Dr. Jeffrey Krupp has become an avid fan of the physical and biological properties of ENDOSEAL MTA. Read his article to discover his many reasons.
Dr. Jeffrey D. Krupp discusses the excellent physical and biological properties of this obturation material
Root canal fillings aim to seal the root canal system to prevent reinfection of the periapex. Obturation should eliminate all routes of leakage from the oral cavity and the periradicular tissues into the root canal system by creating a fluid-tight seal. Therefore, root canal filling materials and endodontic sealers should seal the canal laterally and apically and have good adaptation to the root canal dentin.1,2
The arrival of bioceramic endodontic sealers to the clinical endodontics playing field is highly therapeutic. The introduction and increased use of these advanced materials facilitates the main objectives of endodontic obturation. Their chemical formulation and biological properties have shifted the field from using biologically inactive materials to utilizing biologically active materials. We have therefore progressed from a physical endodontic seal of inactive materials to a biological endodontic seal of active materials by way of biomineralization of dentin with bioceramic sealers.
The first bioceramic material successfully used in endodontics was the mineral trioxide aggregate (MTA) cement, which was introduced by Dr. Mahmoud Torabinejad in 1993. It is osseoconductive, inductive, and biocompatible.3 ENDOSEAL MTA (Maruchi; Wonju, Korea) is a paste-type root canal sealer based on pozzolan cement that has the same excellent physical and biological properties of traditional MTA.
ENDOSEAL MTA is a radiopaque, non-resorbable paste for the permanent obturation of the root canal system. Its composition is well tolerated by the tissues and provides anti-inflammatory, antiseptic, and germicidal actions.4
The sealer is produced in a syringe, unlike many existing products composed of powder and liquid. This means it can be directly injected into the canal system without a rigorous mixing process. In addition, calcium hydroxide produced is released during the setting process to induce hard tissue formation, which has been shown to have a strong antimicrobial effect against E. faecalis. Another beneficial characteristic is that the sealer expands 2% upon setting, rather than shrinking like traditional endodontic sealers. This allows for a better three-dimensional fill.
After using the ENDOSEAL MTA for a few years, I have personally noticed that the high biocompatibility of this product has minimized patient post-op discomfort. The material is easy to handle as it does not require an arduous mixing process and can be directly injected into the canal. During obturation, the flow of the material appears seamless, not trapping air while flowing in three dimensions.
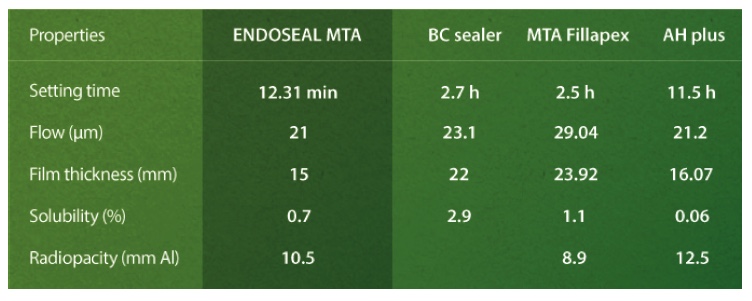
ENDOSEAL MTA, one of the latest and most extensively tested obturation materials, excels with high biocompatibility, excellent antimicrobial properties, exceptional flow, expansion during setting, high radiopacity, low solubility in contact with tissue fluids, and a substantially shortened setting time (in mere minutes).5-8
The rapid-setting ability of ENDOSEAL MTA creates a completely new repertoire of clinical applications and improves appointment efficiency compared to past MTA and bioceramic sealers that required hours or days to set. In past generations of MTA/bio-ceramic sealers, clinical applications beyond obturation were limited due to the risk of the material washout in procedures such as pulp capping, perforation repair, and root-end surgery. These procedures would require a more substantive and more difficult-to-use MTA/bioceramic material, necessitating additional appointments to confirm full set of the material. On the other hand, ENDOSEAL MTA’s patented formulation uses pozzolan reactions to quicken setting times without adding chemical catalysts that disrupt biocompatibility and bioactivity. Its novel pozzolan cement-based formulation also promotes intratubular biomineralization.9,10
For all of the above reasons and its ease-of-use in my hands, I have become an avid user of the ENDOSEAL MTA sealer. As the field of endodontics evolves with novel and improved technologies and materials, we can truly benefit from evolving along with it.
Learn more by visiting: https://maruchiusa.com/
The physical and biological properties of MTA are just one of the many issues that face endodontists each day. Read more of Dr. Krupp’s insights on the specialty in “Evolving clinical intuition and professionalism: knowing when to swing at the pitch.”
https://endopracticeus.com/columns/evolving-clinical-intuition-professionalism-knowing-swing-pitch/
- Özcan E, Eldeniz AU, Arı H. Bacterial killing by several root filling materials and methods in an ex vivo infected root canal model. Int Endod J. 2011;44(12):1102-1109.
- Singh Chandra, Rao S, Chandrashekar, V An in vitro comparison of penetration depth of two root canal sealers: An SEM study. J Conserv Dent. 2012;15(3):261–264.
- Parirokh M, Torabinejad M. Mineral trioxide aggregate: a comprehensive literature review — Part I: chemical, physical, and antibacterial properties. J Endod. 2010;36(1):16-27.
- Endoseal . https://www.indiamart.com/proddetail/endoseal-root-canal-obturation-cement-21208201662.html. Accessed January 30, 2020.
- Kaur A, Shah N, Logani A, Mishra N. Biotoxicity of commonly used root canal sealers: a meta-analysis. J Conserv Dent. 2015;18(2):83-88.
- Ørstavik D. Materials used for root canal obturation: technical, biological and clinical testing. Endodontics Topics. 2005;12(1):25-38.
- Al-Haddad A, Che Ab Aziz ZA. Bioceramic-Based Root Canal Sealers: A Review. Int J Biomaterials. 2016.
- Lee BN, Hwang YC, Jang JH, et al. Improvement of the properties of mineral trioxide aggregate by mixing with hydration accelerators. J Endod. 2011;37(10):1433-1438.
- Lee JK, Kwak SW, Ha JH, Lee W, Kim HC. Physicochemical Properties of Epoxy Resin-Based and Bioceramic-Based Root Canal Sealers. Bioinorg Chem Appl. 2017.
- Yoo YJ, Baek SH, Kum KY, et al. Dynamic intratubular biomineralization following root canal obturation with pozzolan-based mineral trioxide aggregate sealer cement. Scanning. 2016; 38(1):50-56.
Stay Relevant With Endodontic Practice US
Join our email list for CE courses and webinars, articles and more..