CE Expiration Date: March 1, 2028
CEU (Continuing Education Unit):2 Credit(s)
AGD Code: 070
Educational aims and objectives
This self-instructional course for dentists aims to give a general understanding of the various endodontic access cavities, their impact on tooth structure, and the current scientific recommendations.
Expected outcomes
Endodontic Practice US subscribers can answer the CE questions by taking the quiz online to earn 2 hours of CE from reading this article. Correctly answering the questions will demonstrate the reader can:
- Identify the role of endodontic access cavities.
- Identify various access cavity designs.
- Recognize advantages and shortcoming for those various designs.
- Realize the most current scientific recommendations.
Dr. Chafic Safi gives an overview of different types of access cavities and their benefits and drawbacks.
Dr. Chafic Safi discusses how the design of access cavities can affect root canal treatment
Introduction
The prevention and treatment of apical periodontitis has always been paramount for any clinician performing a root canal treatment. By prevention, the clinician aims at stopping an ingress of microbes into the root canal system before affecting the periapical tissues. Once these microbes colonize the root canal system and reach a certain critical concentration, periapical tissues develop a radiolucency, a sign of endodontic disease. The removal of these microbes and lowering their count restores the health of the diseased tissues. In other words, the aim of a root canal treatment is microbial control.1
This control is achieved through a series of steps involving the chemo-mechanical debridement and disinfection of the root canal system. Mechanically, root canal systems are instrumented with files up to a certain diameter.2,3,4 The resulting space is chemically disinfected by the action of irrigation solutions and then filled and sealed using various available techniques.4,5,6 Finally, a proper coronal restoration is placed to ensure a fluid tight seal as well as to consolidate the tooth.7,8 The prognosis of such a goal has been reported to be in the range of 90%-96%. 9,10
In the recent decade, technological advancements have simplified root canal treatments. The advent and accessibility of magnification and illumination, as well as cone beam computed tomography (CBCT), and other techniques made it possible to localize and visualize the pulpal space and canal orifices with more ease. This resulted in a shift in the design of access cavities, going from traditional cavities to less invasive ones such as conservative, ultra conservative (ninja), truss, caries-oriented, and restorative-oriented access cavities.
Endodontic access cavities: the science
The access cavity is the first clinical step in a root canal treatment. Its design and execution can dictate the healing or the persistence of apical periodontitis. The purpose of an access cavity is to offer the clinician a proper entry into the pulpal chamber, the canal orifices, and into the canals all the way to the working length. It should allow the easy way-in and way-out of all the mechanical and chemical armamentarium during a root canal treatment.11
Traditionally, the endodontic access cavity was designed in a way that aimed to remove any obstruction in the way of reaching the canal orifices. This included the complete unroofing of the chamber, exposing all pulp horns, and obtaining a straight-line access to the apex — avoiding the need to alter visual angulation. This design also aimed at reducing the likelihood of iatrogenic errors.
There are various factors that influence the size of such cavities, notably the anatomical location of the orifices and visualizing these orifices without tilting the mirror.12 This results in an access cavity that is widest occlusally and smallest at the level of the orifices.12,13 Hence the drawback of such access cavity design is that it requires the removal of healthy tooth structure, specifically the pericervical dentin — the dentin present 4 mm above and 6 mm below the crestal bone which helps to distribute any forces placed on the tooth (Figure 1).14 This access design, known as Traditional Endodontic Cavity (TEC) is presently being questioned, giving rise to various access designs emphasizing the preservation of this pericervical dentin.14,15
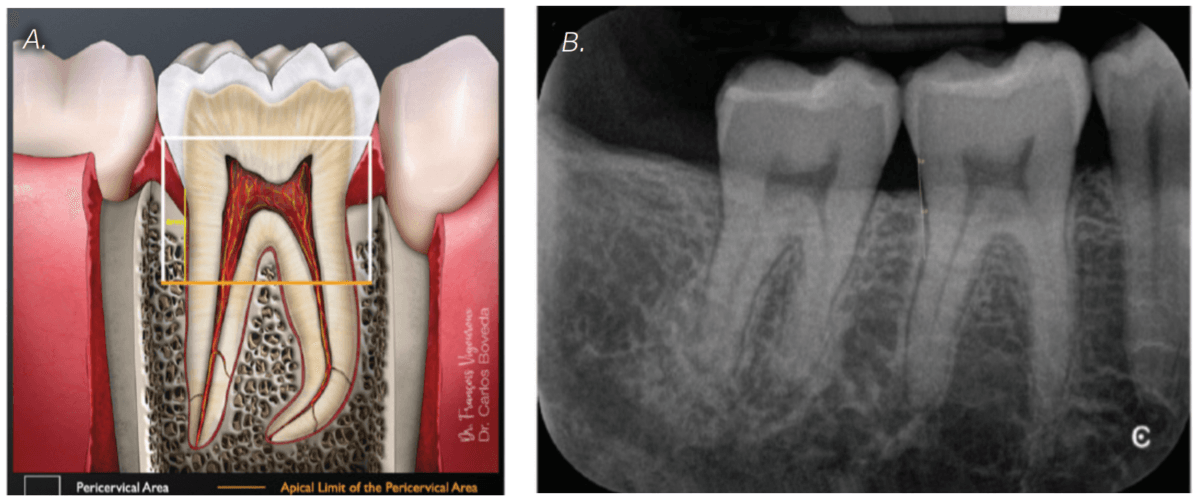
Adapted from Boveda C, Kishen A, Millan B, Camejo MV, Gomez-Sosa JF. Pericervial Dentin Metrics in Mandibular First Molars Determined with Digital Periapical Radiography and Cone-beam Computed Tomography. J Endod. 2024 May;50(5);637-643
Endodontic access cavities: The trends
The increasing popularity of magnification, illumination, and CBCT technology, along with the goal to preserve pericervical dentin, gave rise to a series of new endodontic access cavities. These include conservative, ultra conservative (ninja), truss, guided, caries-oriented, and restorative access cavities.
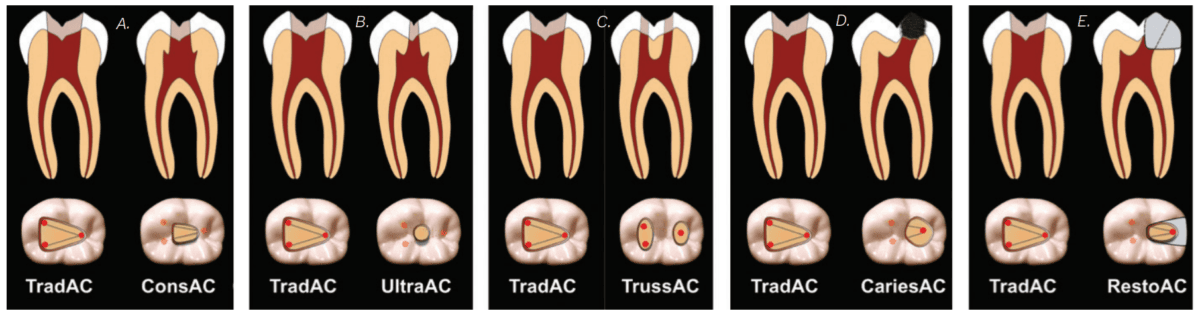
Adapted from Silva EJNL, Pinto KP, Ferreira CM, Belladonna FG, De-Deus G, Dummer PMH, Versiani MA. Current status on minimal access cavity preparations: a critical analysis and a proposal for a universal nomenclature. Int Endod J. 2020 Dec;53(12):1618-1635
Conservative Endodontic Cavity (Figure 2A)
The Conservative Endodontic Cavity (CEC) is a first step towards a less invasive access cavity while executing a root canal treatment. It is based on the partial deroofing of the pulpal chamber while preserving pulpal horns, resulting in a slight occlusal convergence. This elimination of straight-line access makes orifices visible one at a time using different visual angulation.16
It has been shown that CEC might increase the strength of endodontically treated teeth especially in mandibular premolars and molars.17 However, there are concerns about the ability of effective chemo-mechanical debridement and disinfection of the root canal system as well as procedural errors due to reduced direct vision.18
Ultraconservative Endodontic Cavity (Ninja) (Figure 2B)
The Ultraconservative Endodontic Cavity (UEC), also known as Ninja access, is a more minimalistic version of the CEC. It is performed by creating a cavity in the occlusal surface starting from the central fossa or incisal edge and reaching the pulpal floor with an extremely conservative deroofing of the chamber and preservation of the pulp horns. No further extension is made.15 This results in a super convergent cavity and the preservation of not only percervical dentin but also occlusal enamel. This ultraconservative shape makes it more challenging to locate, clean, disinfect, and obturate the root canal system. It also increases the risks of missed canals which can then lead to failure of the treatment. The increased mechanical stability and increased long-term survival claimed to be attributes to such cavity design are limited and debatable.17 There is also increased treatment time to be considered.
Truss Access Cavity (Figure 2C)
In the discussion of smaller access cavities with the aim of preserving pericervical dentin, we include the Truss Access Cavity. This design yields separate access cavities on the occlusal surface, aligned with the corresponding canals, to expose the orifices and leaving the truss of dentin intact in between.19
On mandibular molars, this yields two separate cavities, one mesial and one distal. On maxillary molars, the mesiobuccal and distobuccal orifices are accessed through one opening and the palatal through a separate opening. One of the major challenges of such design is inaccuracy which may lead to perforations and other errors.15
In a study comparing CEC to truss cavities, there was no difference in fracture resistance between the two. Considering the higher risk and difficulty of the truss access, it is advisable to opt for the conservative access.20
There is a major lack of evidence to support the use of truss access cavities and whether they can result in effective tissue cleaning.
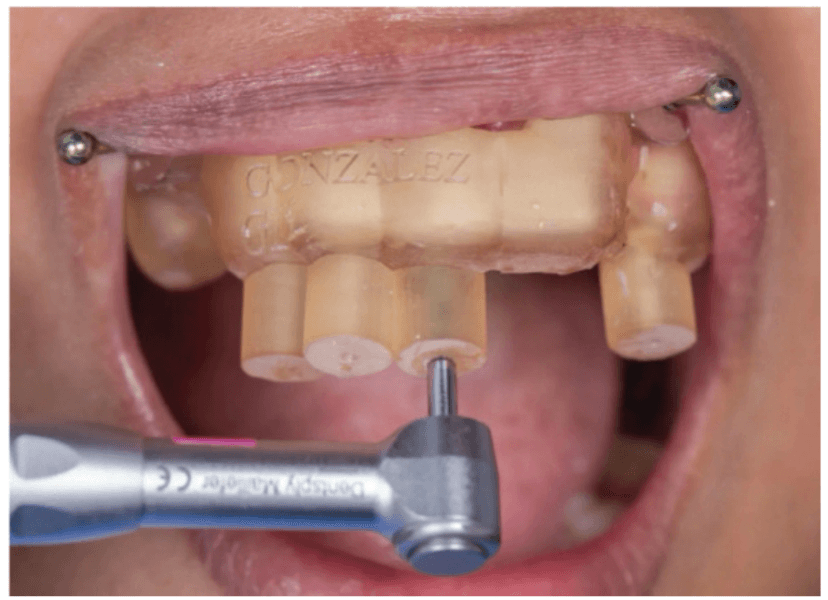
Adapted from Serota K. Dynamic navigation — The future of minimally invasive endodontics. Dental Tribune. March 2020
Guided Access Cavity (Figure 3)
The advancements in CBCT and in imaging software make it possible for a clinician to have an access cavity guide. Similar to a surgical guide in implant dentistry, this access guide/stent is placed in the patient’s mouth and allows for guided dentin removal. This allows the clinician to plan their access cavity in a way that conserves the dentin and saves time. This access cavity design is mainly used in obliterated root canal systems to reduce the risks of canal deviation and perforation. However, the lack of accuracy of the stent as well as its cumbersomeness in posterior regions tend to make this kind of access cavity less popular.15, 21
Caries Oriented and Restorative-Oriented Access Cavity (Figures 2D and 2E)
Remaining in the quest of maximizing tooth structure to reduce post-endodontic fractures, comes the caries and restorative-oriented access cavities. The cavities are done through the caries or through an existing restoration, allowing this to dictate the overall design and preserve sound tooth structure.19 One main disadvantage of these designs is the increased stress and strain on instruments, and hence an increased risk of instrument separation. Due to the restricted access, there is a debate that appropriate chemo-mechanical debridement is compromised, therefore increasing the risk of post treatment disease.15
“The increasing popularity of magnification, illumination, and CBCT technology, along with the goal to preserve pericervical dentin, gave rise to a series of new endodontic access cavities.”
Science versus trends
The transformational shift into more restricted endodontic access cavities with the claim of stronger teeth was investigated by many, especially TEC versus CEC and UEC.
In a study comparing TEC versus CEC and UEC, extracted premolars and molars with TEC showed lower fracture strength than the ones prepared with CEC or UEC. The ultraconservative “ninja” endodontic cavity access did not increase the fracture strength of teeth compared with the ones prepared with CEC.15 It seems consistent in many other studies that UEC does not offer an increased resistance to fracture compared to TEC or CEC. Moreover, there is evidence that UEC makes cleaning procedures more difficult, increasing the total time required for a root canal treatment.20
The effect of CEC is, however, not consistent in the literature, with systematic reviews showing no evidence that supports the use of CEC over TEC for the increase of fracture resistance in human teeth.20,22 It should be mentioned, however, that TEC does sacrifice more percervical dentin, but it is not clear if that can impact the fracture resistance of endodontically treated teeth.
However, not only did many studies’ results show no benefits associated with CECs, but some also present evidence that this access modality resulted in less root canal detection, less preservation of the original canal anatomy particularly at the apical level, and more complications regarding the restoration.16,23,24
As for guided access cavities and caries and restoration-oriented cavities, there are only case reports and case series pertaining to them, hence questioning the validity of their clinical implementation.
Lastly, what seems important in terms of fracture resistance is not the access cavity design but rather the number of walls remaining at time of access. It has been shown that molars with two remaining walls are significantly less resistant to fracture compared to four- and three-walled cavities, regardless of the cavity design.20 This of course, raises the importance of post-endodontic cuspal coverage.
Conclusion
The wave of technological advancements that the field of endodontics has experienced in the last decade has transformed the way a root canal treatment is executed. However, the main purpose remains the same — microbial control. This control relies heavily on the action of chemo-mechanically debriding the root canal system and sealing it afterwards. This in turn relies on having an adequate access cavity opening. The traditional access opening has been redesigned into more restricted preparations with the claim of better preservation of tooth structure. However, at the present time, there is not enough supporting evidence for the incorporation of such cavities into clinical practice, and clinicians must remain cautious and base themselves on current scientific evidence.
Dr. Tony Druttman wrote about access cavities and canal location and how to make preparation of canals easier in his article from our archives that you can access here: https://endopracticeus.com/top-ten-tips-tip-number-5-access-cavities-canal-location/
References
- Bergenholtz G, Hörsted-Bindslev P, Reit C (eds). Textbook of endodontology. Chichester : John Wiley & Sons; 2013.
- Sundqvist G, Figdor, D. Endodontic treatment of apical periodontitis, in Ørstavik, D, Pitt Ford T (eds). Essential Endodontology. Oxford, UK:Blackwell Science Ltd; 1998:242–277.
- Byström A, Sundqvist G. Bacteriologic evaluation of the efficacy of mechanical root canal instrumentation in endodontic therapy. Scand J Dent Res. 1981 Aug;89(4):321-328. doi: 10.1111/j.1600-0722.1981.tb01689.x.
- Shuping GB, Orstavik D, Sigurdsson A, Trope M. Reduction of intracanal bacteria using nickel-titanium rotary instrumentation and various medications. J Endod. 2000 Dec;26(12):751-755. doi: 10.1097/00004770-200012000-00022.
- Byström A, Sundqvist G. The antibacterial action of sodium hypochlorite and EDTA in 60 cases of endodontic therapy. Int Endod J. 1985 Jan;18(1):35-40. doi: 10.1111/j.1365-2591.1985.tb00416.x.
- Byström A, Sundqvist G. Bacteriologic evaluation of the effect of 0.5 percent sodium hypochlorite in endodontic therapy. Oral Surg Oral Med Oral Pathol. 1983 Mar;55(3):307-312. doi: 10.1016/0030-4220(83)90333-x.
- Ray HA, Trope M. Periapical status of endodontically treated teeth in relation to the technical quality of the root filling and the coronal restoration. Int Endod J. 1995 Jan;28(1):12-18. doi: 10.1111/j.1365-2591.1995.tb00150.x.
- Hommez GM, Coppens CR, De Moor RJ. Periapical health related to the quality of coronal restorations and root fillings. Int Endod J. 2002 Aug;35(8):680-689. doi: 10.1046/j.1365-2591.2002.00546.x.
- Sjögren U, Hagglund B, Sundqvist G, Wing K. Factors affecting the long-term results of endodontic treatment. J Endod. 1990 Oct;16(10):498-504. doi: 10.1016/S0099-2399(07)80180-4.
- López-Valverde I, Vignoletti F, Vignoletti G, Martin C, Sanz M. Long-term tooth survival and success following primary root canal treatment: a 5- to 37-year retrospective observation. Clin Oral Investig. 2023 Jun;27(6):3233-3244. doi: 10.1007/s00784-023-04938-y. Epub 2023 Mar 18.
- American Association of Endodontics. Colleagues for Excellence: Access opening and canal location. Spring 2010. https://www.aae.org/specialty/newsletter/access-opening-canal-location/. Accessed January 26, 2025.
- Rankow HJ, Krasner PR. The access box: an ah-ha phenomenon. J Endod. 1995 Apr;21(4):212-214. doi: 10.1016/S0099-2399(06)80569-8.
- Krasner P, Rankow HJ. Anatomy of the pulp-chamber floor. J Endod. 2004 Jan;30(1):5-16. doi: 10.1097/00004770-200401000-00002.
- Clark D, Khademi J. Modern molar endodontic access and directed dentin conservation. Dent Clin North Am. 2010 Apr;54(2):249-273. doi: 10.1016/j.cden.2010.01.001.
- Al-Helou N, Zaki AA, Al Agha M, Moawad E, Jarad F. Which endodontic access cavity is best? A literature review. Br Dent J. 2023 Mar;234(5):335-339. doi: 10.1038/s41415-023-5581-7. Epub 2023 Mar 10.
- Shabbir J, Zehra T, Najmi N, Hasan A, Naz M, Piasecki L, Azim AA. Access Cavity Preparations: Classification and Literature Review of Traditional and Minimally Invasive Endodontic Access Cavity Designs. J Endod. 2021 Aug;47(8):1229-1244. doi: 10.1016/j.joen.2021.05.007. Epub 2021 May 28.
- Plotino G, Grande NM, Isufi A, Ioppolo P, Pedullà E, Bedini R, Gambarini G, Testarelli L. Fracture Strength of Endodontically Treated Teeth with Different Access Cavity Designs. J Endod. 2017 Jun;43(6):995-1000. doi: 10.1016/j.joen.2017.01.022. Epub 2017 Apr 14.
- Krishan R, Paqué F, Ossareh A, Kishen A, Dao T, Friedman S. Impacts of conservative endodontic cavity on root canal instrumentation efficacy and resistance to fracture assessed in incisors, premolars, and molars. J Endod. 2014 Aug;40(8):1160-1166. doi: 10.1016/j.joen.2013.12.012. Epub 2014 Jan 28.
- Silva EJNL, Pinto KP, Ferreira CM, Belladonna FG, De-Deus G, Dummer PMH, Versiani MA. Current status on minimal access cavity preparations: a critical analysis and a proposal for a universal nomenclature. Int Endod J. 2020 Dec;53(12):1618-1635. doi: 10.1111/iej.13391. Epub 2020 Sep 18.
- Corsentino G, Pedullà E, Castelli L, Liguori M, Spicciarelli V, Martignoni M, Ferrari M, Grandini S. Influence of Access Cavity Preparation and Remaining Tooth Substance on Fracture Strength of Endodontically Treated Teeth. J Endod. 2018 Sep;44(9):1416-1421. doi: 10.1016/j.joen.2018.05.012. Epub 2018 Jul 23.
- Connert T, Weiger R, Krastl G. Present status and future directions – Guided endodontics. Int Endod J. 2022 Oct;55 Suppl 4(Suppl 4):995-1002. doi: 10.1111/iej.13687. Epub 2022 Feb 4.
- Ballester B, Giraud T, Ahmed HMA, Nabhan MS, Bukiet F, Guivarc’h M. Current strategies for conservative endodontic access cavity preparation techniques-systematic review, meta-analysis, and decision-making protocol. Clin Oral Investig. 2021 Nov;25(11):6027-6044. doi: 10.1007/s00784-021-04080-7. Epub 2021 Oct 8.
- Rover G, Belladonna FG, Bortoluzzi EA, De-Deus G, Silva EJNL, Teixeira CS. Influence of Access Cavity Design on Root Canal Detection, Instrumentation Efficacy, and Fracture Resistance Assessed in Maxillary Molars. J Endod. 2017 Oct;43(10):1657-1662. doi: 10.1016/j.joen.2017.05.006. Epub 2017 Jul 21.
- Alovisi M, Pasqualini D, Musso E, Bobbio E, Giuliano C, Mancino D, Scotti N, Berutti E. Influence of Contracted Endodontic Access on Root Canal Geometry: An In Vitro Study. J Endod. 2018 Apr;44(4):614-620. doi: 10.1016/j.joen.2017.11.010. Epub 2018 Jan 12.
Stay Relevant With Endodontic Practice US
Join our email list for CE courses and webinars, articles and more..

 Chafic Safi, DMD, completed his postgraduate residency in Endodontics at the University of Pennsylvania in 2015 where he also completed a Master of Science in Oral Biology researching the outcome of endodontic microsurgery and factors affecting prognosis. Dr. Safi is a published researcher and lectures on various endodontic topics nationally and internationally. He is certified by the American Board of Endodontics. Dr. Safi remains on the faculty at the University of Pennsylvania’s department of Endodontics as well as University of Montreal, as an adjunct professor. He is also a faculty lecturer for Next Level Endodontics. He founded Centre Endodontique Saint-Laurent in Montreal, Canada where he lives and practices since 2016.
Chafic Safi, DMD, completed his postgraduate residency in Endodontics at the University of Pennsylvania in 2015 where he also completed a Master of Science in Oral Biology researching the outcome of endodontic microsurgery and factors affecting prognosis. Dr. Safi is a published researcher and lectures on various endodontic topics nationally and internationally. He is certified by the American Board of Endodontics. Dr. Safi remains on the faculty at the University of Pennsylvania’s department of Endodontics as well as University of Montreal, as an adjunct professor. He is also a faculty lecturer for Next Level Endodontics. He founded Centre Endodontique Saint-Laurent in Montreal, Canada where he lives and practices since 2016.