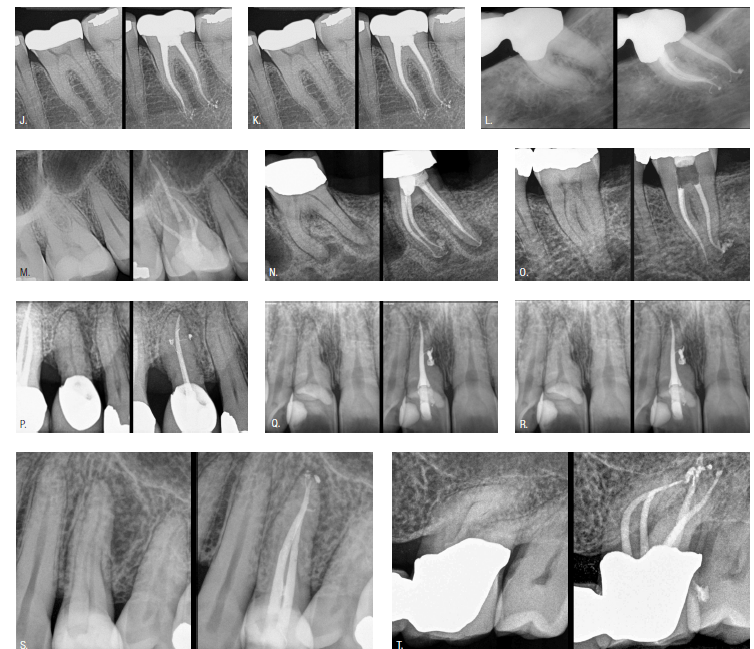
Editor’s intro: By showing readers a visual reference in these case studies, Dr. John West applauds endodontists attention to detail.
Dr. John West offers a quick visual reference guide as a starting point for pretreatment and posttreatment evaluations
”The pulp is a big issue about a little tissue.” This quote is credited to early endodontic educator Dr. Sam Seltzer of Philadelphia.
Nothing has changed.
Restorative dentists have discovered that endodontics is one of the fastest ways to grow their practices, and, therefore, most dentists want to add more endodontic procedures to their schedules. However, as dentists, we are almost all built alike. We also want to do a better job. Our No. 1 desired outcome in clinical dentistry is predictability. I know this because after more than 30 years of clinical teaching, the most frequent question that students ask me is, “Is it predictable?” And the most frequent question that I ask students is, “Is it predictable?” Why do we ask this question? Because our No. 1 focus is our patients. We want to know that we are doing our best for them. So, consequently, dentists who perform endodontics in their practices always want to know what endodontists are doing. They want to compare their best with the level of care that the endodontic specialists are providing. They often bring endodontists their final radiographic images and ask, “What do you think?”
Until 3D endodontic imaging, the only comparison for the restorative dentist’s endodontic result versus the endodontist’s result was a 2D image. At this moment, a facial final image-quality comparison is still the fastest way for a dentist to evaluate how he/she is doing with his/her treatment. The purpose of this article is to offer the restorative dentist a quick radiographic reference guide of radicular endodontic preparation outline and obturation forms. Of course, this comparison does not include details such as access design, the type of 3D cleaning, or obturation technique.
This article represents a quick visual reference guide as a starting point for pretreatment and posttreatment evaluations. While none of the selected respected clinicians used precisely the same treatment protocol (i.e., instruments and technology), this does not matter. The endodontists who were chosen to be showcased in this article are highly trained and skilled. Any of them could prepare the root canal system’s final radicular shapes with literally any modern endodontic tools. They will likely have specific preferences, and most will feel quite strongly about their chosen tools and techniques because, for them, their protocols provide predictability, safety, and ease of delivery. All of us have different skill levels, a unique mix of patients, varied office infrastructure, and a different staff alignment; and we are all at different stages of our endodontic lives, requiring different interests in endodontic procedures. All of these variables make it impossible and inappropriate to actually compare my shape with your shape, but let the conversation begin.
How do endodontists give the restorative dentist helpful and honest answers? To answer this question, we have to look at the back story: the Endodontic Triad and “The Look” of the dentist’s final digital radiograph.
Is the Endodontic Triad dead or alive?
The purpose of endodontics is to prevent or heal lesions of endodontic origin. The rationale of endodontics is that any endodontically diseased tooth can be saved if its root canal system can be cleaned and sealed, either nonsurgically or surgically; if the periodontal condition is healthy or can be made so; and if the tooth is restorable. Recognizing the purpose of endodontics, Schilder1,2 was the first to offer clinical mechanical radicular objectives to make the rationale of endodontics predictable. Previously, the mechanical objectives were essentially described as “instrument and fill.” Schilder consolidated the 5 mechanical objectives into a simple intentional protocol, which most dentists refer to today as cleaning and shaping (more recently, with the acceptance of the NiTi revolution, some endodontists prefer shaping and cleaning). It should be noted that many earlier “instrumented” canals were neither cleaned nor shaped, based upon in vitro examination of extracted endodontic failures.3
Schilder’s 5 mechanical objectives evolved into the Endodontic Triad: clean, shape, and pack.4,5 These time-tested goals remain with the same validity; only the methods have changed. Endodontics has gotten better, safer, and easier, all the while resulting in an increased predictability for the dentist and the patient. Endodontic biology is part of any medical biology. The rules of Mother Nature remain the same: Eliminate the source of a disease, and the disease is gone! The symptoms of the disease also resolve, as symptoms are not sustainable without a cause. Meanwhile, the ravages of a healed disease may remain. While some authors would suggest the Endodontic Triad is no longer valid, the reader should note that, in these recent writings, the clinician(s) still perform the following:
- Make an endodontic access followed by one or more endodontic files
- Perform some form of irrigation cleaning
- Fill the empty anatomy with a sealing material
The only real difference between now versus the past is newer technologies. Examples include the following: the microscope for better vision; digital radiographs for enlarging images for better detail; 3D CBCT to evaluate the root canal system in three dimensions versus two dimensions; NiTi files for increased shaping control, confidence, and consistency; new hopeful technologies to enhance root canal system cleaning; and, finally, improved obturation techniques that better enable filling material to flow into all foramina as well as complex internal anatomy.
In order for a dentist to better understand the desired preparation silhouette or outline form, it is worth revisiting Schilder’s original 5 mechanical objectives for a brief review. Otherwise, how can the endodontist answer the dentist’s question: “How am I doing?”
Schilder’s 5 mechanical objectives
- Continuously taper the funnel shape from the orifice to the physiologic terminus (i.e., cone shape).
- Each cross-sectional diameter becomes narrower from orifice to physiologic terminus (i.e., Schilder refers here to not only the facial view of the final radiograph but also the complete 360° view).
- The root canal preparation is to follow the same multiple planes as the original root canal (i.e., flow).
- Do not transport the foramina internally or externally (i.e., do not block, shelf, tear, or perforate).
- Keep the foramen as small as is practical (i.e., do not intentionally increase the size of the foraminal physiologic constriction).

Mechanical objective No. 4 refers to preserving the position of the original foramina. No. 5 refers to the goal of cleaning to the radiographic terminus in order to stay patent while shaping to, and not intentionally, beyond the physiologic terminus. It is also important to note all foramina are asymmetric to varying degrees. Therefore, if a foramen were determined to be a size No. 20, for example, that diameter is the minimal diameter. The oval dimension (size) may be quite different — for example, a size No. 60 or greater! This is the reason for fully understanding mechanical objective No. 5, which suggests that the funnel shape is, more often than not, an oval or asymmetric apical shape. This knowledge facilitates obturation since the clinician is asking for a round cone of gutta percha to fit into a non-round foramen, and it therefore must be distorted to minimize the gutta-percha/dentin interface.
Newer obturation materials are offering the promise that the gutta-percha cone serves only as a plunger to press nonresorbable material into the body of the root canal system, including the foramina. We just have to wait 5 years to be sure that these newer protocols will deliver what is being claimed.
“The Look”: dead or alive?
“The Look” is far from simply a pretty image of a final radiograph that has visible foramina sealed. Instead, what “The Look” has referred to in modern endodontics is the radiographic achievement of the 5 mechanical objectives for predictable endodontics. That’s it! Because radiographically, “The Look” often reflects a replication of Mother Nature’s complex root canal system’s unique complexities; there was, and is, an element of pride and satisfaction for the clinician when the final image reflects this complex and often unpredictable anatomy. Endodontic clinicians often discover the anatomy when the root canal system is packed. Undiscovered anatomy becomes discovered through the hydraulics of vertical compaction plunger effect! I call this the endodontic seal.

Replicating Mother Nature’s original anatomy has an element of beauty to it, but more importantly, it validates or proves that the dentist has been there physically through finding, following, and finishing each canal within the root canal system.
“The Look” has evolved in recent years with the advent of previously mentioned new technologies that have literally turned the lights on for the endodontic clinician (Figure 1).
“Appropriate”: its role in minimally invasive endodontics
Minimally invasive shapes are not new (Figure 1C). However, in achieving “The Look,” endodontists are not in full agreement about one characteristic, and that is the size of the clinician’s prepared funnel — how wide it is, and how tapered it is. The current trend in endodontics is for narrower shapes. Of course, all dentists and endodontists alike aspire to the concept of minimally invasive endodontics from access to apex. The only difference is really the size of the root with which one begins. It is more accurate for me to refer to minimally appropriate (Figure 2). The guideline is to “connect the dots” from foramen to access orifice. Nature makes root canals anywhere from one-fifth to one-third of the width of the root as it enters the canal orifice. This should also be the clinician’s goal. Then, of course, root canals experience calcific degeneration to varying degrees with age. Some may even appear to fully calcify, but Mother Nature does not do a root canal treatment; and in fact, when calcific degeneration or calcific metamorphosis does occur, it occurs in a crown-down direction. The point here is that, if the clinician’s preparation is no wider than one-fifth to one-third of the width of the root (equivalent to Mother Nature’s natural state), sufficient tooth structure will remain to sustain the tooth for a lifetime, just as Mother Nature intended (Figure 2). The pericervical dentin is protected, and the ferrule must be preserved.
Closing comments
Indeed, “The Look” has radiographic esthetics, but more importantly, it serves as a marker for biologic success. Certainly, a 2D image does not tell the whole story when a restorative dentist asks an endodontist, “Is this a good result?” The vertical extent, the shape of the radicular preparation, the density of the obturation, and the quality of the cleaning of vital or nonvital pulp and bacteria are all unknown variables. The greater variables are perhaps none of these, since the greatest variables of all are the host and host resistance to endodontic disease and the capacity for endodontic success. The threshold of the patient’s required treatment thoroughness to achieve success is unknown. For example, an endodontic obturation halfway down the canal may be successful, while one filled with multiple lateral canals does not. Why? In endodontics, I have estimated thousands of chances each day to make mistakes or successes. Endodontics are truly in the clinician’s hands.
In summary, the final radiograph gives us a glance into reality and suggests our level of attention to detail. And finally, now the restorative dentist can compare his/her final result with the endodontist’s.
Michelangelo said it best: “Trifles are perfection, and perfection is no trifle.”
What is your “Look”?
Editor’s call to action
CBCT offers endodontists an extremely detailed visual reference. Read Dr. West’s article “CBCT 3D imaging: the next endodontic frontier of the great endodontist.”
https://endopracticeus.com/endodontic-insight/cbct-3d-imaging-the-next-endodontic-frontier-of-the-great-endodontist/.
- Schilder H. Cleaning and shaping the root canal. Dent Clin North Am. 1974;18(2):269-296.
- Schilder H. Vertical compaction of warm gutta- percha. In: Gerstein H, ed. Techniques in Clinical Endodontics. Philadelphia, PA: WB Saunders Co; 1982.
- West J. The Incidence of Underfilled Foramina in Endodontic Failures [master’s thesis]. Boston, Massachusetts: Henry M. Goldman School of Dental Medicine; 1974.
- West JD. Endodontic predictability—“Restore or remove: how do I choose?” In: Cohen M, ed. Interdisciplinary Treatment Planning: Principles, Design, Implementation. Hanover Park, IL: Quintessence Publishing; 2008.
- West J, Chivian N, Arens DE, et al. Endodontics and esthetic dentistry. In: Goldstein RE, Chu S, Lee E, et al, (eds.) Esthetics in Dentistry. 3rd ed. Hoboken, NJ: Wiley-Blackwell; 2018.
This article has been reprinted with permission from Dentistry Today.
Stay Relevant With Endodontic Practice US
Join our email list for CE courses and webinars, articles and more..

 John West, DDS, MSD, received his DDS degree from the University of Washington, where he is an affiliate professor. He is the founder and director of the Center for Endodontics in Tacoma, Washington, and a clinical instructor at Boston University, where he earned his MSD degree and was honored with the Distinguished Alumni Award. Dr. West and his two sons, Drs. Jason and Jordan West, are in private endodontic practice in Tacoma. Please contact Dr. West if you have questions to address to any of the contributors. Dr. West can be reached via email at
John West, DDS, MSD, received his DDS degree from the University of Washington, where he is an affiliate professor. He is the founder and director of the Center for Endodontics in Tacoma, Washington, and a clinical instructor at Boston University, where he earned his MSD degree and was honored with the Distinguished Alumni Award. Dr. West and his two sons, Drs. Jason and Jordan West, are in private endodontic practice in Tacoma. Please contact Dr. West if you have questions to address to any of the contributors. Dr. West can be reached via email at 
