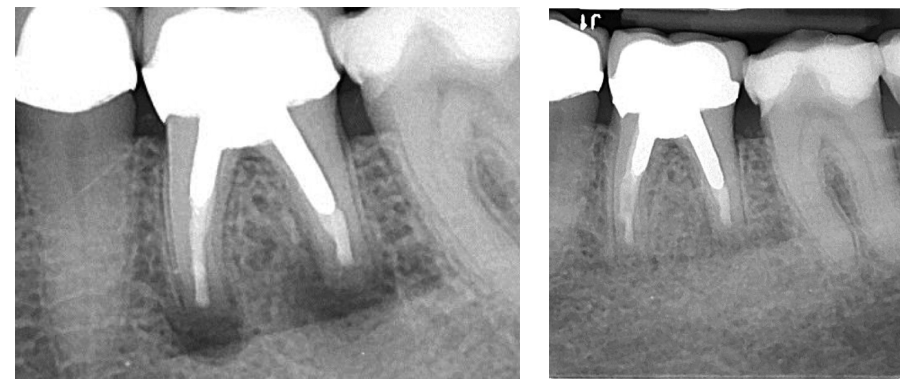
A female patient was seen for consultation regarding tooth LL6. She reported that pain on biting had developed over the past week and intensified day to day. Her generalist took a periapical radiograph and advised the patient that something was amiss. A prescription for amoxicillin (500 mg) was provided, and she was referred to our surgery. Tooth LL6 was percussion sensitive. A two-dimensional radiographic examination revealed a prior root canal procedure, a PFM crown and cast post core in the mesial-buccal and distal canals. The suggestion of a second distal canal was noted (Figure 3).
A cone beam tomography scan was recommended as the tomographic volumes would elicit more accurate diagnostic information; the patient concurred, and was referred to a dental radiologist (www.canaray.com). The CBCT (Figure 4) showed that the apex of the distal root demonstrated rarefying osteitis. In addition, the apical third of the distal root was under-instrumented and under-filled, which contributed to persistent apical pathology. The mesial root appeared normal radiographically. Retreatment as an option was discussed, however, the risk factors involved, removal of the crown/post core, and retreatment of the root canal system, were deemed have an uncertain prognosis. Other options were discussed including consideration for extraction and implant replacement. The patient agreed to have microsurgical treatment using a cortical bone window access — a sagittal view (CBCT) was used to determine the width and height of the cortical window needed (Figure 2A). The coronal view shows the facial lingual width and the position of the inferior alveolar nerve (Figure 2B) — the relation of the lesion between facial and lingual cortical place determines depth of the surgical crypt and the its proximity to the inferior alveolar nerve. The clinical examination identified generalized recession and diminished attached gingiva about the facial aspect of LL4 and the mesial root of LL6 (Figure 5A).




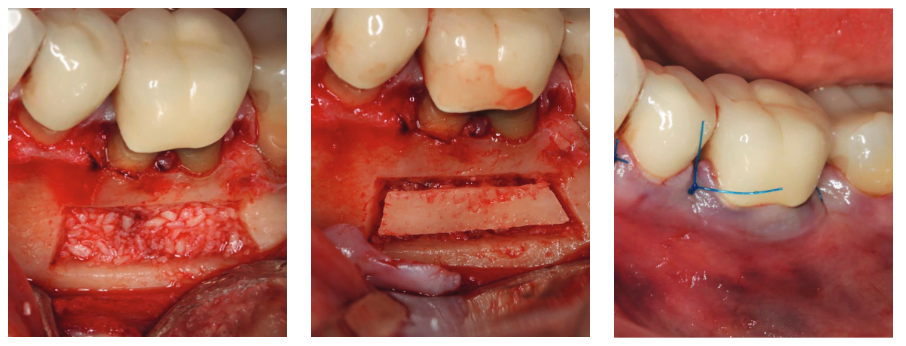

Anesthesia was obtained using Xylocaine 2% with epinephrine 1:100,000 (Dentsply Sirona) for the IAN (inferior alveolar nerve) and Xylocaine 2% with epinephrine 1:50,000 (Dentsply Sirona) was used for regional infiltration. A surgical operating microscope was used, and the principles of modern microsurgical endodontics (Vercellotti, 2009) were applied. A full thickness intra-sulcular flap was incised with a microsurgical blade, which minimizes trauma and loss of the interdental dental papilla especially in areas of recession and thin biotype (Figure 5B). The piezotome was used to cut the cortical window. The cortical window was angled convergent from the external surface to the internal surface and wider at the base, which prevents the plate from sinking internally when repositioned as discussed previously (Figure 6).
The window was removed by luxation (Figure 7) from a thin chisel and placed in sterile saline. The apices are resected at a 0º angle preserving root length exposing the lingual anatomy, centering the canals, eliminating accessory canals, and minimizing the number of exposed dentinal tubules. The canal is retro-prepared (ProUltra® tips, Dentsply-Sirona) retro-sealed using Super EBA (Keystone Dental) (Sullivan, et al., 1999)(Figure 8).
The crypt is filled with freeze-dried allograft (0.5 cc Mineralized Cortical GC, Straumann®) (Figure 9). The cortical window is replaced (Figure 10) and the wound (flap) sutured using 6-0 prolene sutures (Ethicon®) (Figure 11). The postoperative radiograph is shown (Figure 12). The reassessment radiograph taken 6 months later demonstrates almost complete osseous regeneration (Figure 13). The patient is asymptomatic, the procedure has retained substantial root length, and a long-term positive treatment outcome is expected (Figure 14).
Conclusion
The basic framework of endodontic surgery by incorporation of interdisciplinary precepts has evolved into endodontic microsurgery. The benefits of this cortical window approach include greater access the roots for better visibility without greater risk for bone loss. The minimally invasive approach to access the roots by way of removal of a cortical bone plate has its greatest advantage simply due to the fact that the bone plate is conserved and then replaced, allowing maximum regenerative potential. Advances in the surgical armamentarium, based on biological concepts has enabled a microsurgical approach, which ensures enhanced positive treatment outcomes. The past is not being rejected; the future is being embraced. It is the natural progression of all things.
Besides the cortical window technique, microsurgery provides advantages in other procedures as well. Read Dr. Leandro A.P. Pereira’s CE, “Microsurgical management for correction of a procedure error in the phase of apical mechanical preparation in endodontics: apical transport,” to continue expanding your microsurgical horizons!
References
- Abella F, de Ribot J, Doria G, Duran-Sindreu F, Roig M. Applications of piezoelectric surgery in endodontic surgery: a literature review. J Endod. 2014;40(3):325-332.
- Leonardi Dutra K, Haas L, Porporatti AL, et al. Diagnostic accuracy of cone-beam computed tomography and conventional radiography on apical periodontitis: a systematic review and meta-analysis. J Endod. 2016;42(3):356-364.
- Kim S, Kratchman S. Modern endodontic surgery concepts and practice: a review. J Endod. 2006;32(7):601-623.
- Setzer FC, Kohli MR, Shah SB, Karabucak B, Kim S. Outcome of endodontic surgery: a meta-analysis of the literature — Part 2: Comparison of endodontic microsurgical techniques with and without the use of higher magnification. J Endod. 2012;38(1):1-10.
- Sullivan JE Jr, Da Fiore PM, Heuer MA, Lautenschlager EP, Koerber A. Super-EBA as an endodontic apical plug. J Endod. 1999;25(8):559-561.
- Tsesis I, Rosen E, Taschieri S, et al. Outcomes of surgical endodontic treatment performed by a modern technique: an updated meta-analysis of the literature. J Endod. 2013;39(3):332-339.
- Venskutonis T, Plotino G, Juodzbalys G, Mickevičienė L. The importance of cone-beam computed tomography in the management of endodontic problems: a review of the literature. J Endod. 2014;40(12):1895-1901.
- Vercellotti T. Essentials in Piezosurgery: Clinical Advantages in Dentistry. Italy: Quintessence Publishing; 2009.
- Wang N, Knight K, Dao T, Friedman S. Treatment outcome in endodontics — The Toronto Study. Phases I and II: apical surgery. J Endod. 2004;30(11):751-761.

