Dr. John West explores the significance of the lateral canal

This question has been asked of endodontists as long as I can remember. Many of us remember spirited 1970s debates between Dr. Herbert Schilder and Dr. Frank Weine. When I went to dental school, we were taught that if we “instrument and fill the mother canal” we could expect a 95% success rate. Dr. Schilder, however, taught his students “all foramina are potentially significant.” Which thinking is right? Do lateral canals matter? And what is a lateral canal anyway?
Is it biology or just “the look?”
First, in order to determine the biologic determinants of endodontic predictability, there is the biologic question. Am I willing to leave that answer to our scientists and academicians? Second, I do not distinguish “lateral canal.” Nature doesn’t either. Nature simply creates root canal “systems” with portals of exit (POEs). What if a canal divides into two apical POEs of equal length in the last 2 to 4 mm? Which one is the lateral canal? Which one don’t you want if lateral canals do not matter? As endodontic clinicians, we want them both. We want them all. In my experience the “lateralness” of a lateral canal does not matter since even furcal “lateral” canals can cause and/or prevent lesions of endodontic origin.4
Even if clinicians do not think lateral canals matter, they are always excited and proud if they pack one. I remember a colleague showing me a radiograph of a central incisor with his filled lateral canal using lateral condensation. It was the first demonstrable lateral canal he filled in over 15 years! Really, that’s what it’s all about. Demonstrating multiple radiographic POEs is a signature outcome. We know from studying all the teeth in the ToothAtlas.com that there are approximately 2.5 POEs on average for every canal.1 Getting them means the clinician has usually accomplished most, if not all, of the following:
- Unrestricted access, dentin triangles removed while safeguarding precious restorative ferrule dentin
- Appropriately shaped canals with smooth walls and a continuously tapering funnel design where the clinician has preserved the original position and size of the shaped canal, i.e., FLOW
- The root canal system has been cleaned of necrotic debris, detached pulpal tissue, dentin shavings and mud, biofilm, and smear layer
- Proper conefit
- Vertical compaction of warm gutta percha or carrier-based obturation, thereby delivering heat and pressure at the foraminal sites. It means you have created the possibility to seal multiple POEs where they exist. The clinical does not find the “lateral” canal; the obturation hydraulics system finds the lateral canal, which could be in any position along the tunnel geometry of the shaped canal itself.
As a clinician and educator for over 35 years, I am often asked by students if I have a patient where I could demonstrate that a lateral canal matters. Actually, all endodontists can produce these examples if the patients are carefully followed.
Lateral canal matters: case report
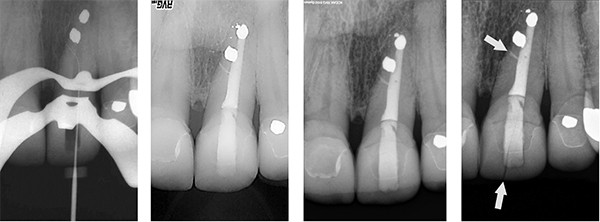
In this issue of Anatomy Matters, I report on a 25-year posttreatment where a “lateral” canal matters. In 1988, the patient presented with soreness over facial of the maxillary left central incisor (Figure 1). A radiograph demonstrated the patient had experienced previous nonsurgical endodontics followed by a surgical endodontic retreatment. In addition, a lateral radiolucency incisal to the apparent lateral canal surgical seal was observed. After reviewing treatment options, the patient, referring restorative dentist, and I choose to nonsurgically attempt to seal the root canal system with the anticipation of an underfilled or unfilled lateral canal. After gutta-percha removal with heat and solvents, I was able to slide into a lateral POE with a No. 6 manual file, which can be seen approximately 2 mm incisal to the amalgam retrofilled apparent lateral canal (Figure 2). The root canal system was cleaned and shaped incisal to the apical amalgam, which tested solid and sealed. Vertical compaction of warm gutta-percha was performed with clear obturation of lateral canal that had been cleaned to size 10 manual file (Figure 3). Twenty-year posttreatment validates radiographic healing of the lesion of endodontic origin with reconstitution of the attachment apparatus and the lamina dura (Figure 4).
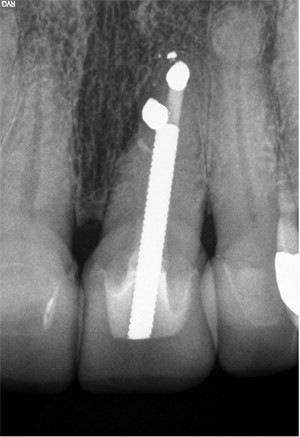
canal and robust post placement, foundation, and new crown.
In 2010, the patient returned with a fractured crown but without endodontic symptoms (Figure 5). Dr. John Kois, a superb clinician and educator in Seattle, Washington, restored the crown with a robust post/foundation, and 3 years later, in 2013, the tooth continues to “feel good,” is asymptomatic, and “looks good” to the patient (Figures 6 and 7).
For me, endodontics has a golf metaphor. The golf pro tells me that in order to finish the golf swing properly, I need to be “scratching my back” with the club and facing the ball path. That finish position means all the right things had to happen properly: position to desired path and stance relative to the ball, proper grip, back swing and nice flat plane, the swinging club forward through the same plane, proper body position of swing from beginning to end, and then the finish or follow-through. Endodontics is the same way. If you consistently visibly obturate multiple POEs, you have disciplined yourself, just like the golf pro, to do all the right things that increase your Endodontic Seal probability and performance.
And remember, some clinicians that may be a little heavy-handed discover that their first lateral canal may actually be their first canal!

So, do lateral canals matter? For this patient it did. And while we do not have scientific control to prove the importance the lateral canal plays in endodontic predictability, there are most certainly cause and effect documentations. The cause for the patient in this report was an undersealed root canal system causing a symptomatic tooth with a lateral radiolucency. The root canal system was treated and 25 years later shows that sustained healing has occurred by all biologic and radiographic standards. The only difference in the before and after: a sealed lateral canal. Anatomy Matters once more.
- West J. How do masters do it. Presented at: American Association of Endodontists; 2012; Boston, MA.
- West J. Anatomy matters. Endodontic Practice US. 2012;5(2):14-16.
- West J. Anatomy matters — part 2. Endodontic Practice US. 2012;5(4):26-27.
- West J. Anatomy matters — part 3. Furcal endodontic seal heals furcal lesion of endodontic origin. Endodontic Practice US. 2012;5(6):22-24.
- West J. Anatomy matters. Long-term case report. Endodontic Practice US. 2013;6(1):50-51.
- West J. Anatomy matters. Root canal system anatomy only matters when it matters. Endodontic Practice US. 2013;6(2):56-58.
Stay Relevant With Endodontic Practice US
Join our email list for CE courses and webinars, articles and more..

 John West, DDS, MSD, the founder and director of the Center for Endodontics, continues to be recognized as one of the premier educators in clinical and interdisciplinary endodontics. Dr. West received his DDS from the University of Washington in 1971 where he is an affiliate associate professor. He then received his MSD in endodontics at Boston University Henry M. Goldman School of Dental Medicine in 1975 where he is a clinical instructor and has been awarded the Distinguished Alumni Award. Dr. West has presented more than 400 days of continuing education in North America, South America, and Europe while maintaining a private practice in Tacoma, Washington. He co-authored “Obturation of the Radicular Space” with Dr. John Ingle in Ingle’s 1994 and 2002 editions of Endodontics and was senior author of “Cleaning and Shaping the Root Canal System” in Cohen and Burns 1994 and 1998 Pathways of the Pulp. He has authored “Endodontic Predictability” in Dr. Michael Cohen’s 2008 Quintessence text Interdisciplinary Treatment Planning: Principles, Design, Implementation, as well as Dr. Michael Cohen’s soon to be published Quintessence text Interdisciplinary Treatment Planning Volume II: Comprehensive Case Studies. Dr. West’s memberships include: 2009 president and fellow of the American Academy of Esthetic Dentistry, and 2010 president of the Academy of Microscope Enhanced Dentistry, the Northwest Network for Dental Excellence, and the International College of Dentists. He is a 2010 consultant for the ADA’s prestigious ADA Board of Trustees where he serves as a consultant to the ADA Council on Dental Practice. Dr. West further serves on the Henry M. Goldman School of Dental Medicine’s Boston University Alumni Board. He is a Thought Leader for Kodak Digital Dental Systems, and serves on the editorial advisory boards for: The Journal of Esthetic and Restorative Dentistry, Practical Procedures and Aesthetic Dentistry, and The Journal of Microscope Enhanced Dentistry. Visit
John West, DDS, MSD, the founder and director of the Center for Endodontics, continues to be recognized as one of the premier educators in clinical and interdisciplinary endodontics. Dr. West received his DDS from the University of Washington in 1971 where he is an affiliate associate professor. He then received his MSD in endodontics at Boston University Henry M. Goldman School of Dental Medicine in 1975 where he is a clinical instructor and has been awarded the Distinguished Alumni Award. Dr. West has presented more than 400 days of continuing education in North America, South America, and Europe while maintaining a private practice in Tacoma, Washington. He co-authored “Obturation of the Radicular Space” with Dr. John Ingle in Ingle’s 1994 and 2002 editions of Endodontics and was senior author of “Cleaning and Shaping the Root Canal System” in Cohen and Burns 1994 and 1998 Pathways of the Pulp. He has authored “Endodontic Predictability” in Dr. Michael Cohen’s 2008 Quintessence text Interdisciplinary Treatment Planning: Principles, Design, Implementation, as well as Dr. Michael Cohen’s soon to be published Quintessence text Interdisciplinary Treatment Planning Volume II: Comprehensive Case Studies. Dr. West’s memberships include: 2009 president and fellow of the American Academy of Esthetic Dentistry, and 2010 president of the Academy of Microscope Enhanced Dentistry, the Northwest Network for Dental Excellence, and the International College of Dentists. He is a 2010 consultant for the ADA’s prestigious ADA Board of Trustees where he serves as a consultant to the ADA Council on Dental Practice. Dr. West further serves on the Henry M. Goldman School of Dental Medicine’s Boston University Alumni Board. He is a Thought Leader for Kodak Digital Dental Systems, and serves on the editorial advisory boards for: The Journal of Esthetic and Restorative Dentistry, Practical Procedures and Aesthetic Dentistry, and The Journal of Microscope Enhanced Dentistry. Visit 